

Nucleus Pulposus Deformation Following Application of
Mechanical Diagnosis and Therapy: A Single Case
Report with Magnetic Resonance ImagingThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Man Manip Ther. 2010 (Sep); 18 (3): 153-158 ~ FULL TEXT
OPEN ACCESS Hiroshi Takasaki, Stephen May, Peter J Fazey, and Toby Hall
Division of Physiotherapy,
School of Health and Rehabilitation Science,
The University of Queensland, Australia.
BACKGROUND: The McKenzie management strategy of mechanical diagnosis and therapy (MDT) is commonly used for the assessment and management of spinal problems. Within this system, 'derangement syndrome' is the most common classification, for which the conceptual model is an intra-discal displacement. However, the reduction of an intra-discal displacement by MDT has never been documented. The purpose of this study was to compare, using magnetic resonance imaging (MRI), the nucleus pulposus (NP) profiles before and after the use of this approach.
PATIENT CHARACTERISTICS: The patient was a 34-year-old female with a long history of right sided low back and buttock pain classified with 'derangement syndrome'.
EXAMINATION: T2-weighted images of the L4-5 disc at initial assessment were compared with that at final assessment 1 month later. Initially, the MRI showed a portion of the NP displaced right and posteriorly towards the side of pain, and an overall NP position in the coronal plane shifted to the left.
INTERVENTION: The patient was managed with a 1-month course of the McKenzie management strategy treatment.
OUTCOMES: One month later, the displaced portion of the NP was no longer present and the left-shifted NP was centrally located.
DISCUSSION: These intervertebral disc changes coincided with centralization and abolition of symptoms. This case may support the conceptual model of MDT.KEYWORDS: Intervertebral disc; Low back pain; Magnetic resonance imaging; Manual therapies; McKenzie; Nucleus pulposus
There are more articles like this @ our: SPINAL ALLIGNMENT/CERVICAL CURVE Page Page
From the FULL TEXT Article:
Background
It is suggested that one of the major sources of low back pain (LBP) is the intervertebral disc. [1] The mechanical cause of disc pain appears to relate to a series of structural failures which can culminate in an internal disc derangement being displaced down a radial fissure. [2] It has been shown that asymmetrical loading of the disc leads to displacement of the nucleus pulposus (NP) to areas of least pressure. [3] Furthermore, it has been suggested that radial fissures bring about excessive mechanical strain on surviving annular layers, and that displaced fragments could mechanically stress surviving and innervated outer annular layers causing pain. [4]
Mechanical diagnosis and therapy (MDT) proposed by McKenzie is a comprehensive management strategy for a range of spinal pain disorders using specific forms of exercise individually prescribed. [4] McKenzie and May [4] put forward a theoretical conceptual model by which MDT improves discogenic pain, which was based on changes within the internal disc structure. They suggested that specific lumbar exercises may generate mechanical force sufficient to correct mal-positioning of internal disc structures, when outer annular layers are intact. In contrast, these exercises are unlikely to be effective when the outer annular layers are ruptured. However, clinically, it is known that positive response to repeated extension exercises can rescue some patients from a surgical intervention for a disc herniation. [5] Furthermore, the presence of centralization and peripheralization has been shown to correlate strongly with positive discography. [6] The ability of centralization to predict a positive provocation discography has been estimated to have a sensitivity of 40%, a specificity of 94%, and a positive likelihood ratio of 6.9. [7] However, no study has looked at changes in the intervertebral disc before and after an episode of MDT.
A recent systematic review showed greater effectiveness of MDT when compared to other therapeutic modalities.8 However, the therapeutic biomechanical basis by which MDT helps discogenic pain has not been studied extensively. The emergence of magnetic resonance imaging (MRI) has allowed a more detailed observation of intervertebral disc in vivo. Recently, Fazey et al. [3, 9] proposed analysis of the hydration profiles of the middle intervertebral discs, which allowed predicting an overall NP location in the coronal plane. As MRI is non-invasive, such data are useful to investigate the theoretical model of MDT. The purpose of this case report was to compare the hydration profiles of the NP, using MRI, before and after the application of MDT.
Patient Characteristics

Table 1 The patient was a 34-year-old female employed in home duties, with a complaint of constant low back and right buttock pain (Table 1). An orthopaedic surgeon and a radiologist diagnosed an L4–5 disc bulge, following MRI evaluation. The patient’s score for pain rating on a numeric pain rating scale (NPRS) and the Oswestry disability index (ODI) are also demonstrated in Table 1. She was not taking any medication at the time of this investigation. The subject in this case study provided informed consent for her case study to be published, and her anonymity was guaranteed. Data collection was conducted in Shinoro Orthopedic, Sapporo, Japan.
History
The onset of central low back pain occurred 6 years previously when lifting a sofa. The patient was prescribed non-steroidal anti-inflammatory drugs and was recommended to use a soft corset and rest for a few days by an orthopaedic surgeon. The doctor also recommended traction, electrotherapy, acupuncture, and strengthening of abdominal muscles, which commenced 2 weeks after the onset of pain. The patient regularly received these treatments for more than 3 months, but stopped attending as she felt that there was little improvement after the first few weeks. Since then, the low back pain had been constant and gradually progressing into her right buttock. Since this initial period of treatment, the patient had not received any other form of physiotherapy intervention.
The patient’s symptoms worsened with trunk flexion in standing, sustained sitting, rising from a chair, sustained standing, and walking. Sustained standing, sitting, and walking also increased the right buttock pain. The patient reported no tingling, numbness, or muscle weakness, but she felt that her gait had changed, due to pain, as a result of a recent increase in the severity of symptoms. The patient was otherwise generally healthy with no evidence of red or yellow flags to indicate serious spinal pathology or psychosocial issues.
Physical Examination
During the history-taking, her sitting posture was characterized as slouched with the lumbar spine positioned in end-range flexion. When the patient was guided into upright sitting (neutral lumbar lordosis: half way between anterior and posterior pelvic tilt), the patient reported an increase in the right buttock pain. Postural assessment in standing revealed an apparent right-lateral shift, with the upper trunk and shoulders displaced to the right. This shift had been noted by the patient and her husband after the original onset of symptoms 6 years previously, but had never fully resolved.
A clinical neurological examination of the dermatomes, myotomes, and reflexes was normal. Right side straight leg raising (SLR) reproduced low back and right buttock pain at around 40°. The addition of passive dorsiflexion just short of 40° increased the symptoms. Left SLR was not provocative and the range was 80°.
In testing pain responses to gentle palpation of specific nerve trunks, the patient reported intense pain on palpation of the right sciatic nerve in the gluteal region but no abnormal response when palpating the tibial, common peroneal, femoral, lateral femoral cutaneous, and medial calcaneal nerves.
Trunk flexion was grossly restricted, fingertips only reaching the mid-thigh, and increased the back and right buttock pain. Similarly, extension was also grossly restricted in range and increased both the back and right buttock pain. Side-gliding the upper trunk to the right increased only back pain. There was mild restriction of left side-gliding, but this also increased right buttock pain.
The effect of repeated movements on baseline pain status was established with respect to change in pain intensity and the distal extent of referred symptoms. Within MDT, responses to repeated movement provide information that determines classification into one of the three syndromes — derangement, dysfunction, or postural syndrome — and determines directionally relevant loading strategies for management.4 For instance, a rapid change in the extent of referred pain or pain intensity would indicate ‘derangement syndrome’. In this syndrome, pain can be made to centralize proximally, with progressively less distal referral, with repeated movement in a specific direction — a directional preference, which may then guide exercise prescription in treatment.
In this case study, pain responses were monitored after 3–4 sets of 10 repetitions of repeated movement. From the patient’s report of aggravating activities, as well as the response to postural correction, and the presence of a visible right-lateral shift, a lateral component to the patient’s problem was considered present and mechanical force in the coronal plane deemed beneficial for investigation of a directional preference. Additionally, the location of the pain response during left side-gliding was more distal than that during right side-gliding. This information suggested that right side-gliding would be the directional preference. Hence, right side-gliding (shoulder to right) was tested first. The patient reported increased low back and right buttock pain during testing, but this returned to baseline after the first series. However, after four sets of the repetitions, the right buttock pain disappeared, and right and left side-glide ranges of movement (ROM) had increased. Following this, as the pain appeared to centralize to the lower back, the response to repeated extension in lying was assessed. With three sets of 10 repetitions, the patient’s back pain increased during the movement, but returned to the same level at the end of each set with no change in subsequent reassessment of extension ROM. Given the failure to affect changes with purely sagittal plane movements and given the previous relevance of a lateral component, the response to extension in lying with hips off-centre to left was tested. Initial movements reduced the size of the painful area and multiple-repeated movements abolished the central back pain.
After the repeated movements, the patient’s low back and buttock pain disappeared completely and there was no evidence of a lateral shift in standing. The range of right SLR had increased to 80° without any pain and when the patient flexed forward, her fingers reached to the middle of her lower leg. The pain intensity on palpation of the right sciatic nerve was much less but still slightly tender.
Clinical Impression
Following tests of repeated movement, there was an apparent directional preference and centralization of symptoms. Therefore, the provisional classification was ‘derangement syndrome’ with initial treatment directed towards improving right side-gliding and postural correction.
Intervention
At the first consultation, the patient was prescribed home exercise consisting of repeated right side-gliding in standing 10–20 times and subsequently, repeated extension in lying (with hips displaced left) 10–20 times, every 3 hours. She was instructed to stop exercising if she felt the pain get worse or move distally. She was also advised to pay attention to her posture and to maintain her lordosis with a lumbar support when sitting.
At the second consultation, which was 2 days later from the first consultation, the patient reported good exercise compliance and demonstrated improved postural habit. She had experienced no pain when doing daily activities after the first consultation. There was no evidence of a lateral shift in standing. Although no specific range of motion measurement was conducted in an effort to prevent exacerbation of symptoms at this early stage, no tenderness was reported on palpation of the right sciatic nerve. In view of the significant improvement, the patient was instructed to perform only extension in lying 10–20 times every 3 hours.
At the third consultation, which was 2 weeks after the first consultation, she reported no pain during daily activities. With repeated movements in all directions, there was no reproduction of pain, and range of movement and response to extension did not change following repeated flexion in lying. Based upon this, to restore full function and ensure that there was no reluctance to move in certain directions, a flexion programme was initiated and written down for the patient. This consisted of slouch-overcorrect on the first day, flexion in lying on the second, followed by flexion in sitting for 5 days during which the legs were gradually straightened, and finally flexion in standing. The advice was to perform 10 repetitions five times daily, but initially with each new exercise to perform only five repetitions. Each exercise was to be followed by a series of extension in standing exercises.
At the final evaluation, which was 1 month after the first consultation, she reported no pain or difficulties with the flexion program. Furthermore, she had experienced no pain and had little anxiety about lumbar spine movement or activities of daily living. Changes in the NPRS and the ODI scores are summarized in Table 1. Based upon these positive findings, the patient was discharged from physical therapy. Finally, the patient was re-scanned.
MRI assessment
MRI data were obtained by a 0.2 T horizontally open MRI unit (AIRIS Mate; Hitachi Inc., Sapporo, Japan) with the subject resting in a supine position. MRI data were collected prior to the above physical assessment using MDT and also 1 month later at the final review appointment. On both occasions, the MRI scan was conducted at the same time of day. T1- and T2-weighted images were acquired in the sagittal, coronal, and axial planes with the following MRI setting: T1 sagittal (FSE, FOV: 300; TR/TE: 385/24.5 ms; thickness: 6.0 mm; interval: 7.0 mm; scan time: 5:45), T2 sagittal (FSE, FOV: 300; TR/TE: 2640/125 m; thickness: 6.0 mm; interval: 7.0 mm; scan time: 5:48), T1 coronal (FSE, FOV: 320; TR/TE: 400/16.0 ms; thickness: 4.0 mm; interval: 5.0 mm; scan time: 6:24), T2 coronal (FSE, FOV: 320; TR/TE: 2750/100 ms; thickness: 4.0 mm; interval: 5.0 mm; scan time: 6:14), T1 axial (FSE, FOV: 260; TR/TE: 450/19.3 ms; thickness: 8.0 mm; interval: 8.0 mm; scan time: 5:46), and T2 axial (FSE, FOV: 260; TR/TE: 3120/120 ms; thickness: 8.0 mm; interval: 8.0 mm; scan time: 6:52). From the axial T2-weighted image of the central disc region at the level of L4–5, a pixel intensity profile was computed using ImageJ 1.6 software (National Institute of Mental Health, Bethesda, MD, USA), along with the measurement method described by Fazey et al.3 Pixel intensity, along three lines through the middle disc area, was collected and for each line, data were normalized to 100 points using LabVIEW software (National Instruments, Austin, TX, USA). Subsequently, normalized pixel intensity was averaged. A proportion of the offset bulk of the pixel was calculated to understand the overall NP position in the coronal plane and used for ensuing comparisons.
To investigate changes in joint alignment at the L4–5 level between measurement sessions, segmental angles were measured using the T1-weighted images in both coronal and axial planes using the following method. [3] Segmental angles were calculated by subtracting the values of the lower vertebrae from those of the upper vertebrae. Segmental left lateral flexion and rotation were expressed as positive. For the measurement of the lateral flexion angles, the four corners of each vertebral body (L4 and L5) were identified and then the midlines of each vertebra, which were defined as lines running through the midpoints between the two anterior and the two posterior corners, were drawn and the values between these lines and the axial plane were calculated. To measure rotation angles, lines from the spinous process of the L4 and L5 vertebra to the midpoint of the L4 and L5 vertebral bodies were drawn. The values between these lines and the sagittal plane were calculated.
Outcomes

Table 2
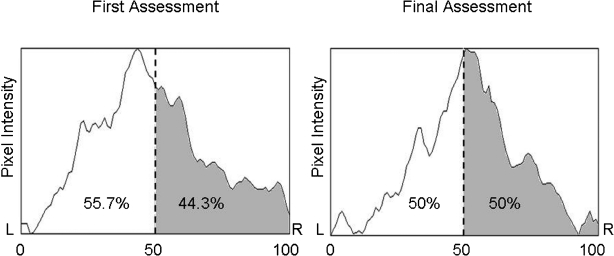
Figure 1 A radiologist examined the T2-weighted images at the L4–5 disc. These results are summarized in Table 2. The lines of pixel intensity in the coronal plane in the centre of the L4–5 discs at the initial and final assessment are shown in Figure 1. Notably, the bulk of pixels in the initial assessment were shifted to the left with a 15.7% offset, while the bulk of pixels were equally balanced on the right and left in the final assessment.
There was minimal change in alignment of the L4–5 segment between MRI measurement occasions. Orientation in the coronal plane at the first and the final assessment was –0.89° and –0.50° lateral flexion, respectively. Similarly, orientation in the axial plane at the first and the final assessment was 0.67° and 0.82° of rotation, respectively.
Discussion
First, on the T2-weighted images, a portion of the NP was displaced right and posteriorly within the disc at the initial assessment, but this displacement was no longer present at follow-up when the symptoms were abolished following an intervention putatively targeted at the lumbar intervertebral disc. The intervertebral disc changes coincided with centralization and abolition of symptoms. It has been reported that the degree of radial fissuring is strongly related to discogenic pain. [10, 11] In addition, when the NP projects through these radial fissures and stimulates outer layers, pain can be provoked. [4] O’Neill et al. [12] showed that the extent of peripheralization of leg symptoms might relate to the intensity of stimulus to the painful disc. Hence, the relocation of the portion of the NP, which was displaced right and posteriorly, might have decreased pressure on the outer layers of the annulus and might have lead to the centralization and abolition of symptoms.
Second, in the relationship between postural shift and the direction of repeated movements, generally the postural shift is corrected by side-gliding in the opposite direction of the shift. [4] However, in this case, the direction of apparent lateral shift in standing and the direction of repeated movement which led to postural correction were the same. Side-gliding in the opposite direction of the lateral shift caused an increase in symptoms (peripheralization). Hence, a reason for the postural shift in this case may be explained as an antalgic posture adopted by the patient subconsciously. According to Mulvein and Jull, [13] a posture with side glide (shifted posture) is a combination of ipsilateral lateral flexion of the lower lumber segments and contralateral lateral flexion of the upper segments. Fazey et al. [3] reported that the NP tended to move in the opposite direction during lateral flexion. Thus, at the lower lumber discs, side glide to the left is likely to cause the NP to displace to the right. As the patient already had a portion of the NP displaced right and posteriorly at the initial assessment, the patient may have subconsciously shifted to the right in an attempt to minimize further lateral displacement of the portion of the NP stimulating outer annular layers.
In addition, assessment with the hydration profiles could provide further discussion regarding a link between the NP position and habitually shifted posture. Despite the minimum change of the joint alignments at L4–5 during MRI scanning, 15.7% of the bulk of pixel was shifted left in the initial MRI scan. It is known that even for asymptomatic subjects, the standard deviations of the offset bulk of pixel in the supine position is 7.37%. [3] The initial offset in this case was almost double the standard deviation in asymptomatic subjects. Hence, it seems to be reasonable to think that in the initial assessment, the overall NP position was shifted considerably to the left. The discrepancy between the minimal offset of the joint alignment and the left-shifted NP position can be explained by Kramer’s report. [14] He stated that the NP under prolonged asymmetrical compression tended to stay in the displaced position and to achieve a change in the NP position, it was necessary to apply force in the opposite direction. Indeed, since the patient had a habitual right-shifted posture, theoretically the NP would be under constant pressure to remain offset to the left. Hence, just correcting posture in the supine position for the MRI scanning would not have been enough to correct the left-shifted NP position.
Study limitations
There is a significant limitation in this study. We hypothesized that the change in disc profile was related to the intervention. However, this cannot be absolutely certain given the length of time between MRI procedures and the uncertainty of stability of measuring disc profiles over time. Repeat MRIs performed immediately before and after centralization and abolition of symptoms would be more convincing evidence of a link between centralization and changes to the disc profile. Further study would be required.
Conclusion
In conclusion, in this case study, the disc profiles of the lumbar intervertebral disc clearly showed that NP displacements were relocated to the centre of the disc after a 1-month course of treatment based on the MDT management strategy. The conceptual model in MDT is supported by the objective changes observed using MRI in this case study, though further investigations are required to determine if the MRI changes are causally related to the change in symptoms.
Acknowledgments
The authors wish to acknowledge Yoshikazu Ikemoto (MD, PhD) and Mitsuharu Tamakawa (MD) for the inspection of the patient’s MRI, and the patient for volunteering for study.
References:
Kramer J.
Intervertebral disk diseases: causes, diagnosis, treatment and prophylaxis. 3rd ed.
New York: Georg Thieme Verlag; 2008Adams MA, Roughley PJ.
What is intervertebral disc degeneration, and what causes it?
Spine (Phila Pa 1976) 2006;31:2151–61Fazey PJ, Takasaki H, Singer KP.
Nucleus pulposus deformation in response to lumbar spine lateral flexion:
an in vivo MRI investigation.
Eur Spine J 2010; Mar 5McKenzie R, May S.
The lumbar spine: mechanical diagnosis and therapy. 2nd ed.
Waikenae: Spinal Publications; 2003Alexander AH, Jones AM, Rosenbaum DH., Jr
Nonoperative management of herniated nucleus pulposus: patient selection
by the extension sign. Long-term follow-up.
Orthop Rev 1992;21:181–8Donelson R, Aprill C, Medcalf R, Grant W.
A prospective study of centralization of lumbar and referred pain:
a predictor of symptomatic discs and anular competence.
Spine (Phila Pa 1976) 1997;22:1115–22Laslett M, Oberg B, Aprill CN, McDonald B.
Centralization as a predictor of provocation discography results in chronic low back pain,
and the influence of disability and distress on diagnostic power.
Spine J 2005;5:370–80Clare HA, Adams R, Maher CG.
A systematic review of efficacy of McKenzie therapy for spinal pain.
Aust J Physiother 2004;50:209–16Fazey PJ, Song S, Monsas S, Johansson L, Haukalid T, Price RI, et al.
An MRI investigation of intervertebral disc deformation in response to torsion.
Clin Biomech (Bristol, Avon) 2006;21:538–42Videman T, Nurminen M.
The occurrence of anular tears and their relation to lifetime back pain history:
a cadaveric study using barium sulfate discography.
Spine (Phila Pa 1976) 2004;29:2668–76Videman T, Battie MC, Gibbons LE, Maravilla K, Manninen H, Kaprio J.
Associations between back pain history and lumbar MRI findings.
Spine (Phila Pa 1976) 2003;28:582–8O’Neill CW, Kurgansky ME, Derby R, Ryan DP.
Disc stimulation and patterns of referred pain.
Spine (Phila Pa 1976) 2002;27:2776–81Mulvein K, Jull G.
Kinematic analysis of the lumbar lateral flexion and lumbar lateral shift movement techniques.
J Man Manip Ther 1995;3:104–9Kramer J.
Intervertebral disk disease. Cause, diagnosis, treatment and prophylaxis. 2nd ed.
New York: George Thieme Verlag; 1990
Return to McKENZIE METHOD
Since 12-28-2018


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |