

Spinal Manipulation and Home Exercise With Advice
for Subacute and Chronic Back-related Leg Pain:
A Trial With Adaptive AllocationThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Annals of Internal Medicine 2014 (Sep 16); 161 (6): 381—391 ~ FULL TEXT
Gert Bronfort, DC, PhD; Maria A. Hondras, DC, MPH; Craig A. Schulz, DC, MS;
Roni L. Evans, DC, PhD; Cynthia R. Long, PhD; and Richard Grimm, MD, PhD
University of Minnesota,
Northwestern Health Sciences University, and
Berman Center for Outcomes and Clinical Research at
the Minneapolis Medical Research Foundation,
Minneapolis, Minnesota, and
Palmer Center for Chiropractic Research,
Davenport, Iowa.
BACKGROUND: Back-related leg pain (BRLP) is often disabling and costly, and there is a paucity of research to guide its management.
OBJECTIVE: To determine whether spinal manipulative therapy (SMT) plus home exercise and advice (HEA) compared with HEA alone reduces leg pain in the short and long term in adults with BRLP.
DESIGN: Controlled pragmatic trial with allocation by minimization conducted from 2007 to 2011.
(ClinicalTrials.gov: NCT00494065).
SETTING: 2 research centers (Minnesota and Iowa).
PATIENTS: Persons aged 21 years or older with BRLP for least 4 weeks.
INTERVENTION: 12 weeks of SMT plus HEA or HEA alone.
MEASUREMENTS: The primary outcome was patient-rated BRLP at 12 and 52 weeks. Secondary outcomes were self-reported low back pain, disability, global improvement, satisfaction, medication use, and general health status at 12 and 52 weeks. Blinded objective tests were done at 12 weeks.
RESULTS: Of the 192 enrolled patients, 191 (99%) provided follow-up data at 12 weeks and 179 (93%) at 52 weeks. For leg pain, SMT plus HEA had a clinically important advantage over home exercise and advice (HEA) (difference, 10 percentage points [95% CI, 2 to 19]; P=0.008) at 12 weeks but not at 52 weeks (difference, 7 percentage points [CI, -2 to 15]; P=0.146). Nearly all secondary outcomes improved more with SMT plus HEA at 12 weeks, but only global improvement, satisfaction, and medication use had sustained improvements at 52 weeks. No serious treatment-related adverse events or deaths occurred.
LIMITATION: Patients and providers could not be blinded.
CONCLUSION: For patients with back-related leg pain (BRLP), SMT plus home exercise and advice (HEA) was more effective than HEA alone after 12 weeks, but the benefit was sustained only for some secondary outcomes at 52 weeks.
From the FULL TEXT Article:
Background
Back-related leg pain (BRLP) is an important symptom commonly associated with pervasive low back pain (LBP) conditions and, despite its socioeconomic effect, has been generally understudied. With poorer prognosis and quality of life, persons with BRLP have greater pain severity and incur more work loss, medication use, surgery, and health-related costs than those with uncomplicated LBP. [1–6]
Most patients with BRLP are treated with prescription medications and injections, although little to no evidence supports their use. [7, 8] Surgical approaches are also commonly applied, although there is only some evidence for short-term effectiveness compared with less invasive treatments. [9] Concerns are mounting about the overuse, costs, and safety of these conventional medical treatments [10–18], warranting identification of more conservative treatment options. Spinal manipulative therapy (SMT), exercise, and education promoting self-management are increasingly recommended as low-risk strategies for BRLP. [19] Although limited, evidence shows that these conservative approaches can be effective. [20–26] A recent systematic review by our group showed that SMT is superior to sham SMT for acute BRLP in the short and long term; however, the evidence for subacute and chronic BRLP is inconclusive, and high-quality research is needed to inform clinical and health policy decisions. [20] The underlying mechanisms of SMT seem to be multifactorial, including improvement in spinal stiffness, muscle recruitment, and synaptic efficacy of central neurons. [27, 28]
The purpose of this study was to test the hypothesis that the addition of SMT to home exercise and advice (HEA) would be more effective than HEA alone for patients with subacute and chronic BRLP.
METHODS
Design Overview
This pragmatic trial used a parallel design with allocation by minimization and has been described previously. [29] Patients were recruited between 2007 and 2010, and follow-up was completed in 2011. Institutional review boards approved the study protocol, and all patients provided written consent. The primary outcomes and most secondary outcomes were self-reported; objective measures were obtained by blinded examiners. There were no important changes to methods after trial commencement.
Settings and Patients
The trial was conducted at institution-affiliated research clinics at Northwestern Health Sciences University (Minneapolis, Minnesota) and Palmer College of Chiropractic (Davenport, Iowa). Patients were recruited through newspaper advertisements, direct mail, and community posters. Interested patients were initially screened by telephone interviews, followed by 2 in-person baseline evaluation visits. Inclusion criteria were age 21 years or older; BRLP based on Quebec Task Force on Spinal Disorders classifications 2, 3, 4, or 6 (radiating pain into the proximal or distal part of the lower extremity, with or without neurologic signs) (30); BRLP severity of 3 or greater (scale of 0 to 10); a current episode of 4 weeks or more; and a stable prescription medication plan in the previous month. Exclusion criteria were Quebec Task Force on Spinal Disorders classifications of 1, 5, 7, 8, 9, 10, and 11 (pain without radiation into the lower extremities, progressive neurologic deficits, the cauda equina syndrome, spinal fracture, spinal stenosis, surgical lumbar spine fusion, several incidents of lumbar spine surgery, chronic pain syndrome, visceral diseases, compression fractures or metastases, blood clotting disorders, severe osteoporosis, and inflammatory or destructive tissue changes of the spine). Patients could not be receiving ongoing treatment of leg pain or LBP; be pregnant or nursing; have current or pending litigation for worker’s compensation, disability, or personal injury; be unable to read or comprehend English; or have evidence of substance abuse.
Allocation
A Web-based program assigned patients to treatment after the second baseline visit using a minimization algorithm based on the Taves method [31], balancing on 7 baseline characteristics previously shown to influence outcomes. [32–34] Baseline characteristics included age, BRLP duration, neurologic signs, distress, positive straight leg raise, time spent driving a vehicle, and pain aggravation with coughing or sneezing. Patients were assigned in a 1:1 ratio, stratified by site. The allocation algorithm was prepared by the study statistician before enrollment, and its administration was concealed from study personnel.
Interventions
The intervention protocols were developed and tested in previous pilot studies. [32, 33] Both interventions were intended to be pragmatic in nature (for example, modified to patient presentation and needs) and were informed by commonly recommended clinical practices, patient preferences, and promising research evidence. [19, 35–38]
Eleven chiropractors with a minimum of 5 years of practice experience delivered SMT in the SMT plus HEA group. Thirteen providers (7 chiropractors, 5 exercise therapists, and 1 personal trainer) delivered the HEA intervention. When possible, patients worked with the same providers during the 12–week course of care; however, to accommodate patient and provider schedules during the intervention period, providers were trained to comanage patients. Treatment fidelity was facilitated through standardized training, manuals of operation, and clinical documentation forms that were monitored weekly by research staff.
SMT Plus HEA Group
As many as 20 SMT visits were allowed, each lasting 10 to 20 minutes, including a brief history and examination. Patients assigned to SMT plus HEA also attended 4 HEA visits, as described in the HEA Group section. For SMT visits, the primary focus of treatment was on manual techniques (including high-velocity, low amplitude thrust procedures or low-velocity, variable amplitude mobilization maneuvers to the lumbar vertebral or sacroiliac joints). The specific spinal level treated and the number and frequency of SMT visits were determined by the clinician on the basis of patient-reported symptoms, palpation, and pain provocation tests. [39] Adjunct therapies to facilitate SMT were used as needed and included light soft-tissue techniques (that is, active and passive muscle stretching and ischemic compression of tender points) and hot or cold packs. To facilitate adherence to HEA, chiropractors asked about patients’ adherence, reaffirmed main HEA messages, and answered questions as needed.
HEA Group
Home exercise and advice were delivered in four 1–hour, one-on-one visits during the 12–week intervention. The main program goals were to provide patients with the tools to manage existing pain, prevent pain recurrences, and facilitate engagement in daily activities.
Instruction and practice were provided for positioning and stabilization exercises to enhance mobility and increase trunk endurance. These were individualized to patients’ lifestyles, clinical characteristics (including positional sensitivities), and fitness levels. Positioning exercises included extension and flexion motion cycles (patients were encouraged to perform 25 repetitions 3 times per day in the lying, standing, or seated position). [33, 40] Stabilization exercises included pelvic tilt, quadruped, bridging, abdominal curl-ups, and side bridging with positional variations appropriate to patients’ tolerance and abilities. [41] Patients were instructed to do 8 to 12 repetitions of each stabilization exercise every other day.
Patients were also instructed in methods for developing spine posture awareness related to their activities of daily living, such as lifting, pushing and pulling, sitting, and getting out of bed. [42] Information about simple pain-management techniques, including cold, heat, and movement, was also provided.
Printed materials were distributed to take home and review. They included instructions of exercises with photos and a modification of the Back in Action book [43], emphasizing movement and restoration of normal function and fitness. [35, 44]
To facilitate adherence to HEA, providers called or e-mailed patients 3 times (at 1, 4, and 9 weeks) to reaffirm main messages and answer exercise-related questions.
Outcomes and Measurements
Patients’ demographic and clinical characteristics were collected at their first baseline visit through self-report questionnaires, histories, and physical examinations. Selfreported outcomes were collected at the baseline visit and at 3, 12, 26, and 52 weeks via questionnaires independent of study personnel influence. Patients were queried in each questionnaire about attempts to influence their responses.
The primary outcome measure was patient-rated typical level of leg pain during the past week using an 11– point numerical rating scale, a reliable, valid, and important patient-centered outcome. [36, 45–47] The primary end points were 12 weeks, which was the end of the intervention phase, and the 52–week follow-up.
A complete description of all secondary outcome measures is provided elsewhere. [29] The measures reported in this article include LBP, disability measured with the modified Roland–Morris Disability Questionnaire [48–50], physical and mental health status using the Short Form-36 Health Survey (SF–36) [51, 52], patient satisfaction [53], global improvement [53], and frequency of medication use for back and leg pain in the past week. [53]
Patient expectations about treatment were measured using an 11–box numerical rating scale (0 meaning treatment was not at all helpful and 10 meaning it was extremely helpful) at baseline. Expected side effects were measured using a self-report questionnaire by indicating presence or absence of 7 symptoms as well as bothersomeness on an 11–box numerical rating scale (0 meaning symptoms were not at all bothersome and 10 meaning they were extremely bothersome).
Secondary, biomechanical, and clinical objective outcomes were straight leg raise and muscle endurance tests at baseline and 12 weeks collected by examiners who were independent of treatment delivery and masked to group assignment. Three-dimensional lumbar motion, standing postural sway, sudden load response, self-reported fear avoidance, self-efficacy, and qualitative data about patient perceptions of care were also collected and will be reported separately.
Statistical Analysis
Sample size was calculated to ensure 85% power to detect an 8–percentage point mean difference between groups in patient-rated leg pain; 8 to 11 percentage points have been recommended as a minimally important group difference in pain and disability for LBP studies. [54] We assumed an SD of 17 percentage points and 17% loss to follow-up on the basis of our latest pilot study [33] and a 0.05 level of significance for a 2–tailed test at one end point to calculate a target sample size of 96 patients per group, totaling 192.
We used an intention-to-treat approach in which patients were analyzed according to their original treatment assignment. All observed data were used in the analyses. Data analyses were done using SAS, version 9.3 (SAS Institute). All regression models included terms for site and the variables used in the minimization algorithm for treatment allocation. Dependent on the outcome variable, adjusted mean differences or odds ratios and 95% CIs between groups at weeks 12 and 52 were presented.
The primary outcome variable, patient-rated leg pain, was modeled with mixed-effects regression over baseline (the average value obtained at the 2 baseline visits) and 3, 12, 26, and 52 weeks. After assuming that group means were the same at baseline, the additional terms in the model were time (as a categorical variable) and site-bygroup and time-by-group interactions. The site-by-group interaction was removed if it was not significant at the 0.05 level. Because we tested between-group differences at 2 primary end points, we used the Bonferroni method to control for 2 tests.
Responder analyses were done for pain reduction of 50%, 75%, and 100% at the end of treatment at 12 weeks and at the 52–week follow-up. [55–57] The differences in proportions between groups were calculated for patients with data at each end point based on each criterion, and 95% CIs were based on the Wilson score method. [58]
The secondary outcome variables, patient-rated LBP scores, disability scores, SF-36 physical and mental health component scores, global improvement scores, and satisfaction scores, were analyzed with the same methods as patient-rated leg pain but without controlling for multiple testing. Two approaches were used for sensitivity analyses to examine the possible effects of missing data on the results (Appendix and Appendix Tables 1 and 2, available at www.annals.org). The ordinal categorical variable representing the number of days that patients used any medications over the past week for leg pain or LBP was analyzed at baseline and at 3, 12, 26, and 52 weeks with a proportional odds model. Generalized estimating equations using all observed data with an independent covariance structure were used to fit the model. The change in the biomechanical variables from baseline to end of treatment were evaluated by analysis of covariance.
Role of the Funding Source
This trial was funded by the U.S. Department of Health and Human Services. The funding source did not participate in the study design, data collection, analysis and interpretation of the data, or writing of this article.
RESULTS
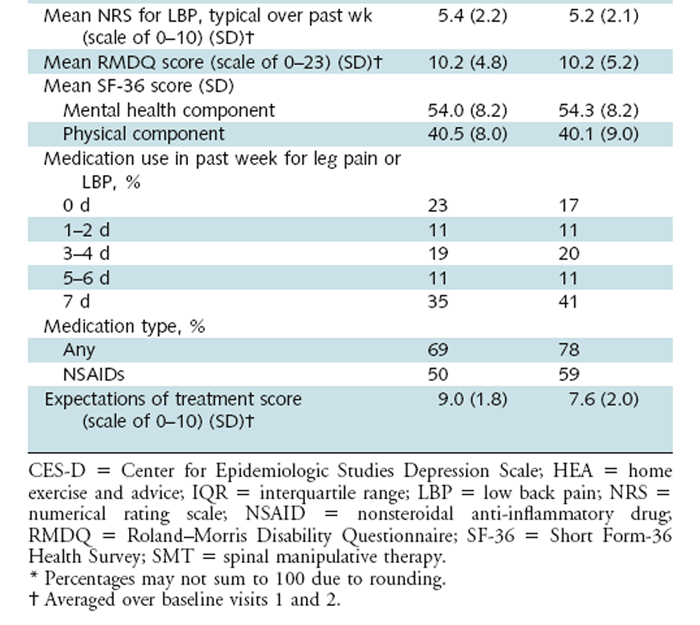
A total of 1132 patients were initially screened by phone, and 658 attended 1 or 2 clinic baseline visits. We enrolled 192 patients: 70 at the Iowa site and 122 at the Minnesota site (Figure 1). Allocation resulted in baseline comparability between groups. Table 1 summarizes the demographic and clinical characteristics of enrolled patients. Approximately 90% of the patients in both groups had chronic BRLP.
Figure 1. Study flow diagram.
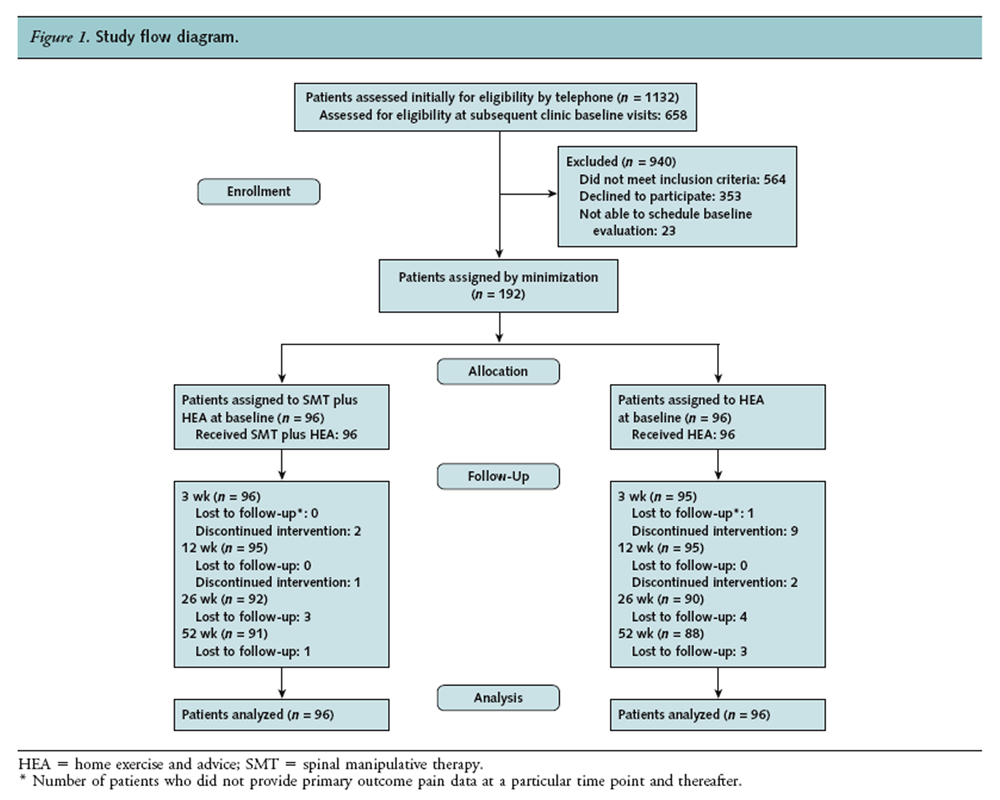
Table 1A. Baseline Characteristics*
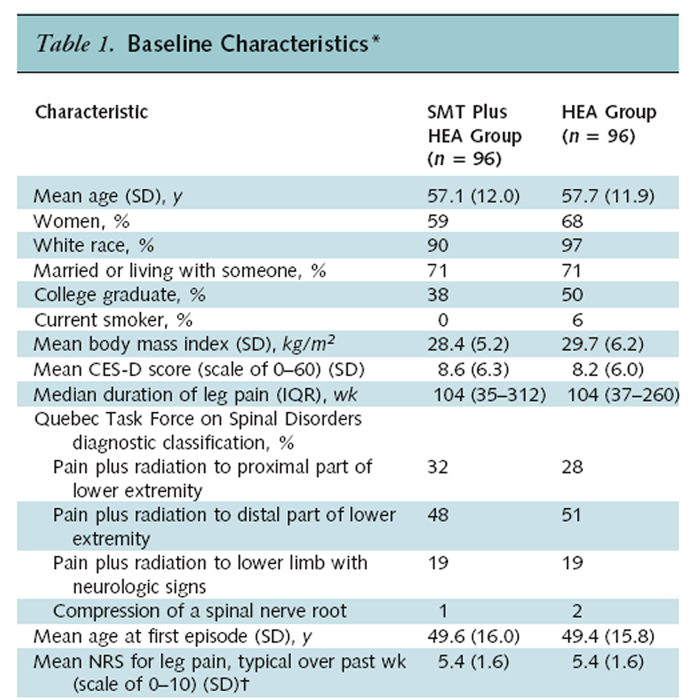
Table 1B.
Study Treatments
Of the 192 enrolled patients, 191 (99%) provided follow-up data at 12 weeks and 179 (93%) at 52 weeks. Overall, 94% of study patients attended their prescribed treatment visits: 98% in the SMT plus HEA group and 91% in the HEA group. The mean number of HEA visits was 3.8 (SD, 0.6; median, 4.0) in the SMT plus HEA group and 3.6 (SD, 1.0; median, 4.0) in the HEA group. The mean number of SMT visits was 14.6 (SD, 3.8; median, 16) in the SMT plus HEA group. Each HEA provider delivered care to approximately the same number of patients in each treatment group (range for SMT plus HEA group, 1 to 38; range for HEA group, 2 to 47); 7 chiropractors who delivered SMT plus HEA also delivered at least 1 HEA session. Patients receiving SMT plus HEA had slightly greater expectations of improvement (scale of 0 to 10) from their assigned treatment (mean, 9.0 [SD, 1.8] than the HEA group (mean, 7.6 [SD, 2.0]). One patient reported being influenced on how he answered the questionnaire at 12 weeks and indicated that it was by a person who was not involved with the study. There were no crossovers of treatment assignments during the trial. Group differences have been standardized into percentage points for all outcomes to facilitate interpretation of effect magnitude. The adjusted and unadjusted results were very similar and did not affect the conclusions.
Primary Outcome

Table 2
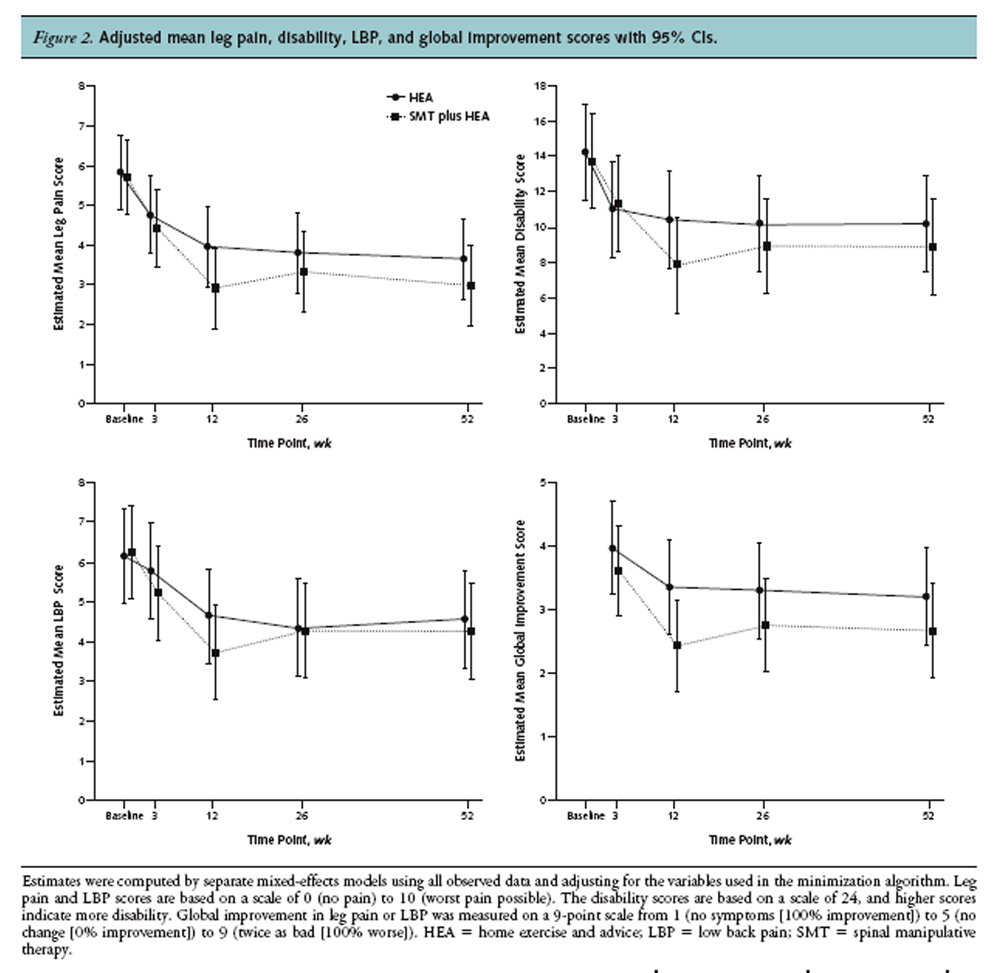
Figure 2

Table 3 On the basis of the adjusted means of the primary outcome measure, patient-rated leg pain, there was an advantage of SMT plus HEA over HEA alone after 12 weeks (10 percentage points [95% CI, 2 to 19]; P = 0.008) but not at the 52–week follow-up (7 percentage points [CI, –2 to 15]; P = 0.146) (Table 2). Figure 2 shows the adjusted group means of patient-rated leg pain over time. At 12 weeks, 37% of patients receiving SMT plus HEA had at least a 75% reduction in leg pain, compared with 19% in the HEA group. Twenty percent of patients receiving SMT plus HEA had a 100% reduction, compared with 5% in the HEA group (Table 2).
Secondary Outcomes
At 12 weeks, the adjusted means in the SMT plus HEA group were better than those in the HEA group for LBP (difference, 9 percentage points [CI, 3 to 16]; P = 0.005) (Table 2), disability (difference, 11 percentage points [CI, 5 to 17]; P < 0.001) (Table 3), SF-36 physical component score (difference, 3.4 percentage points [CI, 1.0 to 5.8]; P = 0.006) (Appendix Table 3, available at www.annals.org), global improvement (difference, 10 percentage points [CI, 14 to 5]; P = 0.02) (Table 3), and satisfaction (difference, 13 percentage points [CI, 17 to 9]; P < 0.001) (Table 3). There were no significant between-group differences for the SF-36 mental health component score at 12 weeks (Appendix Table 3).
At 52 weeks, the SMT plus HEA group sustained better global improvement (difference, 6 percentage points [CI, 11 to 1]; P = 0.02) (Table 3) and satisfaction (difference, 10 percentage points [CI, 16 to 6]; P < 0.001) (Table 3) than did the HEA group. However, no significant long-term differences were seen for LBP, disability, and SF-36 mental health and physical component scores (Tables 2 and 3 and Appendix Table 3).
The proportions of patients still using medication for leg or back pain at 12 weeks was 56% for SMT plus HEA versus 63% for HEA and 42% versus 66% at week 52, respectively. The odds of the SMT plus HEA group having fewer versus more medication days was 1.8 (CI, 1.0 to 3.1) times that for the HEA group at 12 weeks and 2.6 (CI, 1.4 to 4.7) at 52 weeks.
Adjusted group means in patient-rated LBP, disability, and global improvement over time are shown in Figure 2. The sensitivity analyses for the assumptions that data were missing at random and were not missing at random showed estimated model coefficients of consistent magnitude and in the same direction as the results reported here. All statistically significant between-group differences remained the same (Appendix).
The SMT plus HEA group had better extension trunk endurance (14.2 seconds; P = 0.001) (Appendix Table 4, available at www.annals.org) and performed better in the straight leg raise test, although it was of borderline significance (left, P = 0.054; right, P = 0.051) (Appendix Table 4). There were no between-group differences in flexion and side bridge endurance.
Nonstudy Treatments
During the 12–week intervention, 10 patients reported visits to nonstudy health care providers for their leg pain or LBP: 3 in the SMT plus HEA group (2 chiropractic visits and 1 massage therapy visit) and 7 in the HEA group (3 multiple provider visits, 2 medical physician visits, 1 chiropractic visit, and 1 massage therapy visit). By 52 weeks, 81 patients had sought additional health care since the end of the study treatment phase: 38 in the SMT plus HEA group and 43 in the HEA group.
Adverse Events

Table 4 Five serious adverse events occurred during the trial, all unrelated to study interventions (1 due to bowel obstruction in the HEA group and 4 due to anaphylaxis, sports-related trauma, heart condition, and menorrhagia in the SMT plus HEA group). No deaths occurred among the enrolled patients. Expected adverse events were mild to moderate, self-limiting, and reported by 30% of patients in the SMT plus HEA group and 42% in the HEA group (Table 4).
DISCUSSION
To our knowledge, this is one of the first adequately powered pragmatic trials to focus on patients with subacute and chronic BRLP. Both groups demonstrated improvement during the 12–week intervention. Similar patterns were seen for all outcome measures, showing that SMT plus HEA was more effective than HEA alone on all selfreport outcomes except SF-36 mental health status after 12 weeks of treatment. This short-term advantage for the SMT plus HEA group was sustained only for global improvement, medication use, and satisfaction at the 52–week follow-up.
Determination of the clinical importance of betweengroup mean differences has not been well-standardized; however, we facilitated interpretation by considering many factors in aggregate, including the magnitude of group differences (54), consistency of results, durability of treatment effect, intervention safety and tolerance, and patients’ ability to adhere to treatment. [59]
The magnitude of 10 percentage points for the group differences of the primary outcome, leg pain, translates to a medium effect size of 0.6 [60] in favor of SMT plus HEA, which is considered clinically important. Further, we saw consistent statistically significant and clinically important group differences for nearly all other outcomes in the short term and for some secondary outcomes in the long term in favor of SMT plus HEA, including global improvement, an important and recommended patient-centered outcome. [45, 61] Group differences in the responder analyses for patient-rated leg pain consistently favored SMT plus HEA. The SMT plus HEA group had less aggravation of leg pain. Of importance, patients receiving SMT plus HEA used less medication during the treatment phase and at the 52–week follow-up. On the basis of these factors, we consider the group differences in aggregate in this trial to be clinically important, consistently favoring SMT plus HEA over HEA alone, especially in the short term.
Various terms describe radiating leg pain associated with back pain (such as radiculopathy, sciatica, and BRLP). There is a need for consensus on the classification and definition of radiating leg pain to facilitate comparison between studies. [62] We used the term BRLP to be consistent with the Quebec Task Force on Spinal Disorders Classification Taxonomy. [30] Back-related leg pain was defined by a constellation of symptoms characterized by radiating pain originating from the lumbar spine and traveling into the proximal or distal lower extremity with or without neurologic signs.
There is currently no first-line therapy for BRLP that is clearly supported by a strong evidence base. This is illustrated by recent systematic reviews that found insufficient evidence to confidently guide the use of prescription medication for the effective management of BRLP. [7] Further, epidural corticosteroid injections have been shown to provide only short-term relief of leg pain and disability for patients with BRLP. [8] Surgery for BRLP associated with image-verified disc herniation has been shown to be superior to conservative interventions only in the short term. [9, 63] The lack of evidence is further compounded by growing concerns about the safety of these commonly used interventions. [10–18]
Before this study, there was moderate-quality evidence that SMT is superior to sham SMT for acute BRLP in the short and long term; however, the evidence for subacute and chronic BRLP was inconclusive because of poor study quality. This evidence was based on conclusions from an earlier systematic review by our group [20], which searched MEDLINE, EMBASE, CINAHL, Index to Chiropractic Literature, Mantis, PEDro, and the Cochrane Library for all randomized trials published through July 2010. Eleven trials were identified, 8 of which included patients with subacute or chronic BLRP and none of which were considered to be at low risk of bias (for example, high-quality). We did an updated search through April 2014, using the same search strategies described previously. We identified a small randomized study of surgical candidates for chronic sciatica that found similar outcomes for spinal manipulation and surgery. [24] Because of the small sample size and lack of baseline comparability, we consider that study to be at high risk of bias. Thus, our current trial adds to the much-needed evidence base about SMT for subacute and chronic BRLP.
The trial has several strengths, including a rigorous design and interventions intended to be pragmatic in nature and reflect clinical practice, patient needs, and the best available research. Also, patients older than 65 years were included, resulting in a greater mean age than in similar studies (but with similar clinical characteristics to other trials, including primary care settings), enhancing generalizability. [64–66] The study is limited by the inability to blind patients and providers to the nature of the treatments and differentiate between the specific treatment effects and contextual (nonspecific) effects (such as patient–provider interactions). Qualitative data collection examining patients’ perspectives will shed more light on these issues and are planned for future publications. This study was not designed to assess the effectiveness of SMT alone. Although that is a worthwhile question, this trial was intentionally pragmatic in nature, comparing the relative clinical effectiveness of commonly used treatment approaches by approximating how they are delivered in practice. [67]
Given the dearth of high-quality research investigating conservative interventions for BRLP, there are several opportunities for future research, including those that directly compare manual therapy with commonly used medical treatments and address cost-effectiveness. Further qualitative studies would be useful in identifying potential mediators and moderators of outcome to aid in individualizing treatments to best meet the preferences and abilities of patients with BRLP.
For patients with subacute and chronic BRLP, SMT in addition to HEA is a safe and effective conservative treatment approach, resulting in better short-term outcomes than HEA alone.
Acknowledgment:
The authors thank the coinvestigators at both sites for their collaboration to develop and analyze the biomechanical objective outcome measures and qualitative data, which will be reported elsewhere. The authors also thank the research patients, clinicians, therapists, and staff for the successful conduct of this trial.
Grant Support:
By the Health Resources and Services Administration, U.S. Department of Health and Human Services (grant R18HP07638).
Reproducible Research Statement:
Study protocol: Available at http://chiromt.com/content/19/1/8. Statistical code: Available from Dr. Long (email, long_c@palmer.edu). Data set: Not available.
References:
Andersson GBJ.
The epidemiology of spinal disorders.
In: Frymoyer JW, Ducker TB, Hadler NM, Kostuik JP, Weinstein JN, Whitecloud TS, eds.
The Adult Spine: Principles and Practice.
New York: Raven Pr; 1997:93-141.Selim AJ, Ren XS, Fincke G, Deyo RA, Rogers W, Miller D, et al.
The importance of radiating leg pain in assessing health outcomes among patients with low back pain. Results from the Veterans Health Study.
Spine (Phila Pa 1976). 1998;23:470-4Kent PM, Keating JL.
Can we predict poor recovery from recent-onset nonspecific low back pain? A systematic review.
Man Ther. 2008;13:12-28Hill JC, Konstantinou K, Egbewale BE, Dunn KM, Lewis M, van der Windt D.
Clinical outcomes among low back pain consulters with referred leg pain in primary care.
Spine (Phila Pa 1976). 2011;36:2168-75Kongsted A, Kent P, Albert H, Jensen TS, Manniche C.
Patients with Low Back Pain Differ From Those Who Also Have Leg Pain or Signs of Nerve Root
Involvement - A Cross-sectional Study
BMC Musculoskelet Disord. 2012 (Nov 28); 13: 236Konstantinou K, Hider SL, Jordan JL, Lewis M, Dunn KM, Hay EM.
The impact of low back-related leg pain on outcomes as compared with low back pain alone: a systematic review of the literature.
Clin J Pain. 2013;29:644-54Pinto RZ, Maher CG, Ferreira ML, Ferreira PH, Hancock M, Oliveira VC, et al.
Drugs for relief of pain in patients with sciatica: systematic review and meta-analysis.
BMJ. 2012;344:e497Pinto RZ, Maher CG, Ferreira ML, Hancock M, Oliveira VC, McLachlan AJ, et al.
Epidural corticosteroid injections in the management of sciatica: a systematic review and meta-analysis.
Ann Intern Med. 2012;157:865-77Jacobs WC, van Tulder M, Arts M, Rubinstein SM, van Middelkoop M, Ostelo R, et al.
Surgery versus conservative management of sciatica due to a lumbar herniated disc: a systematic review.
Eur Spine J. 2011;20:513-22Centers for Disease Control and Prevention (CDC).
CDC grand rounds: prescription drug overdoses—a U.S. epidemic.
MMWR Morb Mortal Wkly Rep. 2012;61:10-3Manchikanti L, Pampati V, Boswell MV, Smith HS, Hirsch JA.
Analysis of the growth of epidural injections and costs in the Medicare population: a comparative evaluation of 1997, 2002, and 2006 data.
Pain Physician. 2010;13:199-212Bohnert AS, Valenstein M, Bair MJ, Ganoczy D, McCarthy JF, Ilgen MA, et al.
Association between opioid prescribing patterns and opioid overdoserelated deaths.
JAMA. 2011;305:1315-21Dunn KM, Saunders KW, Rutter CM, Banta-Green CJ, Merrill JO, Sullivan MD, et al.
Opioid prescriptions for chronic pain and overdose: a cohort study.
Ann Intern Med. 2010;152:85-92Martell BA, O’Connor PG, Kerns RD, Becker WC, Morales KH, Kosten TR, et al.
Systematic review: opioid treatment for chronic back pain: prevalence, efficacy, and association with addiction.
Ann Intern Med. 2007;146:116-27Gore M, Sadosky A, Stacey BR, Tai KS, Leslie D.
The Burden of Chronic Low Back Pain: Clinical Comorbidities, Treatment Patterns,
and Health Care Costs in Usual Care Settings
Spine (Phila Pa 1976). 2012 (May 15); 37 (11): E668–677Deshpande A, Furlan A, Mailis-Gagnon A, Atlas S, Turk D.
Opioids for chronic low-back pain.
Cochrane Database Syst Rev. 2007:CD004959Deyo RA, Mirza SK, Turner JA, Martin BI.
Overtreating Chronic Back Pain: Time to Back Off?
J Am Board Fam Med. 2009 (Jan); 22 (1): 62–68Ohrn A, Elfstro¨m J, Tropp H, Rutberg H.
What can we learn from patient claims? A retrospective analysis of incidence and patterns of adverse events after orthopaedic procedures in Sweden.
Patient Saf Surg. 2012;6:2Delitto A, George SZ, Van Dillen LR, Whitman JM, Sowa G, Shekelle P, et al;
Orthopaedic Section of the American Physical Therapy Association. Low back pain.
J Orthop Sports Phys Ther. 2012;42:A1-57Leininger B, Bronfort G, Evans R, Reiter T.
Spinal manipulation or mobilization for radiculopathy: a systematic review.
Phys Med Rehabil Clin N Am. 2011;22:105-25Hahne AJ, Ford JJ, McMeeken JM.
Conservative management of lumbar disc herniation with associated radiculopathy: a systematic review.
Spine (Phila Pa 1976). 2010;35:E488-504Luijsterburg PA, Verhagen AP, Ostelo RW, van Os TA, Peul WC, Koes BW.
Effectiveness of conservative treatments for the lumbosacral radicular syndrome: a systematic review.
Eur Spine J. 2007;16:881-99Petersen T, Larsen K, Nordsteen J, Olsen S, Fournier G, Jacobsen S.
The McKenzie Method Compared with Manipulation When Used
Adjunctive to Information and Advice in Low Back Pain Patients
Presenting with Centralization or Peripheralization:
A Randomized Controlled Trial
Spine (Phila Pa 1976) 2011 (Nov 15); 36 (24): 1999-2010McMorland G, Suter E, Casha S, du Plessis SJ, Hurlbert RJ.
Manipulation or Microdiskectomy for Sciatica?
A Prospective Randomized Clinical Study
J Manipulative Physiol Ther. 2010 (Oct); 33 (8): 576–584Albert HB, Manniche C.
The efficacy of systematic active conservative treatment for patients with severe sciatica: a single-blind, randomized, clinical, controlled trial.
Spine (Phila Pa 1976). 2012;37:531-42Oliveira VC, Ferreira PH, Maher CG, Pinto RZ, Refshauge KM, Ferreira ML.
Effectiveness of self-management of low back pain: systematic review with meta-analysis.
Arthritis Care Res (Hoboken). 2012;64:1739-48Fritz JM, Koppenhaver SL, Kawchuk GN, Teyhen DS, Hebert JJ, Childs JD.
Preliminary Investigation of the Mechanisms Underlying the Effects of Manipulation:
Exploration of a Multivariate Model Including Spinal Stiffness,
Multifidus Recruitment, and Clinical Findings
Spine (Phila Pa 1976). 2011 (Oct 1); 36 (21): 1772-1781Pickar JG, Bolton PS.
Spinal Manipulative Therapy and Somatosensory Activation
J Electromyogr Kinesiol. 2012 (Oct); 22 (5): 785–794Schulz CA, Hondras MA, Evans RL, Gudavalli MR, Long CR, Owens EF.
Chiropractic and Self-care for Back-related Leg Pain: Design of a Randomized Clinical Trial
Chiropractic & Manual Therapies 2011 (Mar 22); 19: 8Scientific approach to the assessment and management of activity-related spinal disorders.
A monograph for clinicians. Report of the Quebec Task Force on Spinal Disorders.
Spine (Phila Pa 1976). 1987;12:S1-59Taves DR.
Minimization: a new method of assigning patients to treatment and control groups.
Clin Pharmacol Ther. 1974;15:443-53Bronfort G, Evans RL, Anderson AV, Schellhas KP, Garvey TA, Marks RA, et al.
Nonoperative Treatments for Sciatica: A Pilot Study for a Randomized Clinical Trial
J Manipulative Physiol Ther. 2000 (Oct); 23 (8): 536–544Bronfort G, Evans R, Maiers M, Anderson AF.
Spinal Manipulation, Epidural Injections, and Self-care for Sciatica:
A Pilot Study for a Randomized Clinical Trial
J Manipulative Physiol Ther. 2004 (Oct); 27 (8): 503–508Bronfort G, Maiers MJ, Evans RL, Schulz CA, Bracha Y, Svendsen KH, et al.
Supervised Exercise, Spinal Manipulation, and Home Exercise for
Chronic Low Back Pain: A Randomized Clinical Trial
Spine J. 2011 (Jul); 11 (7): 585–598Engers A, Jellema P, Wensing M, van der Windt DA, Grol R, van Tulder MW.
Individual patient education for low back pain.
Cochrane Database Syst Rev. 2008:CD004057Evans RL, Maiers MJ, Bronfort G.
What Do Patients Think? Results of a Mixed Methods Pilot Study Assessing
Sciatica Patients' Interpretations of Satisfaction and Improvement
J Manipulative Physiol Ther. 2003 (Oct); 26 (8): 502–509National Board of Chiropractic Examiners.
Practice Analysis of Chiropractic 2010
Greeley, CO: National Board of Chiropractic Examiners; 2010:1-236Lawrence DJ, Meeker W, Branson R, Bronfort G, Cates JR, Haas M, Haneline M et al.
Chiropractic Management of Low Back Pain and Low Back-Related Leg Complaints:
A Literature Synthesis
J Manipulative Physiol Ther 2008 (Nov); 31 (9): 659–674Seffinger MA, Najm WI, Mishra SI, Adams A, Dickerson VM, Murphy LS, et al.
Reliability of spinal palpation for diagnosis of back and neck pain: a systematic review of the literature.
Spine (Phila Pa 1976).McKenzie R.
Treat Your Own Back. 7th ed.
Waikanae, New Zealand: Spinal Publications; 1997.McGill SM.
Developing the exercise program.
In: McGill S, ed. Low Back Disorders: Evidence-Based Prevention and Rehabilitation. 2nd ed.
Champaign, IL: Human Kinetics; 2002:239-57.McGill S.
Building better rehabilitation programs for low back injuries.
In: McGill S, ed. Low Back Disorders: Evidence-Based Prevention and Rehabilitation.
2nd ed. Champaign, IL: Human Kinetics; 2002:205-22.Cherkin DC, Deyo RA, Street JH, Hunt M, Barlow W.
Pitfalls of patient education. Limited success of a program for back pain in primary care.
Spine (Phila Pa 1976). 1996;21:345-55Burton AK, Waddell G, Tillotson KM, Summerton N.
Information and advice to patients with back pain can have a positive effect. A randomized controlled trial of a novel educational booklet in primary care.
Spine (Phila Pa 1976). 1999;24:2484-91Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, et al;
IMMPACT. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations.
Pain. 2005;113:9-19Jaeschke R, Singer J, Guyatt GH.
A comparison of seven-point and visual analogue scales. Data from a randomized trial.
Control Clin Trials. 1990;11:43-51Jensen MP, Karoly P, Braver S.
The measurement of clinical pain intensity: a comparison of six methods.
Pain. 1986;27:117-26Roland M, Morris R.
A study of the natural history of low-back pain. Part II: development of guidelines for trials of treatment in primary care.
Spine (Phila Pa 1976). 1983;8:145-50Roland M, Morris R.
A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain.
Spine (Phila Pa 1976). 1983;8:141-4Patrick DL, Deyo RA, Atlas SJ, Singer DE, Chapin A, Keller RB.
Assessing health-related quality of life in patients with sciatica.
Spine (Phila Pa 1976). 1995;20:1899-908McHorney CA, Ware JE Jr, Raczek AE.
The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs.
Med Care. 1993;31:247-63Ware JE Jr, Gandek B.
Overview of the SF-36 Health Survey and the International Quality of Life Assessment (IQOLA) Project.
J Clin Epidemiol. 1998;51:903-12Bronfort G, Evans R, Anderson AV, Svendsen KH, Bracha Y, Grimm RH.
Spinal Manipulation, Medication, or Home Exercise With Advice for Acute
and Subacute Neck Pain: A Randomized Trial
Annals of Internal Medicine 2012 (Jan 3); 156 (1 Pt 1): 1–10Bombardier C, Hayden J, Beaton DE.
Minimal clinically important difference. Low back pain: outcome measures.
J Rheumatol. 2001;28:431-8Fritz JM, Hebert J, Koppenhaver S, Parent E.
Beyond minimally important change: defining a successful outcome of physical therapy for patients with low back pain.
Spine (Phila Pa 1976). 2009;34:2803-9Ostelo RW, Deyo RA, Stratford P, Waddell G, Croft P, Von Korff M, et al.
Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change.
Spine (Phila Pa 1976). 2008;33:90-4Guyatt GH, Juniper EF, Walter SD, Griffith LE, Goldstein RS.
Interpreting treatment effects in randomised trials.
BMJ. 1998;316:690-3Newcombe RG.
Interval estimation for the difference between independent proportions: comparison of eleven methods.
Stat Med. 1998;17:873-90Dworkin RH, Turk DC, McDermott MP, Peirce-Sandner S, Burke LB, Cowan P, et al.
Interpreting the clinical importance of group differences in chronic pain clinical trials: IMMPACT recommendations.
Pain. 2009;146:238-44Cohen J.
Statistical Power Analysis for the Behavioral Sciences. 2nd ed.
Hillsdale, NJ: Lawrence Erlbaum Associates; 1988.Evans R, Bronfort G, Maiers M, Schulz C, Hartvigsen J.
"I Know It's Changed": A Mixed-methods Study of the Meaning of Global Perceived Effect
in Chronic Neck Pain Patients
European Spine Journal 2014 (Apr); 23 (4): 888–897Lin CW, Verwoerd AJ, Maher CG, Verhagen AP, Pinto RZ, Luijsterburg PA, et al.
How is radiating leg pain defined in randomized controlled trials of conservative treatments in primary care? A systematic review.
Eur J Pain. 2014; 18:455-64Lequin MB, Verbaan D, Jacobs WC, Brand R, Bouma GJ, Vandertop WP, et al;
Leiden-The Hague Spine Intervention Prognostic Study Group. Surgery versus prolonged conservative treatment for sciatica: 5-year results of a randomised controlled trial.
BMJ Open. 2013;3Nyiendo J, Haas M, Goldberg B.
Pain, Disability, and Satisfaction Outcomes and Predictors of Outcomes:
A Practice-based Study hronic Low Back Pain Patients
Attending Primary Care and Chiropractic Physicians
J Manipulative Physiol Ther. 2001 (Sep); 24 (7): 433–439Weinstein JN, Lurie JD, Tosteson TD, Skinner JS, Hanscom B, Tosteson AN, et al.
Surgical vs. nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT) observational cohort.
JAMA. 2006;296:2451-9Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Hanscom B, Skinner JS, et al.
Surgical vs. nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial.
JAMA. 2006;296:2441-50Thorpe KE, Zwarenstein M, Oxman AD, Treweek S, Furberg CD, Altman DG, et al.
A pragmatic-explanatory continuum indicator summary (PRECIS): a tool to help trial designers.
J Clin Epidemiol. 2009;62:464-75
Return to LOW BACK PAIN
Return to CHIROPRACTIC AND SCIATICA
Return to EXERCISE AND CHIROPRACTIC
Return to DISC HERNIATION & CHIROPRACTIC
Since 6-04-2016


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |