Measures of Adult Pain Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain),
McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ),
Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS),
and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP)
This section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Arthritis Care Res (Hoboken) 2011 (Nov); 63 Suppl 11: S240-252 ~ FULL TEXT
OPEN ACCESS Gillian A. Hawker, Samra Mian, Tetyana Kendzerska, And Melissa French
Women's College Hospital,
University of Toronto,
Toronto, Ontario, Canada.
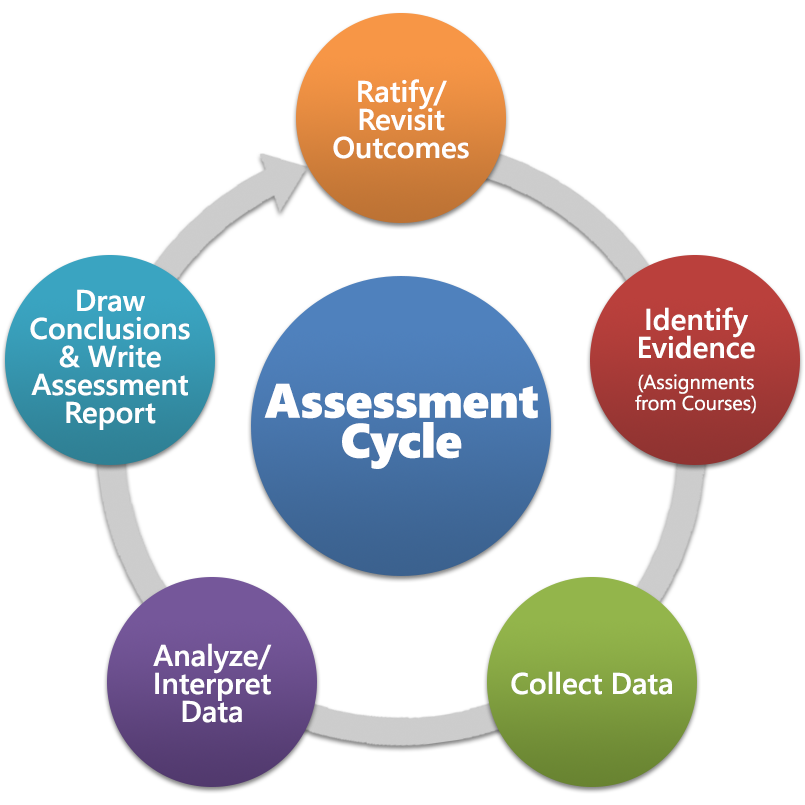
FROM: Learning Outcomes Assessment
From the FULL TEXT Article:
INTRODUCTION
Our purpose is to provide an overview of available generic and rheumatology population–specific questionnaires suitable for evaluating pain in adult rheumatology populations. The content, ease of use, and measurement properties of the questionnaires are presented and compared in order to assist both clinicians and researchers select the questionnaire that is most appropriate for their purpose.
The questionnaires are presented in the following order:generic unidimensional pain questionnaires (Visual Analog Scale and Numeric Rating Scale),
generic multidimensional pain questionnaires (Short-form McGill Pain Questionnaire, Chronic Pain Grade Scale, and Short Form-36 Bodily Pain Scale), and finally
an arthritis-specific pain questionnaire (Measure of Intermittent and Constant Osteoarthritis Pain).Composite measures of arthritis symptoms, including pain and associated disability, specifically the Western Ontario and McMaster Universities Osteoarthritis Index and the Arthritis Impact Measurement Scales, are described in Measures of Knee Function and Measures of Disability, respectively.
Visual Analog Scale (VAS) For Pain
Description
Purpose. The pain VAS is a unidimensional measure of pain intensity [1], which has been widely used in diverse adult populations, including those with rheumatic diseases. [2-5]
Content. The pain VAS is a continuous scale comprised of a horizontal (HVAS) or vertical (VVAS) line, usually 10 centimeters (100 mm) in length, anchored by 2 verbal descriptors, one for each symptom extreme. [2, 6] Instructions, time period for reporting, and verbal descriptor anchors have varied widely in the literature depending on intended use of the scale. [7]
Number of items. The pain VAS is a single-item scale.
Response options/scale. For pain intensity, the scale is most commonly anchored by “no pain” (score of 0) and “pain as bad as it could be” or “worst imaginable pain” (score of 100 [100-mm scale]). [6-8] To avoid clustering of scores around a preferred numeric value, numbers or verbal descriptors at intermediate points are not recommended. [4, 9]
Recall period for items. Varies, but most commonly respondents are asked to report “current” pain intensity or pain intensity “in the last 24 hours.”
Practical Application
How to obtain. The pain VAS is available in the public domain at no cost. [7] Graphic formats for the VAS may be obtained from Scott & Huskisson [9] or online:
http://www.amda.com/tools/library/whitepapers/hospiceinltc/ appendix-a.pdf.
Method of administration. The pain VAS is self-completed by the respondent. The respondent is asked to place a line perpendicular to the VAS line at the point that represents their pain intensity. [2, 9, 10]
Scoring. Using a ruler, the score is determined by measuring the distance (mm) on the 10-cm line between the “no pain” anchor and the patient’s mark, providing a range of scores from 0–100. [6]
Score interpretation. A higher score indicates greater pain intensity. Based on the distribution of pain VAS scores in postsurgical patients (knee replacement, hysterectomy, or laparoscopic myomectomy) who described their postoperative pain intensity as none, mild, moderate, or severe, the following cut points on the pain VAS have been recommended:no pain (0–4 mm),
mild pain (5–44 mm),
moderate pain (45–74 mm), and
severe pain (75–100 mm). [11]Normative values are not available.
Respondent burden. The VAS takes <1 minute to complete. [3, 7]
Administrative burden. The VAS is administered as a paper and pencil measure. As a result, it cannot be administered verbally or by phone. No training is required other than the ability to use a ruler to measure distance to determine a score. [7, 9] Caution is required when photocopying the scale as this may change the length of the 10-cm line. [6] As slightly lower scores have been reported on the HVAS compared to the VVAS [12], the same alignment of scale should be used consistently within the same patient.
Translations/adaptations. Minimal translation difficulties have led to an unknown number of cross-cultural adaptations.
Psychometric Information
Method of development. The pain VAS originated from continuous visual analog scales developed in the field of psychology to measure well-being. [13, 14] Woodforde and Merskey [15] first reported use of the VAS pain scale with the descriptor extremes “no pain at all” , and “my pain is as bad as it could possibly be” in patients with a variety of conditions. Subsequently, others reported use of the scale to measure pain in rheumatology patients receiving pharmacologic pain therapy. [2, 6, 9] While variable anchor pain descriptors have been used, there does not appear to be any rationale for selecting one set of descriptors over another.
Acceptability. The pain VAS requires little training to administer and score and has been found to be acceptable to patients. [2, 10] However, older patients with cognitive impairment may have difficulty understanding and therefore completing the scale. [6, 16] Supervision during completion may minimize these errors. [9]
Reliability. Test–retest reliability has been shown to be good, but higher among literate (r = 0.94, P < 0.001) than illiterate patients (r = 0.71, P < 0.001) before and after attending a rheumatology outpatient clinic. [8]
Validity. In the absence of a gold standard for pain, criterion validity cannot be evaluated. For construct validity, in patients with a variety of rheumatic diseases, the pain VAS has been shown to be highly correlated with a 5-point verbal descriptive scale (“nil,” “mild,” “moderate,” “severe,” and “very severe”) and a numeric rating scale (with response options from “no pain” to “unbearable pain”), with correlations ranging from 0.71–0.78 and 0.62–0.91, respectively). [3] The correlation between vertical and horizontal orientations of the VAS is 0.99. [12]
Ability to detect change. In patients with chronic inflammatory or degenerative joint pain, the pain VAS has demonstrated sensitivity to changes in pain assessed hourly for a maximum of 4 hours and weekly for up to 4 weeks following analgesic therapy (P < 0.001). [10] In patients with rheumatoid arthritis, the minimal clinically significant change has been estimated as 1.1 points on an 11-point scale (or 11 points on a 100-point scale). [17] A minimum clinically important difference of 1.37 cm has been determined for a 10-cm pain VAS in patients with rotator cuff disease evaluated after 6 weeks of nonoperative treatment. [18]
Critical Appraisal of Overall Value to the Rheumatology Community
Strengths/caveats and cautions/clinical and research usability. The VAS is widely used due to its simplicity and adaptability to a broad range of populations and settings. Its acceptability as a generic pain measure was demonstrated in the early 1970s. Limitations to the use of the pain VAS include the following: older patients may have difficulty completing the pain VAS due to cognitive impairments or motor skill issues, scoring is more complicated than that for the Numeric Rating Scale for pain (described below), and it cannot be administered by telephone, limiting its usefulness in research.
Numeric Rating Scale (NRS) For Pain
Description
Purpose. The NRS for pain is a unidimensional measure of pain intensity in adults [19-21], including those with chronic pain due to rheumatic diseases. [3, 8] Although various iterations exist, the most commonly used is the 11-item NRS [22], which is described here.
Content. The NRS is a segmented numeric version of the visual analog scale (VAS) in which a respondent selects a whole number (0–10 integers) that best reflects the intensity of their pain. [21] The common format is a horizontal bar or line. [23] Similar to the pain VAS, the NRS is anchored by terms describing pain severity extremes. [3,20,21]
Number of items. The pain NRS is a single 11-point numeric scale. [3]
Response options/scale. An 11-point numeric scale (NRS 11) with 0 representing one pain extreme (e.g., “no pain”) and 10 representing the other pain extreme (e.g., “pain as bad as you can imagine” and “worst pain imaginable”). [20, 21]
Recall period for items. Varies, but most commonly respondents are asked to report pain intensity “in the last 24 hours” or average pain intensity. [24]
Practical Application
How to obtain. Available from the web site:
http://www.partnersagainstpain.com/printouts/A7012AS2.pdf.
Method of administration. The NRS can be administered verbally (therefore also by telephone) or graphically for self-completion. [6] The respondent is asked to indicate the numeric value on the segmented scale that best describes their pain intensity.
Scoring. The number that the respondent indicates on the scale to rate their pain intensity is recorded. Scores range from 0–10.
Score interpretation. Higher scores indicate greater pain intensity.
Respondent burden. The pain NRS takes <1 minute to complete.
Administrative burden. The pain NRS is easy to administer and score. [6, 25]
Translations/adaptations. Like the pain VAS, minimal language translation difficulties support the use of the NRS across cultures and languages. [26]
Psychometric Information
Method of development. To improve discrimination for detecting relatively small changes, an NRS comprised of numbers along a scale was used in a population of 100 patients with a variety of rheumatic diseases. [3] Variations in pain descriptors used as anchors for end points on the pain NRS have been reported in the literature. [3, 6, 24] However, the methodology used to develop these various anchor terms is unknown.
Acceptability. Chronic pain patients prefer the NRS over other measures of pain intensity, including the pain VAS, due to comprehensibility and ease of completion. [27] However, focus groups of patients with chronic back pain and symptomatic hip and knee osteoarthritis (OA) have found that the pain NRS is inadequate in capturing the complexity and idiosyncratic nature of the pain experience or improvements due to symptom fluctuations. [28, 29]
Reliability. High test–retest reliability has been observed in both literate and illiterate patients with rheumatoid arthritis (r = 0.96 and 0.95, respectively) before and after medical consultation. [8]
Validity. For construct validity, the NRS was shown to be highly correlated to the VAS in patients with rheumatic and other chronic pain conditions (pain >6 months): correlations range from 0.86 to 0.95. [3, 8]
Ability to detect change. In clinical trials of pregabalin for diabetic neuropathy, postherpetic neuralgia, chronic low back pain, fibromyalgia, and OA, analyses of the relationships between changes in pain NRS scores and patient reports of overall improvement, measured using a standard 7-point patient global impression of change, demonstrated a reduction of 2 points, or 30%, on the pain NRS scores to be clinically important. [22] Similar results were found in low back pain patients when changes in pain NRS scores were compared to patient improvements in pain after physical therapy, using a 15-point Global Rating of Change scale. [19]
Critical Appraisal of Overall Value to the Rheumatology Community
Strengths/caveats and cautions/clinical and research usability. The pain NRS is a valid and reliable scale to measure pain intensity. Strengths of this measure over the pain VAS are the ability to be administered both verbally (therefore by telephone) and in writing, as well as its simplicity of scoring. However, similar to the pain VAS, the pain NRS evaluates only 1 component of the pain experience, pain intensity, and therefore does not capture the complexity and idiosyncratic nature of the pain experience or improvements due to symptom fluctuations.
McGill Pain Questionnaire (MPQ)
Description
Purpose. A multidimensional pain questionnaire designed to measure the sensory, affective and evaluative aspects of pain and pain intensity in adults with chronic pain, including pain due to rheumatic diseases. [30, 31]
Content. The scale contains 4 subscales evaluating the sensory, affective and evaluative, and miscellaneous aspects of pain, responses to which comprise the Pain Rating Index, and a 5-point pain intensity scale (Present Pain Intensity).
Number of items. The Pain Rating Index contains 78 pain descriptor items categorized into 20 subclasses, each containing 2–6 words that fall into 4 major subscales:sensory (subclasses 1–10),
affective (subclasses 11–15),
evaluative (subclass 16), and
miscellaneous (subclasses 17–20).There is also a 1-item pain intensity scale. [30]
Response options/scale. The value (score) associated with each descriptor is based on its position or rank order within the word set. The Present Pain Intensity scale, a measure of the magnitude of pain experienced by an individual, is a numeric-verbal combination that indicates overall pain intensity [31] and includes 6 levels:none (0),
mild (1),
discomforting (2),
distressing (3),
horrible (4), and
excruciating (5) (32).Recall period for items. Present pain. [31]
Examples of use. The MPQ can be used to evaluate the efficacy and effectiveness of pain interventions and to identify qualities of pain associated with distinct nocioceptive disorders and neuropathic pain disorders, including arthritis. [30]
Practical Application
How to obtain. The MPQ is available at no cost from the developer, Ronald Melzack, PhD, Department of Psychology, McGill University, 1205 Dr. Penfield Avenue, Montreal, Quebec H3A 1B1, Canada, and online (http://www.qolid.org) by paying a membership fee.
Method of administration. The MPQ is interviewer-administrated using paper and pencil. The interviewer must read instructions to the respondent and define any words that the respondent does not understand. For each subclass of words, the respondent is instructed to select 1 word that fits their present pain. If none of the words describe their pain, then no word is selected. [30, 33]
Scoring. The MPQ is scored by hand by first counting the number of words selected to obtain a Number of Words Chosen score (0–20 words). Pain Rating Index scores range from 0–78 based on the rank values of the chosen words. The value (score) associated with each descriptor is based on its position or rank order in the word set, such that the first word is given a value of 1, the next a value of 2 and so on. Rank values are summed within each subclass as well as overall. Scores on the Present Pain Intensity scale range from 0–5. [31]
Score interpretation. A higher score on the MPQ indicates worse pain. The Pain Rating Index is interpreted both in terms of quantity of pain, as evidenced by the number of words used and the rank values of the words, as well as the quality of pain, as evidenced by the particular words that are chosen. The normative mean scores across painful conditions ranged from 24–50% of the maximum score. [7]
Respondent burden. Completion of the MPQ can take up to 20 minutes. [3]
Administrative burden. No training is required to score and interpret the MPQ, other than the ability of the interviewer to define each word. [30, 33] Time to score is 2–5 minutes.
Translations/adaptations. There are a total of 44 different versions of the MPQ, representing 26 different languages/cultures. [34] The MPQ has been translated into English, French [35], German [36-38], Norwegian [36], Danish [40], Italian [41], Japanese [42], Finnish [43], Spanish [44], Chinese [45], Dutch [46], Amharic [47], Slovak [48], Turkish [49], and Portuguese. [50-52]
Psychometric Information
Method of development. Pain descriptors were derived from recording the words used by chronic pain patients to describe their pain; these descriptors were then categorized into subclasses and rank ordered by intensity using a numerical scale by groups of physicians, patients, and students. [31, 53]
Acceptability. Some respondents have difficulty with the complexity of the vocabulary used, resulting in failure to read the instructions carefully and to see essential features. [54]
Reliability. In a study of general rheumatology clinic patients, test–retest reliability for the 3 MPQ pain items (“nagging,” “aching,” and “stabbing”) ranged from a high of 0.81 for 1-day recall to a low of 0.59 for 7-day recall. [55] These findings are consistent with those of other studies evaluating test–retest reliability in populations with a variety of other conditions including arthritis and other musculoskeletal conditions (r = >0.70). [31, 56, 57]
Validity. Content validity. Arthritis patients, regardless of their disease severity, used similar words to describe the sensory aspects of their pain. MPQ words have been shown to differentiate between 4 different circumstances of rheumatoid arthritis (RA) pain (i.e., overall pain at rest, overall pain on movement, joint pain at rest, and joint pain on movement). [58] The MPQ has the ability to detect mild pain due to the multidimensional nature of the scale and the large number of pain descriptor options. [59]
Construct validity. In RA, the number of sensory and affective MPQ words selected has been positively correlated with visual analog scale (VAS) scores of severity of pain at rest and on movement (r = 0.27, P < 0.01 and r = 0.17, P < 0.05, respectively). [58] Higher Pain Rating Index scores are associated with negative affect (e.g., Minnesota Multiphasic Personality Inventory, Pain Catastrophizing Scale). [60] In knee pain or knee osteoarthritis patients, higher MPQ scores were associated with greater anxiety and depression (r = 0.30, P < 0.05 and r = 0.31, P < 0.05, respectively) [60], and greater symptoms and disability using the Western Ontario and McMaster Universities pain scale (r = 0.34–0.38). [61]
Ability to detect change. In clinical trials designed to evaluate the efficacy of different pain therapies on postoperative pain after general surgical and orthopedic procedures, the relative effect sizes for the MPQ-Pain Rating Index compared with a 4-point categorical verbal rating scale and a pain VAS were 1.08 (moderate) and 1.12 (good), respectively. [62]
Critical Appraisal of Overall Value to the Rheumatology Community
Strengths/caveats and cautions/clinical and research usability. The MPQ is a valid and reliable tool that evaluates both the quality and quantity of pain through use of unique pain descriptors. This may be useful in epidemiologic studies and clinical trials of older patients with multimorbidity, in whom pain may arise from multiple causes. Specifically, use of the MPQ may help to identify neuropathic type pain from nocioceptive type pain. A limitation of the MPQ is the rich vocabulary required of respondents for completion. Further, sex and ethnic differences may affect selection of pain descriptors. However, the interviewer can facilitate MPQ completion by providing respondents
Short-Form McGill Pain Questionnaire (SF-MPQ)
Description
Purpose. The SF-MPQ, a shorter version of the MPQ, is a multidimensional measure of perceived pain in adults with chronic pain, including pain due to rheumatic diseases. [30, 33]
Content. The SF-MPQ is comprised of 15 words (11 sensory and 4 affective) from the original MPQ. [66]
Number of items. The Pain Rating Index is comprised of 2 subscales: 1) sensory subscale with 11 words or items and 2) affective subscale with 4 words or items, which are rated on an intensity scale as 0 = none, 1 = mild, 2 = moderate, or 3 = severe. The SF-MPQ also includes 1 item for present pain intensity and 1 item for a 10-cm visual analog scale (VAS) for average pain (33).
Recall period for items. Present time.
Examples of use. To discriminate among different pain syndromes [33, 63, 64] and evaluate the responsiveness of different symptoms to treatment. [65, 66]
Practical Application
How to obtain. See this section for the MPQ above.
Method of administration. See this section for the MPQ above.
Scoring. For the Pain Rating Index, each selected word is scored from 0 (none) to 3 (severe). The total Pain Rating Index score is obtained by summing the item scores (range 0–45). Scores on the Present Pain Intensity range from 0–5 and on the VAS from 0–10.
Score interpretation. There are no established critical cut points. As for the MPQ, a higher score indicates worse pain.
Respondent burden. The SF-MPQ takes ~ 2–5 minutes to complete. [33]
Administrative burden. No training is required to score and interpret the SF-MPQ other than the ability of the interviewer to define each word. [33] Time to score is ~ 1 minute.
Translations/adaptations. The SF-MPQ has been translated into the following languages: English, French, Amharic [47], Chinese [67], Czech [68], Danish [69], Farsi [70], Greek [71, 72], Hebrew [73], Hindi [74], Korean [75, 76], Norwegian [77], Swedish [78], Thai [79], and Turkish. [49, 80]
Psychometric Information
Method of development. In addition to indices of overall pain intensity (the Present Pain Intensity [31] and VAS [81]), a selection of pain descriptors representing sensory and affective categories were retained from the original version of the MPQ. [31] Other than for one descriptor (“splitting”), those selected for inclusion in the SF-MPQ were those chosen by greater than one-third of patients with various types of pain). [31, 82–84]
Acceptability. Standardized instructions for patient completion have not been published. Some difficulties with completion have been reported and attributed to unfamiliar descriptors and unclear written instructions. However, experience in completing the SF-MPQ and verbal instructions improved completion among osteoarthritis (OA) patients. [85]
Reliability. For internal consistency, using the SF-MPQ in rheumatoid arthritis (RA) and fibromyalgia patients, Cronbach’s alphas were estimated at α 0.73–0.89. [78] In the same study [78], test–retest reliability ranged from 0.45–0.73 for 1-month and 3-month intervals. Among rheumatology patients, test–retest reliability was 0.79–0.93 at intervals of 1 to 3 days. [86] In an OA population, high intraclass correlations were demonstrated for the total, sensory, affective, and average pain scores (5-day period): 0.96, 0.95, 0.88, and 0.89, respectively. [85]
Validity. The SF-MPQ was found to have more content validity among patients with fibromyalgia than for those with RA. Percentage of use of 15 pain descriptors by 2 groups was significantly different for all words except “throbbing” and “punishing-cruel.” The mean intensity score for each word ranged from 1.69 for “sickening” to 2.60 for “tender” in the fibromyalgia group and 1.57 for “fearful” to 2.18 for “aching” in the RA group. [78] For construct validity, the SF-MPQ was found to be moderately correlated with both the Western and Ontario and McMaster Universities Osteoarthritis Index and the Short Form 36 Health Survey bodily pain scales (r = 0.36 and –0.36, respectively; P < 0.01) in 200 patients with hip and knee OA. [61]
Ability to detect change. Although designed for descriptive purposes, the SF-MPQ has been found to be sensitive to the effects of pain therapies in a variety of population settings. [86 88] In patients with a range of musculoskeletal conditions reporting improvements in pain after rehabilitation and surgical interventions, the Norwegian SF (NSF)-MPQ scores were found to be responsive to change (standardized response mean values >0.80): a mean improvement in NSF-MPQ total scores >5 on the 0–45 scale demonstrated a clinically important change. [86] In an OA population, the minimum detectable change for total, sensory, affective, average, and current pain components have been estimated as 5.2, 4.5, 2.8, 1.4, and 1.4 cm, respectively. [85]
Critical Appraisal of Overall Value to the Rheumatology Community.
Strengths/caveats and cautions/clinical and research usability. The SF-MPQ is easier to use and takes less time to administer and complete than the longer form. The word choices are not as complex, and the intensity ranking of mild, moderate, and severe is better understood by patients. [33] However, sufficient experience is required to adequately complete the SF-MPQ; therefore, new users require supervision during completion. [85] In 2009, the short form was further revised for use in neuropathic and nonneuropathic pain conditions (SF-MPQ-2). The SF-MPQ-2 includes 7 additional symptoms relevant to neuropathic pain, for a total of 22 items with 0–10 numerical response options. [89] We await further psychometric testing of this revised measure, which may play a useful role in the future with respect to identifying rheumatic disease patients with neuropathic versus nociceptive pain patterns.
Chronic Pain Grade Scale (CPGS)
Description
Purpose. The CPGS is a multidimensional measure that assesses 2 dimensions of overall chronic pain severity: pain intensity and pain-related disability. It is suitable for use in all chronic pain conditions, including chronic musculoskeletal (MSK) and low back pain. [90]
Content. Subscale scores for pain intensity and disability are combined to calculate a chronic pain grade that enables classification of chronic pain patients into 5 hierarchical categories: grades 0 (no pain) to IV (high disability-severely limiting). [90]
Number of items. The CPGS is comprised of 7 items.
Response options/scale. All items are scored on an 11-point Likert scale, with responses ranging from 0–10.
Recall period for items. Pain in the past 3–6 months.
Examples of use. The CPGS has been used in epidemiologic studies and clinical trials to evaluate and compare pain severity across groups and in response to treatment effects, and in clinical practice to improve the prognostic judgments of physicians. [91-93]
Practical Application
How to obtain. Please note that the scale is available in the original reference [90], as well as directly from the author.
Method of administration. The CPGS is an interview-administered questionnaire that can also be self-completed by respondents. Scoring. Scores are calculated for 3 subscales: the characteristic pain intensity score, which ranges from 0–100, is calculated as the mean intensity ratings for reported current, worst, and average pain; the disability score, which ranges from 0–100, is calculated as the mean rating for difficulty performing daily, social, and work activities; and the disability points score, which ranges from 0–3, is derived from a combination of ranked categories of number of disability days and disability score.
Score interpretation. The 3 subscale scores (characteristic pain intensity, disability score, and the disability points score) are used to classify subjects into 1 of the 5 pain severity grades: grade 0 for no pain, grade I for low disability-low intensity, grade II for low disability-high intensity, grade III for high disability-moderately limiting, and grade IV for high disability-severely limiting.
Respondent burden. Time to complete the CPGS does not exceed 10 minutes.
Administrative burden. The CPGS is easy to administer. Scoring is complex.
Translations/adaptations. The CPGS has been adapted into UK English. [94] An Italian version has been developed to evaluate severity in chronic pain patients. [95]
Psychometric Information
Method of development. Interviews were conducted with primary care patients with back pain, headache, and temporomandibular disorder. [96] The development of the graded classification drew on concepts by Turk and Rudy of chronic pain severity. [97, 98] Two of the items used in the disability score were adapted from their Multidimensional Pain Inventory. [99] The Guttman scaling method was used to develop the graded classification of chronic pain. [90]
Acceptability. The CPGS is easy to understand and complete based on a high response rate (76.3%) to a postal survey sent to general practice patients in the UK. [94] Among MSK chronic pain patients, missing values were only noted in < 3% of each of the questions in an Italian version of the CPGS. [100]
Reliability. For internal consistency, Cronbach’s alpha was shown to be α = 0.74 among patients with chronic back pain. [90] In an Italian version of CPGS, Cronbach’s alpha ranged from 0.81–0.89 for subscales and global scores in patients with chronic MSK pain. [95] In UK general practice patients with low back pain, test–retest reliability was high after a 2-week interval (weighted 0.81 [95% confidence interval 0.65–0.98]). [101]
Validity. For construct validity, cross-sectional and longitudinal studies of general practice patients have shown that higher scores on the CPGS, indicating greater chronic pain, are significantly associated with higher rates of unemployment, greater pain impact scale scores, greater use of opioid analgesics and physician visits, depressed mood, and lower self-rated health status. [90, 94, 102] Comparisons of CPGS scores with the Short Form 36 Health Survey (SF-36) indicate that a higher chronic pain grade using the CPGS is associated with poorer physical, psychological, social, and general health as measured by the SF-36 (P = 0.001) [102] and worse scores on the SF-36 bodily pain scale (ρ = –0.545, P < 0.0001). [95] Spearman’s correlation coefficients for the CPGS scores and the various dimensions of SF-36 were highest for the pain dimension (r = –0.71 to –0.84) and lowest for the mental health dimension (r = –0.28 to –0.38). [94]
Ability to detect change. Among patients with moderate to severe chronic MSK pain, the CPGS has been shown to be modestly responsive to changes after 12 months of treatment with an efficacious pain intervention, with standardized effect sizes for the intensity and disability subscales of 0.41 and 0.43, respectively. Among participants with chronic knee or hip pain, the standardized effect size for the CPGS intensity was 0.32. [91]
Critical Appraisal of Overall Value to the Rheumatology Community
Strengths/caveats and cautions/clinical and research usability. The CPGS is a valid and reliable tool that is useful for the evaluation of chronic MSK pain; it allows for grading of the global severity of chronic pain and therefore analysis of the qualitative changes in chronic pain over time. Further, the CPGS assesses not only aspects of the pain itself, but also the impact of the pain on daily, social, and work activities, which is a significant advantage over many other pain questionnaires. A limitation of the CPGS relative to the other scales reported here is the complexity of scoring, which renders it less useful for assessment of pain at point of care. Additionally, further research is needed to be able to compare scoring methods and cut points.
Short Form 36 Bodily Pain Scale (SF-36 BPS)
Description
Purpose. The SF-36 BPS is 1 of 8 subscales of the Medical Outcomes Study SF-36 questionnaire [103, 104], a generic measure of health status designed for use in population surveys. [105] In 1996, version 2.0 of the SF-36 (SF-36v2) was introduced to correct deficiencies identified in the original version, SF-36v1. [106] The 2-item SF-36 BPS subscale assesses bodily pain as a dimension of health status. [104, 105]
Content. The SF-36 BPS assesses bodily pain intensity and interference of pain with normal activities.
Number of items. The SF-36 BPS is a 2-item scale.
Response options/scale. Intensity of bodily pain is evaluated using a 6-point rating scale of “none” to “very severe.” The extent to which pain has interfered with work is evaluated on a 5-point rating scale from “not at all” to “extremely.”
Recall period for items. The SF-36 BPS is available in both standard (4 week) and acute (1 week) recall versions. [105, 106]
Examples of use. The SF-36 and its subscales, including the BPS, have been used in epidemiologic studies to compare health status across populations and within population subgroups, such as in estimating the relative burden of different diseases, including rheumatic diseases [107], and differentiating the health benefits of different treatments. [108]
Practical Application
How to obtain. The SF-36 and its various versions have been developed by the Rand Corporation and John E. Ware (SF-36 Health Survey, The Health Institute, New England Medical Center Hospitals, Box 345, 750 Washington Street, Boston, MA, 02111). The Medical Outcomes Trust, Health Assessment Lab, and Quality Metric Incorporated are cocopyright holders of all SF-36 and SF-12 surveys. All SF-36 survey instruments, scoring manuals, and licenses for use are available from QualityMetric at www.quality metric.com. Different charges are levied for academic and commercial use.
Method of administration. The SF-36 BPS is suitable for self-administration, computerized administration, or administration by a trained interviewer in person or by telephone. Telephone voice recognition interactive systems and online administrations are currently being evaluated.
Scoring. Responses for each of the 2 SF-36 BPS items are recoded into final item values. [109] The raw scale score is computed as a simple algebraic sum of the recoded item values. The raw scale score is then transformed to a 0–100 scale. Norm-based scores may be calculated for SF-36v2 by including population normative data in the scoring algorithms. The BPS score is only calculated if both items are completed.
Score interpretation. SF-36v1 BPS scores range from 0–100. A higher score indicates lack of bodily pain. SF-36v2 uses norm-based scoring, where 50 is the “average” for the population. Therefore, scores above or below 50 can be considered above or below, respectively, the population average health status for bodily pain, and scores can be interpreted based on deviance from the mean (10 points = 1 SD). Population normative data are available for the US and UK.
Respondent burden. The BPS takes <2 minutes to complete.
Administrative burden. Training to administer, score, and interpret is minimal. Administration guidelines are specific and clearly outlined.
Translations/adaptations. SF-36 has been translated and adapted for use in more than 50 countries as part of the International Quality of Life Assessment (IQOLA) Project. Currently, published forms include the German [110], Spanish [111], Swedish [112], and Italian [113] translations and English-language adaptations for use in Australia/New Zealand, Canada, and the UK. Information about translations is available from the IQOLA Program of the Health Assessment Lab in Boston, Massachusetts (http://www.iqola.org).
Psychometric Information
Method of development. The Medical Outcomes Study researchers selected and adapted questionnaire items from instruments in use since the 1970s and 1980s [114-117] to develop a new 149-item Functioning and Well-Being Profile. Items were subsequently reduced and improvements were made in item wording, format, and scoring to produce the SF-36. One item on pain intensity was retained from an earlier version of the SF-20 question regarding bodily pain or discomfort. In order to improve prediction of best total scores for the Behavioural Effects of Pain Scale in the Medical Outcomes Study [114], a second item was added to measure the extent to which pain interferes in activities. [105]
Acceptability. Generally easy to administer and complete. [103, 118]
Reliability. For internal consistency, Cronbach’s α for the SF-36 BPS administered in hip [118] and knee [119] osteoarthritis (OA) patients was 0.72 and 0.77, respectively; using a Chinese version of the SF-36 BPS in rheumatoid arthritis (RA) patients, Cronbach’s α was 0.91. [120] In adults with persistent back, hip, or knee pain recruited from primary care, Cronbach’s α was 0.59. [100] Among patients from 2 general practices in the UK, the test–retest reliability over a 2-week period was 0.78. [121] Over a 14-day interval, test–retest reliability of a Chinese SF-36 version used in Chinese-speaking RA patients was 0.82. [120]
Validity. Regarding face and content validity, items were derived from pre-existing questionnaires used in large population studies. However, both floor and ceiling effects have been reported. [118] Regarding construct validity, the proportions reporting no pain on the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and the SF-36 BPS were 32.2% and 13.6%, respectively, and pain scores were modestly correlated (–0.55) [122] among patients who had undergone joint replacement surgery. In the same study, the WOMAC better discriminated subjects with varying severity of knee problems, whereas the SF-36 BPS better discriminated subjects with varying levels of self-reported health status and comorbidity. In patients with hip and knee OA, correlations between the WOMAC pain scale and the SF-36 BPS are in the range of 0.6–0.7. [61, 121, 123] In Chinese-speaking patients with RA, moderate correlations were reported between the Chinese SF-36 BPS and physician global assessment of disease activity (r = –0.34), physician’s assessment of global disease activity (r = –0.35), and patient pain assessment based on a pain visual analog scale (r = –0.48). [120]
Ability to detect change. Although the SF-BPS is designed to measure the health status of populations, it has been shown to be responsive to improvements in pain. Among patients undergoing knee replacement surgery, the estimated minimum clinically important difference (MCID) ranged from 16.86/100 (SD 31.83) at 6 months to 6.69/100 (SD 29.20) at 2 years. [119] In a similar study on hip replacement, the estimated MCID ranged from 14.67/100 (SD 26.46) to 18.34/100 (SD 27.06) at 6 months and 2 years, respectively. [118] The minimal detectable change for the SF-36 BPS ranged from 37.91/100 (knee OA) to 38.09/100 (hip OA) at 6 months. [118, 119]
Critical Appraisal of Overall Value to the Rheumatology Community
Strengths/caveats and cautions/clinical and research usability. The SF-36 BPS is a valid and reliable generic questionnaire designed to evaluate bodily pain as a dimension of overall health status and has been widely used internationally and in diverse populations. Its advantages include simplicity of administration and usefulness in making comparisons across populations for research purposes. At point of patient care, a disease-specific pain measure may be more useful to discriminate levels of pain severity, and therefore response to treatment.
Measure Of Intermittent And Constant Osteoarthritis Pain (ICOAP)
Description
Purpose. The ICOAP measure is a multidimensional osteoarthritis (OA)-specific measure designed to comprehensively evaluate the pain experience in people with hip or knee OA, including pain intensity, frequency, and impact on mood, sleep, and quality of life, independent of the effect of pain on physical function. [28] It is intended for use alongside a measure of physical disability. Content. The ICOAP is an 11-item scale evaluating 2 pain domains: a 5-item scale evaluates constant pain and a 6-item scale evaluates intermittent pain or “pain that comes and goes”. [28] Two supplementary questions can be used to assess predictability of intermittent pain when present. [124] Both a hip and knee joint version of the ICOAP are available. [28]
Number of items: 11 items in 2 domains with 2 supplementary items on intermittent pain predictability.
Response options/scale. All items are constructed as rating scales with 5 levels of response. For items asking about intensity, response options are “not at all,” “mildly,” “moderately,” “severely,” and “extremely.” For items about frequency, response options are “never,” “rarely,” “sometimes,” “often,” and “very often”. [28] For the supplementary items asking about predictability of pain, the response options are “never,” “rarely,” “sometimes,” “often,” and “very often”. [124]
Recall period for items. Past week.
Endorsements. Osteoarthritis Research Society International (OARSI)/Outcome Measures in Rheumatology (OMERACT) Initiative.
Practical Application
How to obtain. The ICOAP and ICOAP Users Guide can be obtained free of charge from the OARSI web site, www.oarsi.org.
Method of administration. The measure can be interviewer- administered in person or by telephone. [28] Respondents should complete both subscales. [63] Scoring. Each ICOAP item is scored from 0–4. A score is separately produced for each subscale by summing the items’ subscale scores and then normalizing each score from 0 (no pain) to 100 (extreme pain). A total ICOAP score can be calculated by summing the 2 subscale scores, and normalizing from 0 (no pain) to 100 (extreme pain). Rules have been created to deal with missing data. [63] No scoring guidelines are available for the 2 supplementary items.
Score interpretation. Higher scores indicate a worse pain experience.
Respondent burden. The ICOAP takes < 10 minutes to complete.
Administrative burden. Easy to administer and score.
Translations/adaptations. To date, the ICOAP has been translated into the following languages: English (North America and UK), Czech, Dutch, French (France), German [125], Italian, Norwegian, Spanish (Castillan), North and Central American Spanish, Swedish, Portuguese [50], Greek, Romanian, and Russian. [126] Translated versions are available at www.oarsi.org.
Psychometric Information
Method of development. Focus groups were conducted in individuals with painful hip or knee OA in 4 countries (US, UK, Canada, and Australia) to generate items pertaining to the OA pain experience. [28, 127] Content analysis of resulting transcripts was used to identify themes, which were verified with participants. Subsequent psychometric testing was conducted in subjects age ≥ 40 years with hip or knee OA drawn from rheumatologists’ practices, joint replacement wait lists, and from among the members of an existing OA cohort. [28]
Acceptability. The ICOAP has been shown to be easy to understand and complete; subjects felt positive about the inclusion of the 2 distinct pain domains (constant pain and pain that comes and goes). [126]
Reliability. Regarding content validity, Cronbach’s α was 0.93 [28] for 100 individuals with hip and knee OA. Test–retest reliability in 76 individuals with hip and knee OA, age ≥ 40 years, demonstrated an intraclass correlation coefficient of 0.85 (95% confidence interval 0.76–0.91). [122]
Validity. Content and face validity were determined through focus groups used to develop the ICOAP. For construct validity, descriptive analyses of items demonstrated good distribution of response options across all items. [28] Total and subscale ICOAP scores are significantly correlated with scores on the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain scale, the Knee Injury and OA Outcome Score (KOOS) symptoms scale, and self-rated effect of hip/knee problems on quality of life, with Spearman’s correlation coefficients ranging in magnitude from 0.60 (KOOS symptoms) to 0.81 (WOMAC pain scale). [28]
Ability to detect change. The ICOAP has been found to be responsive to changes in OA pain in response to pharmacologic interventions [128] and joint replacement surgery. [129] For the knee, standard response means (SRMs) ranged from 0.49–0.57 for the ICOAP intermittent, constant, and total scores comparable to that for the WOMAC pain (SRM 0.54). For the hip, SRMs ranged from 0.11– 0.19, again comparable to that for the WOMAC (SRM 0.15). [128] The ICOAP detected large improvements in pain resulting from joint replacement surgery with SRMs (0.84–1.02 for knee replacement and 1.50–2.29 for hip replacement). [129]
Critical Appraisal of Overall Value to the Rheumatology Community
Strengths/caveats and cautions/clinical and research usability. The ICOAP is a valid and reliable measure that is unique in that it is intended to evaluate the multidimensional pain experience in OA, distinct from the impact of pain on physical functioning. Prior experience with the WOMAC, the most commonly used OA measure, has shown high correlations between the pain and physical function subscales. As a result, evaluation of OA pain using the WOMAC is confounded by physical disability. The ICOAP is intended for use together with a measure of OA disability. Although the ICOAP has been translated from English into a number of languages, only a few have been evaluated for validity, reliability, and responsiveness.
DISCUSSION
There are multiple measures available to assess pain in adult rheumatology populations. Each measure has its own strengths and weaknesses. Both the Visual Analog Scale for Pain and the Numeric Rating Scale (NRS) for Pain are unidimensional single-item scales that provide an estimate of patients’ pain intensity. They are easy to administer, complete, and score. Of the 2, the pain NRS may be preferred at point of patient care due to simpler scoring.
In research, the pain NRS may similarly be preferred due to its ability to be administered both verbally and in writing. However, neither measure provides a comprehensive evaluation of pain in patients with rheumatic disease. To evaluate the multiple dimensions of acute and chronic pain, a number of valid and reliable questionnaires are available.
The McGill Pain Questionnaire (MPQ) is a generic pain measure useful largely for research purposes to describe not only the quantity (intensity), but also the quality of the patients’ pain.
The Chronic Pain Grade Scale (CPGS) is similarly a generic pain measure useful for research purposes to describe, evaluate and compare chronic pain severity (its intensity and impact) across groups and in response to treatment effects.
The third generic multidimensional pain measure, the Short Form-36 Bodily Pain Scale (SF-36 BPS), is useful in evaluating pain in the context of overall health status, and therefore most suitable for use in making comparisons across populations and between subgroups within populations. Unlike the MPQ and CPGS, the SF-36 BPS is simple enough for use at point of care.
Finally, the Measure of Intermittent and Constant Osteoarthritis Pain is an osteoarthritis-specific pain measure that is recommended for descriptive and evaluative purposes in both clinical practice and research to provide a comprehensive evaluation of the pain experience in osteoarthritis, including the impact of pain on mood, sleep and quality of life, separate and distinct from the impact of pain on functioning.
Due to the variability in purpose, content, method of administration, respondent and administrative burden, and evidence to support the psychometric properties of each measure, no one pain measure can be recommended for use in all situations. We encourage clinicians and researchers to use this information presented in this chapter to help guide the selection of the questionnaire that is most appropriate for their specific purpose.
Author Contributions
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published.
Additional Tables
Refer to Full-Text for
Summary Table for Adult Pain Measures* tables on p. S251-252
References:
McCormack HM, Horne DJ, Sheather S.
Clinical applications of visual analogue scales: a critical review.
Psychol Med 1988;18:1007–19.Huskisson EC.
Measurement of pain.
Lancet 1974;2:1127–31.Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, Anderson JA.
Studies with pain rating scales.
Ann Rheum Dis 1978;37:378–81.Huskisson EC, Wojtulewski JA, Berry H, Scott J, Hart FD, Balme HW.
Treatment of rheumatoid arthritis with fenoprofen: comparison with aspirin.
Br Med J 1974;1:176–80.Berry H, Huskisson EC.
Treatment of rheumatoid arthritis.
Clin Trials J 1972;4:13–5.Jensen MP, Karoly P, Braver S.
The measurement of clinical pain intensity:
a comparison of six methods.
Pain 1986;27:117–26.Burckhardt CS, Jones KD.
Adult measures of pain: The McGill Pain Questionnaire (MPQ),
Rheumatoid Arthritis Pain Scale (RAPS), Short-Form McGill
Pain Questionnaire (SF-MPQ), Verbal Descriptive Scale
(VDS), Visual Analog Scale (VAS), and West Haven-Yale
Multidisciplinary Pain Inventory (WHYMPI).
Arthritis Rheum 2003;49:S96–104.Ferraz MB, Quaresma MR, Aquino LR, Atra E, Tugwell P, Goldsmith CH.
Reliability of pain scales in the assessment of literate
and illiterate patients with rheumatoid arthritis.
J Rheumatol 1990;17:1022–4.Scott J, Huskisson EC.
Graphic representation of pain.
Pain 1976;2: 175–84.Joyce CR, Zutshi DW, Hrubes VF, Mason RM.
Comparison of fixed interval and visual analogue scales
for rating chronic pain.
Eur J Clin Pharmacol 1975;8:415–20.Jensen MP, Chen C, Brugger AM.
Interpretation of visual analog scale ratings and change scores:
a reanalysis of two clinical trials of postoperative pain.
J Pain 2003;4:407–14.Scott J, Huskisson EC.
Vertical or horizontal visual analogue scales.
Ann Rheum Dis 1979;38:560.Aitken RC.
Measurement of feelings using visual analogue scales.
Proc R Soc Med 1969;62:989–93.Clarke PR, Spear FG.
Reliability and sensitivity in the self-assessment of well-being.
Bull Br Psychol Soc 1964;17:18A.Woodforde JM, Merskey H.
Some relationships between subjective measures of pain.
J Psychosom Res 1972;16:173–8.Kremer E, Atkinson JH, Ignelzi RJ.
Measurement of pain: patient preference does not confound pain measurement.
Pain 1981;10: 241–8.Wolfe F, Michaud K.
Assessment of pain in rheumatoid arthritis: minimal clinically significant
difference, predictors, and the effect of anti-tumor necrosis factor therapy.
J Rheumatol 2007;34:1674–83.Tashjian RZ, Deloach J, Porucznik CA, Powell AP.
Minimal clinically important differences (MCID) and patient acceptable
symptomatic state (PASS) for visual analog scales (VAS) measuring
pain in patients treated for rotator cuff disease.
J Shoulder Elbow Surg 2009;18:927–32.Childs JD, Piva SR, Fritz JM.
Responsiveness of the numeric pain rating scale in patients with low back pain.
Spine 2005;30:1331–4.Jensen MP, McFarland CA.
Increasing the reliability and validity of pain
intensity measurement in chronic pain patients.
Pain 1993;55: 195–203.Rodriguez CS.
Pain measurement in the elderly: a review.
Pain Manag Nurs 2001;2:38–46.Farrar JT, Young JP Jr, LaMoreaux L, Werth JL, Poole RM.
Clinical importance of changes in chronic pain intensity
measured on an 11-point numerical pain rating scale.
Pain 2001;94:149–58.Johnson C. Measuring pain.
Visual analog scale versus numeric pain scale: what is the difference?
J Chiropr Med 2005;4:43–4.Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, et al.
Core outcome measures for chronic pain clinical trials:
IMMPACT recommendations.
Pain 2005;113:9–19.Jensen MP, Karoly P, O’Riordan EF, Bland F Jr, Burns RS.
The subjective experience of acute pain.
Clin J Pain 1989;5:153–9.Langley GB, Sheppeard H.
The visual analogue scale: its use in pain measurement.
Rheumatol Int 1985;5:145–8.De C Williams AC, Davies HT, Chadury Y.
Simple pain rating scales hide complex idiosyncratic meanings.
Pain 2000;85:457–63.Hawker GA, Davis AM, French MR, Cibere J, Jordan JM, March L, et al.
Development and preliminary psychometric testing of a
new OA pain measure: an OARSI/OMERACT initiative.
Osteoarthritis Cartilage 2008;16:409–14.Hush JM, Refshauge KM, Sullivan G, De Souza L, McAuley JH.
Do numerical rating scales and the Roland-Morris Disability Questionnaire
capture changes that are meaningful to patients with persistent back pain?
Clin Rehabil 2010;24:648–57.Burckhardt CS.
The use of the McGill Pain Questionnaire in assessing arthritis pain.
Pain 1984;19:305–14.Melzack R.
The McGill Pain Questionnaire: major properties and scoring methods.
Pain 1975;1:277–99.Escalante A, Lichtenstein MJ, White K, Rios N, Hazuda HP.
A method for scoring the pain map of the McGill
pain questionnaire for use in epidemiologic studies.
Aging Clin Exp Res 1995;7:358–66.Melzack R.
The short-form McGill Pain Questionnaire.
Pain 1987;30: 191–7.Menezes CL, Maher CG, McAuley JH, Costa LO.
Systematic review of cross-cultural adaptations of McGill
Pain Questionnaire reveals a paucity of clinimetric testing.
J Clin Epidemiol 2009;62:934–43.Boureau F, Luu M, Doubrere JF, Gay C.
Construction of a questionnaire for the self-evaluation
of pain using a list of qualifiers.
Therapie 1984;39:119–29.Geissner E.
Measuring pain via questionnaires: several results concerning the validity
of a modified German version of the McGill Pain Questionnaire.
Z Klin Psychol 1988;17:334–40.Kiss I, Muller H, Abel M.
The McGill Pain Questionnaire: German version.
Pain 1987;29:195–207.Stein C, Mendl G.
The German counterpart to McGill Pain Questionnaire.
Pain 1988;32:251–5.Kim HS, Schwartz-Barcott D, Holter IM, Lorensen M.
Developing a translation of the McGill pain questionnaire
for cross-cultural comparison: an example from Norway.
J Adv Nurs 1995;21:421–6.Van Lankveld WF, van Pad Bosch PF, van de Putte LF, van der Staak CF, Naring G.
Pain in rheumatoid arthritis measured with the visual analogue scale
and the Dutch version of the McGill Pain Questionnaire.
Ned Tijdschr Geneeskd 1992;136:1166–70.Maiani G, Sanavio E.
Semantics of pain in Italy: the Italian version
of the McGill Pain Questionnaire.
Pain 1985;22:399–405.Hasegawa M, Hattori S, Mishima M, Matsumoto IF, Kimura T, Baba Y, et al.
The McGill Pain Questionnaire, Japanese version, reconsidered:
confirming the theoretical structure.
Pain Res Manag 2001;6:173–80.Ketovuori H, Pontinen PJ.
A pain vocabulary in Finnish: the Finnish pain questionnaire.
Pain 1981;11:247–53.Lazaro C, Bosch F, Torrubia R, Banos JE.
The development of a Spanish questionnaire for assessing pain:
preliminary data concerning reliability and validity.
Euro J Psychol Assess 1994;10:145–51.Hui YL, Chen AC.
Analysis of headache in a Chinese patient population.
Ma Zui Xue Za Zhi 1989;27:13–8.Van der Kloot WA, Oostendorp RA, van der Meij J, van den HJ.
The Dutch version of the McGill pain questionnaire:
a reliable pain questionnaire.
Ned Tijdschr Geneeskd 1995;139:669–73. In Dutch.Aboud FE, Hiwot MG, Arega A, Molla M, Samson SN, Seyoum N, et al.
The McGill Pain Questionnaire in Amharic: Zwai Health
Center patients’ reports on the experience of pain.
Ethiop Med J 2003;41:45–61.Bartko D, Kondas M, Janco S.
Quantification of pain in neurology.
Cesk Neurol Neurochir 1984;47:113–21.Kuguoglu S, Aslan FE, Olgun N.
Turkish version of the McGill Melzack Pain Questionnaire Form (MPQF).
Agri-Istanbul 2003;15:47–51.Goncalves RS, Cabri J, Pinheiro JP, Ferreira PL, Gil J.
Cross-cultural adaptation and validation of the Portuguese version
of the intermittent and constant osteoarthritis pain
(ICOAP) measure for the knee.
Osteoarthritis Cartilage 2010;18:1058–61.Pimenta CA, Teixeiro MJ.
Proposal to adapt the McGill Pain Questionnaire into Portuguese.
Rev Esc Enferm USP 1996;30:473–83. In Portuguese.Varoli FK, Pedrazzi V.
Adapted version of the McGill Pain Questionnaire to Brazilian Portuguese.
Braz Dent J 2006;17:328–35.Torgerson WS.
Theory and methods of scaling.
New York: Wiley and Son; 1958.Chapman CR, Casey KL, Dubner R, Foley KM, Gracely RH, Reading AE.
Pain measurement: an overview.
Pain 1985;22:1–31.Broderick JE, Schwartz JE, Vikingstad G, Pribbernow M, Grossman S, Stone AA.
The accuracy of pain and fatigue items across different reporting periods.
Pain 2008;139:146–57.Love A, Leboeuf C, Crisp TC.
Chiropractic chronic low back pain sufferers and self-report assessment methods.
Part I. A reliability study of the Visual Analogue Scale,
the Pain Drawing and the McGill Pain Questionnaire.
J Manipulative Physiol Ther 1989;12:21–5.Roche PA, Klestov AC, Heim HM.
Description of stable pain in rheumatoid arthritis: a 6 year study.
J Rheumatol 2003;30:1733–8.Papageorgiou AC, Badley EM.
The quality of pain in arthritis: the words patients use to describe
overall pain and pain in individual joints at rest and on movement.
J Rheumatol 1989;16:106–12.Katz J, Clairoux M, Kavanagh BP, Roger S, Nierenberg H, Redahan C, et al.
Pre-emptive lumbar epidural anesthesia reduces postoperative pain and
patient-controlled morphine consumption after lower abdominal surgery.
Pain 1994;59:395–403.Creamer P, Lethbridge-Cejku M, Hochberg MC.
Determinants of pain severity in knee osteoarthritis: effect of
demographic and psychosocial variables using 3 pain measures.
J Rheumatol 1999;26:1785–92.Gandhi R, Tsvetkov D, Dhottar H, Davey JR, Mahomed NN.
Quantifying the pain experience in hip and knee osteoarthritis.
Pain Res Manag 2010;15:224–8.Jenkinson C, Carroll D, Egerton M, Frankland T, McQuay H, Nagle C.
Comparison of the sensitivity to change of long and short form pain measures.
Qual Life Res 1995;4:353–7.ICOAP User’s Guide.
Osteoarthritis Research Society International. 2011. URL:
http://www.oarsi.org/pdfs/pain_indexes/ICOAP_USERS_ GUIDE_07072010.pdfRasmussen PV, Sindrup SH, Jensen TS, Bach FW.
Symptoms and signs in patients with suspected neuropathic pain.
Pain 2004;110: 461–9.Dworkin RH, Corbin AE, Young JP Jr, Sharma U, LaMoreaux L, Bockbrader H, et al.
Pregabalin for the treatment of postherpetic neuralgia:
a randomized, placebo-controlled trial.
Neurology 2003;60:1274–83.Gilron I, Bailey JM, Tu D, Holden RR, Weaver DF, Houlden RL.
Morphine, gabapentin, or their combination for neuropathic pain.
N Engl J Med 2005;352:1324–34.Hsieh LL, Kuo CH, Yen MF, Chen TH.
A randomized controlled clinical trial for low back pain
treated by acupressure and physical therapy.
Prev Med 2004;39:168–76.Knotek P, Solcova I, Zalsky M.
Czech version of the short form McGill Pain Questionnaire: restandardization.
Bolest 2002;5:169–72.Perkins FM, Werner MU, Persson F, Holte K, Jensen TS, Kehlet H.
Development and validation of a brief, descriptive Danish pain questionnaire (BDDPQ).
Acta Anaesthesiol Scand 2004;48:486–90.Najafi-Ghezeljeh T, Ekman I, Nikravesh MY, Emami A.
Adaptation and validation of the Iranian version of
Angina Pectoris characteristics questionnaire.
Int J Nurs Pract 2008;14:470–6.Georgoudis G, Watson PJ, Oldham JA.
The development and validation of a Greek version
of the short-form McGill Pain Questionnaire.
Eur J Pain 2000;4:275–81.Georgoudis G, Oldham JA, Watson PJ.
Reliability and sensitivity measures of the Greek version
of the short form of the McGill Pain Questionnaire.
Eur J Pain 2001;5:109–18.Sloman R, Rosen G, Rom M, Shir Y.
Nurses’ assessment of pain in surgical patients.
J Adv Nurs 2005;52:125–32.Ahuja S, Saluja V, Bhattacharya A.
A Modified Short form McGill Pain Questionnaire for evaluation
of post-operative pain and behavioural response to pain relief.
J Anaesthesiol Clin Pharmacol 1999;15:149–53.Lee HF, Nicholson LL, Adams RD, Maher CG, Halaki M, Bae SS.
Development and psychometric testing of Korean language
versions of 4 neck pain and disability questionnaires.
Spine (Phila Pa 1976) 1976;31:1841–5.Lee MC, Essoka G.
Patient’s perception of pain: comparison between
Korean-American and Euro-American obstetric patients.
J Cult Divers 1998;5:29–37.Ljunggren AE, Strand LI, Johnsen TB.
Development of the Norwegian short-form McGill Pain Questionnaire (NSF-MPQ).
Adv Physiother 2007;9:169–80.Burckhardt CS, Bjelle A.
A Swedish version of the short-form McGill Pain Questionnaire.
Scand J Rheumatol 1994;23:77–81.Kitisomprayoonkul W, Klaphajone J, Kovindha A.
Thai Short-form McGill Pain Questionnaire.
J Med Assoc Thai 2006;89:846–53.Yakut Y, Yakut E, Bayar K, Uygur F.
Reliability and validity of the Turkish version short-form McGill
pain questionnaire in patients with rheumatoid arthritis.
Clin Rheumatol 2007;26:1083–7.Huskisson EC.
Current practice in rheumatology.
Practitioner 1983; 227:1087.Grushka M, Sessle BJ.
Applicability of the McGill Pain Questionnaire
to the differentiation of ’toothache’ pain.
Pain 1984;19:49–57.Hunter M.
The Headache Scale: a new approach to the assessment
of headache pain based on pain descriptions.
Pain 1983;16:361–73.Leavitt JW.
“Science” enters the birthing room:
obstetrics in America since the eighteenth century.
J Am Hist 1983;70:281–304.Grafton KV, Foster NE, Wright CC.
Test-retest reliability of the Short-Form McGill Pain Questionnaire:
assessment of intraclass correlation coefficients and l
imits of agreement in patients with osteoarthritis.
Clin J Pain 2005;21:73–82.Strand LI, Ljunggren AE, Bogen B, Ask T, Johnsen TB.
The Short-Form McGill Pain Questionnaire as an outcome measure:
test-retest reliability and responsiveness to change.
Eur J Pain 2008;12:917–25.Birch S, Jamison RN.
Controlled trial of Japanese acupuncture for chronic myofascial neck pain:
assessment of specific and nonspecific effects of treatment.
Clin J Pain 1998;14:248–55.Ruoff GE, Rosenthal N, Jordan D, Karim R, Kamin M.
Tramadol/acetaminophen combination tablets for the treatment of chronic lower back pain:
a multicenter, randomized, double-blind, placebocontrolled outpatient study.
Clin Ther 2003;25:1123–41.Dworkin RH, Turk DC, Revicki DA, Coyne KS, Peirce-Sandner S, Burke LB, et al.
Development and initial validation of an expanded and revised
version of the Short-form McGill Pain Questionnaire (SF-MPQ-2).
Pain 2009;144:35–42.Von Korff M, Ormel J, Keefe FJ, Dworkin SF.
Grading the severity of chronic pain.
Pain 1992;50:133–49.Elliott AM, Smith BH, Smith WC, Chambers WA.
Changes in chronic pain severity over time:
the Chronic Pain Grade as a valid measure.
Pain 2000;88:303–8.Elliott AM, Smith BH, Penny KI, Smith WC, Chambers WA.
The epidemiology of chronic pain in the community.
Lancet 1999;354: 1248–52.Von Korff M, Stewart WF, Lipton RB.
Assessing headache severity.
Neurology 1994;44:S40–6.Smith BH, Penny KI, Purves AM, Munro C, Wilson B, Grimshaw J, et al.
The Chronic Pain Grade questionnaire:
validation and reliability in postal research.
Pain 1997;71:141–7.Salaffi FF, Stancati AF, Grassi W.
Reliability and validity of the Italian version of the Chronic Pain
Grade questionnaire in patients with musculoskeletal disorders.
Clin Rheumatol 2006;25:619–31.Von Korff M, Dworkin SF, Le RL.
Graded chronic pain status: an epidemiologic evaluation.
Pain 1990;40:279–91.Turk DC, Rudy TE.
Towards a comprehensive assessment of chronic pain patients.
Behav Res Ther 1987;25:237–49.Turk DC, Rudy TE.
Toward an empirically derived taxonomy of chronic pain patients:
integration of psychological assessment data.
J Consult Clin Psychol 1988;56:233–8.Kerns RD, Turk DC, Rudy TE.
The West Haven-Yale Multidimensional Pain Inventory (WHYMPI).
Pain 1985;23:345–56.Krebs EE, Bair MJ, Damush TM, Tu W, Wu J, Kroenke K.
Comparative responsiveness of pain outcome measures among
primary care patients with musculoskeletal pain.
Med Care 2010;48:1007–14.Dunn KM, Jordan K, Croft PR.
Does questionnaire structure influence response in postal surveys?
J Clin Epidemiol 2003;56:10–6.Penny KI, Purves AM, Smith BH, Chambers WA, Smith WC.
Relationship between the chronic pain grade and measures
of physical, social and psychological well-being.
Pain 1999;79:275–9.Ware JE, Kosinski M, Keller SK.
SF-36 physical and mental health summary scales: a user’s manual.
Boston: The Health Institute; 1994.McHorney CA, Ware JE, Raczek AE.
The MOS 36-Item Short-Form Health Survey (SF-36) II: psychometric
and clinical tests of validity in measuring physical
and mental health constructs.
Med Care 1993;31: 247–63.Ware JE Jr, Sherbourne CD.
The MOS 36-item Short-Form health survey (SF-36). I.
Conceptual framework and item selection.
Med Care 1992;30:473–83.Ware JE, Kosinski M, Dewey JE.
How to score version two of the SF-36 Health Survey.
Lincoln (RI): QualityMetric; 2000.Ware JE, Gandek B.
Overview of the SF-36 Health Survey and the International
Quality of Life Assessment (IQOLA) project.
J Clin Epidemiol 1998;51:903–12.Shiely JC, Bayliss MS, Keller SD, Tsai C, Ware JE.
SF-36 Health Survey annotated bibliography: the first edition (1988-1995).
Boston: The Health Institute, New England Medical Center; 1996.Ware JE, Snow KK, Kosinski M, Gandek B.
SF-36 Health Survey: manual and interpretation guide.
Boston: The Health Institute, New England Medical Center; 1993.Bullinger M.
German translation and psychometric testing of the SF-36
Health Survey: preliminary results from the IQOLA Project.
Soc Sci Med 1995;41:1359–66.Alonso J, Prieto L, Anto JM.
The Spanish version of the SF-36 Health Survey (the SF-36 health questionnaire):
an instrument for measuring clinical results.
Med Clin (Barc) 1995;104:771–6. In Spanish.Sullivan M, Karlsson J, Ware JE Jr.
SF-36 Halsoenkat: Svensk manual och tolkningsguide
(Swedish manual and interpretation guide).
Gothenburg: Sahlgrenska University Hospital; 1994.Apolone G, Cifani S, Liberati MC, Mosconi P.
Questionario sullo stato di salute SF-36. Traduzione e
validazione della versione italiana: risultati del progetto IQOLA.
Metodologia e Didattica Clinica 1997;5: 86–94.Stewart AL, Ware JE.
Measuring functioning and well-being:
the Medical Outcomes Study approach.
Durham (NC): Duke University Press; 1992.Dupuy HJ.
The Psychological General Well-Being (PGWB) Index.
In: Wenger NK, Mattson ME, Furberg JF, Elinson JA, editors.
Assessment of quality of life in clinical trials
of cardiovascular therapies.
New York: Le Jacq; 1984. p. 170–83.Hulka BS, Cassel JC.
The AAFP-UNC study of the organization, utilization,
and assessment of primary medical care.
Am J Public Health 1973;63:494–501.Patrick DL, Bush JW, Chen MM.
Methods for measuring levels of well-being for a health status index.
Health Serv Res 1973;8:228–45.Quintana JM, Escobar A, Bilbao A, Arostegui I, Lafuente I, Vidaurreta I.
Responsiveness and clinically important differences for
the WOMAC and SF-36 after hip joint replacement.
Osteoarthritis Cartilage 2005;13:1076–83.Escobar A, Quintana JM, Bilbao A, Arostegui I, Lafuente I, Vidaurreta I.
Responsiveness and clinically important differences for
the WOMAC and SF-36 after total knee replacement.
Osteoarthritis Cartilage 2007;15:273–80.Koh ET, Leong KP, Tsou IY, Lim VH, Pong LY, Chong SY, et al.
The reliability, validity and sensitivity to change of the Chinese
version of SF-36 in oriental patients with rheumatoid arthritis.
Rheumatology (Oxford) 2006;45:1023–8.Brazier J, Harper R, Jones SN.
Validating the SF-36 Health Survey Questionnaire:
New Outcome Measure for Primary Care
British Medical Journal 1992 (Jul 18); 305 (6846): 160-164Brazier JE, Harper R, Jones NM, O’Cathain A, Thomas KJ, Usherwood T, et al.
Validating the SF-36 Health Survey questionnaire:
new outcome measure for primary care.
BMJ 1992;305:160–4.Bombardier C, Melfi C, Paul J, Green R, Hawker GA, Wright J, et al.
Comparison of a generic and a disease-specific measure of pain
and physical function after knee replacement surgery.
Med Care 1995;33: AS131–44.Salaffi F, Leardini G, Canesi B, Mannoni A, Fioravanti A, Caporali R, et al.
Reliability and validity of the Western Ontario and McMaster Universities
(WOMAC) Osteoarthritis Index in Italian patients with osteoarthritis of the knee.
Osteoarthritis Cartilage 2003;11:551–60.Hawker GA, French MR, Elkayam JG, Davis AM. Unpredictability of intermittent knee OA pain:
impact on pain, function, and mood.
Arthritis Rheum 2010;62 Suppl 10:S284–5.Kessler S, Grammozis A, Gunther KP, Kirschner S.
The Intermittent and Constant Pain Score (ICOAP): a questionnaire
to assess pain in patients with gonarthritis.
Z Orthop Unfall 2010;149:22–6. In German.Maillefert JF, Kloppenburg M, Fernandes L, Punzi L, Gunther KP, Martin Mola E, et al.
Multi-language translation and cross-cultural adaptation of the OARSI/OMERACT
measure of intermittent and constant osteoarthritis pain (ICOAP).
Osteoarthritis Cartilage 2009;17: 1293–6.Hawker GA, Stewart L, French MR, Cibere J, Jordan JM, March L, et al.
Understanding the pain experience in hip and knee steoarthritis:
an OARSI/OMERACT initiative.
Osteoarthritis Cartilage 2008;16:415–22.Hawker GA, Davis A, Lohmander S.
Responsiveness of the new OARSI-OMERACT OA pain and function measures [abstract].
Ann Rheum Dis 2009;68 Suppl 3:350.Davis AM, Lohmander LS, Wong R, Venkataramanan V, Hawker GA.
Evaluating the responsiveness of the ICOAP
following hip or knee replacement.
Osteoarthritis Cartilage 2010;18:1043–5.
Return to OUTCOME ASSESSMENT
Since 1-16-2023


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |