

The Use of Spinal Manipulation to Treat an
Acute on Field Athletic Injury: A Case ReportThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Can Chiropr Assoc. 2016 (Jun); 60 (2): 158–163 ~ FULL TEXT
OPEN ACCESS Sean A. Duquette, BA, DC and
Mohsen Kazemi, RN, DC, MSc., FRCCSS(C), FCCPOR(C), PhD (Candidate)
Canadian Memorial Chiropractic College.
This case describes the utilization of spinal manipulative therapy for an acute athletic injury during a Taekwondo competition. During the tournament, an athlete had a sudden, non-traumatic, ballistic movement of the cervical spine. This resulted in the patient having a locked cervical spine with limited active motion in all directions. The attending chiropractor assessed the athlete, and deemed manipulation was appropriate. After the manipulation, the athlete's range of motion was returned and was able to finish the match. Spinal manipulation has multiple positive outcomes for an athlete with an acute injury including the increase of range of motion, decrease in pain and the relaxation of hypertonic muscles. However, there should be some caution when utilizing manipulation during an event.
In the article the authors propose four criteria that should be met before utilizing manipulation for an acute, in competition, athletic injury. These include the lack of red flags, limited time for the intervention, preexisting doctor-patient relationship and the athlete has experience receiving spinal manipulation. Clinicians should be aware that manipulation may be an effective tool to treat an acute in competition athletic injury. The criteria set out in the article may help a practitioner decide if manipulation is a good option for them.
Key indexing terms: chiropractic, spinal manipulation, athlete, competition, sideline
From the FULL TEXT Article:
Introduction
Spinal manipulative therapy (SMT) is a treatment modality that has been utilized for centuries with written explanations dating as far back as 460–385 BCE by Hippocrates. [1] There are numerous theoretical mechanisms of action for SMT. [2–4] These theories are based around three major concepts: the biomechanical effects, the muscular reflexogenic effects and the neurophysiological effects. [1] In addition, SMT also appears to have systemic effects on the body. [5] SMT have been demonstrated to be effective for the treatment of numerous conditions; research has consistently demonstrated its effectiveness for neck and low back pain. [6, 7] It has also been shown that SMT may have positive effects on pain and injury in the extremities. [8, 9] However, with this knowledge, there is limited evidence of the use of SMT during a sporting event to treat an acute injury.
Taekwondo is a martial art originating from Korea. Currently it is practiced throughout the world and has been an Olympic sport since 2000. Taekwondo competition is divided into two different categories: Poomsae (patterns) and sparring. At the highest levels sparring contests consist of three two-minute rounds with a one minute rest period between. Points are accrued through landing punches to the trunk or kicks to the trunk and head. If an injury is sustained during the competition the referee must suspend the match to allow the athlete’s doctor to treat the issue. If the athlete cannot return to the match within one minute; the opposing athlete is declared the winner. [1]
The goal of this case study is to demonstrate the utilization of SMT during competition and to discuss the times when it may be appropriate.
Case presentation
During a national level Taekwondo match, one of the competitors had a sudden, quick, non-traumatic neck movement and experienced locking in the cervical spine. There was no blow delivered to the head or fall to the mat that would have elicited an immediate change in her cervical range of motion (ROM). She was immediately attended to by her chiropractor who was working in the role of medical responder during the competition.
Taekwondo matches have a strict one-minute time limit for the medical responder to assess, provide any treatment and decide if the athlete can continue the match. The chiropractor had witnessed the mechanism of injury and completed an abbreviated history around the complaint. The chiropractor had also had previous encounters with the patient and knew of their medical history. The chiropractor then assessed the athlete for any red flags (referral pain, headaches, dizziness, visual disturbances, and unusual acute and sharp pain) and found a decreased ROM through visual estimation, hypertonic cervical para-spinal musculature bilaterally and restricted cervical segments with point tenderness reproducing the athlete’s chief complaint.
Based on the mechanism of injury, the lack of red flags, the previous doctor/ patient relationship with the fighter and the assessment results, the chiropractor completed a standing cervical spine manipulation upon the athlete’s verbal consent. Due to the previous doctor/patient interactions the athlete was informed of the risks associated with spinal manipulation. The patient had previously signed an informed consent six months prior for a similar neck complaint.
This was treated with SMT, in addition to other treatment modalities, to which the patient had responded positively. After the manipulation, the fighter’s ROM was immediately improved compared to pre-manipulation ranges, and she was able to continue and successfully complete the match. After the match, the chiropractor assessed the athlete further to ensure their safety. The athlete reported no pain after the completion of the match and continued to compete on the same day. After the encounter, the chiropractor recorded the entire encounter, which included the competition number, the time and date, mechanism of injury, physical findings and treatment rendered.
Discussion
In this case, the athlete experienced an immediate reduction in her cervical ROM after a sudden, ballistic, non-traumatic movement. The athlete most likely suffered from an entrapped cervical facet meniscoid. One of the older biomechanical theories behind the mechanism of SMT is the release of intra-articular meniscoids, synovial folds or plicas. [3, 11] Intra-articular meniscoids have been found in the majority (86%) of the cervical spine facet joints. [12]
Previous literature has described three types of synovial folds that include type I, which are adipose tissue and crescent shaped, type II which are elliptical shaped and project into the facet joint and type III which are made of fibrous tissue and are ragged shaped. [13] Additionally, it has previously been demonstrated that the synovial folds contain nociceptive fibres which allow them to be pain generators. [14] In addition to the nociceptors, cervical spine facet joints contain type I, type II and type III mechanoreceptors. [15]
During cervical spine movement, the facets will move relative to one another. The facet’s motion will take the intra-articular meniscoid to the extreme ranges of motion. As the facets return to their neutral position, the meniscoid can remain trapped in the peripheries of the joint cavity. Pain will then result due to pressure and irritation applied to the trapped meniscoid. [3]
SMT is suspected to gap the facets, therefore reducing the impaction on the trapped meniscoid and allowing it to return to its normal position. [3] This will allow the joint to regain full range of motion. Due to the absence of a traumatic event, the quick cervical motion and decreased range of motion, it is the authors’ belief that this is the explanation for the effectiveness of SMT during the case presented. However, other differential diagnoses could include a facet joint irritation or a strain to the surrounding musculature.
There are other theoretical models where SMT may be beneficial in treating acute injuries in athletes during competition. Other effects of SMT beyond that of restoring range of motion can include hypoalgesic effects as well as muscle reflex effects. [15–19] The hypoalgesic effects of SMT can be attributed to the gate-control theory of pain. [2, 4] The facet joint capsule and surrounding musculature have numerous proprioceptors in the form of muscle spindles and type I and type II afferents. [2, 4] With SMT, there is a dynamic stretch to the tissue that will cause an increase in afferent discharge from these receptors. [19–21]
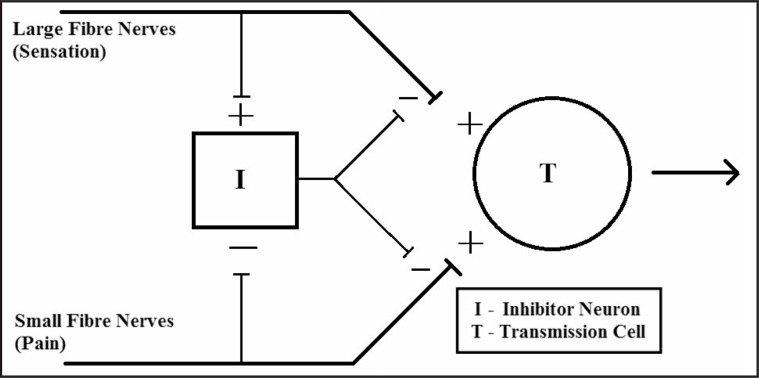
Figure 1 This increase in afferent input will attenuate the pain sensation at the dorsal horn, thereby creating a hypoalgesic effect. [2] (Figure 1) The muscle-reflexogenic effects of SMT are believed to occur through the effects on the muscle spindles surrounding the joint. As with the gate-control theory, during the act of the spinal manipulation, there is an increase in the afferent output from the surrounding muscle spindles. [19–21] Directly after SMT, the muscle spindles become silent for a short period. [19, 21] After this silent period, the spindles return to firing at their appropriate rate, which can cause a relaxation of the surrounding muscles.

Table 1 While there are possible benefits to utilizing SMT for acute injuries during a sporting event, it should be used sparingly. In the authors’ opinion, if the medical practitioner decides to utilize SMT the following criteria should be met (Table 1): the practitioner has assessed for any red flags, there is limited time for the intervention, there is a pre-existing relationship between patient and practitioner, the patient is familiar with spinal manipulation, and the rules surrounding informed consent have been satisfied. These recommendations will allow the doctor assess the patient and deliver a treatment in a circumstance where the patient is informed of the associated risks.
As a medical practitioner, the primary goal would be to do no harm, therefore, ruling out red flags would be a priority when assessing a patient with or without the intent of using SMT. A good red-flag screen for the cervical spine would include utilizing the Canadian C-Spine Rules. [22, 23] These rules were originally designed to screen if a patient would require a radiograph, however, they can help to recognize if there is a traumatic incident or if there are concerning signs and symptoms.
A dangerous mechanism, which applies to sporting events, is defined as either a fall from greater than 3 feet, an axial load to the head, or a bicycle accident. [22, 23] Other tests which can be used to rule out potentially severe injuries include the absence of midline cervical spine tenderness, absence of parathesias in the extremities and the ability of the patient to actively rotate their head 45° in both directions. [22, 23]

Table 2 It is important to be aware of the grading of neck pain and if the diagnosis is grade 3 neck pain (Table 2) or higher this would require additional assessment with removal from the competition. [24] If the athlete is presenting with a complaint in another area besides the cervical spine, other red flags should be considered. For example, red flags for low back spinal fractures include older age, prolonged steroid use, severe trauma and contusion or abrasion at the location. [25]
In addition to the red flags, a chiropractor would also need to assess for the possibility of a concussion as they can occur with impulsive forces transmitted to the head. [26] In the case of a concussion, there needs to be an immediate assessment for any cervical spine injuries as well as observations for any more serious pathologies such as intra-cranial bleeds. [26]
The chiropractor will assess for those changes during the on field assessment including looking for changes in memory, mood and communication. Utilization of the Maddocks Score allows for a quick assessment of these aspects. This test allows for quick assessment of the athletes’ orientation to time, location and ability to communicate. It is five questions asking if the athlete knows where they are, the time in the competition, who scored last, what was the last team they played and if the team won the last game. [26]
After assessing for red flags, the amount of time available for intervention would have an impact on the practitioner’s decision to utilize SMT. Certain sports have limited time periods to assess the athlete and make a decision to continue the match (Taekwondo) while other sports can force a team to compete short-handed if the assessment takes a prolonged period of time (soccer). In these time-limited scenarios, SMT may be the only practical option available to the practitioner to treat the athlete in order for the athlete to continue to compete. However, in situations where immediate return is not necessary, the practitioner should bring the athlete to the side of the field for further assessment. At this point, they can utilize the treatment options which they feel will be most effective for the patient’s presenting compliant and preferences. If the chiropractor is unsure or concerned about the use of SMT other treatment options can include the use of soft tissue techniques (such as ART®, cross-friction, or instrumented assisted soft tissue techniques), acupuncture or other physical modalities to help return the athlete to sport.
Finally, before a practitioner utilizes SMT on the field, the patient should have a familiarity with both the chiropractor and receiving SMT. This familiarity must include the athlete’s past medical history, relevant family history, previous response to treatment (including SMT) and allows for comparison of the current complaint to previous episodes. This information will allow the chiropractor to abbreviate their history to focus on the current complaint. Additionally, the chiropractor can assess if this is a re-occurring condition or a new complaint, which, in the case of the latter, they should be more cautious with before proceeding with on field care. Also, previous research has demonstrated that there is a variable muscle activity response when the spine is manipulated. [27] Therefore, if an athlete has never had a spinal manipulation, receiving their first manipulation on the field may have unexpected side effects.
Another key aspect of the necessity of a pre-existing relationship between the practitioner and the athlete is based around the issues involving informed consent. For the patient to receive SMT, they must be fully informed of the risks associated with the treatment. A previous doctor/patient relationship ensures that the patient is aware of these risks and can properly consent to the treatment. This previous relationship will allow the chiropractor to have standardized written consent from the patient as well. It is important that the chiropractor completes a new informed consent form with the patient periodically to ensure that the patient is still aware of the risks associated with the treatment. Even with a previous history of spinal manipulation of the injured area and a doctor/patient relationship, a verbal consent to provide SMT on the field with brief explanation is still necessary and prudent. However, if no previous relationship has been established, there may not be adequate time to inform the patient, and, under these circumstances, SMT should not be delivered.
Summary
This case demonstrates the use of SMT for an acute injury during a sporting event. SMT can have the ability to decrease pain, increase range of motion and decrease muscle spasm. While it may have its benefits, SMT should be used sparingly for on-field treatment. For SMT to be utilized, there needs to be a limited time to treat, the absence of any red flags, and, finally, the athlete needs to be comfortable and familiar with the proposed manipulation, have a pre-existing relationship with the practitioner and consent to the treatment.
Footnotes
The patient has provided written consent for publication.
Declaration: No external sources of funding were provided. The authors have no conflicts of interest to declare regarding this paper of the material described therein.
References
Pettman E.
A history of manipulative therapy.
J Man Manip Ther. 2007;15(3):165–174Potter L, McCarthy C, Oldham J.
Physiological effects of spinal manipulation: a review of proposed theories.
Phys Ther Rev. 2005;10(3):163–170Evans DW.
Mechanisms and Effects of Spinal High-velocity, Low-amplitude
Thrust Manipulation: Previous Theories
J Manipulative Physiol Ther 2002 (May); 25 (4): 251–262Pickar JG.
Neurophysiological Effects of Spinal Manipulation
Spine J (N American Spine Society) 2002 (Sep); 2 (5): 357–371Bolton PS, Budgell B.
Visceral Responses to Spinal Manipulation
J Electromyogr Kinesiol. 2012 (Oct); 22 (5): 777–784Hurwitz EL, Carragee EJ, van der Velde G, Carroll LJ, Nordin M, Guzman J, et al.
Treatment of Neck Pain: Noninvasive Interventions:
Results of the Bone and Joint Decade 2000–2010
Task Force on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S123–152Bronfort G, Maiers MJ, Evans RL, Schulz CA, Bracha Y, Svendsen KH, Grimm RH, Jr.:
Supervised Exercise, Spinal Manipulation, and Home Exercise for Chronic Low Back Pain:
A Randomized Clinical Trial
Spine J. 2011 (Jul); 11 (7): 585–598Muth S, Barbe MF, Lauer R, McClure P.
The effects of thoracic spine manipulation in subjects with signs of
rotator cuff tendinopathy.
J Ortho Sport Phys Ther. 2012;42(12):1005–1016Haik MN, Alburquerque-Sendín F, Silva CZ, Siqueira-Junior AL, Ribeiro IL, Camargo PR.
Scapular kinematics pre–and post–thoracic thrust manipulation in individuals
with and without shoulder impingement symptoms: A randomized controlled study.
J Ortho Sport Phys Ther. 2014;44(7):475–487World Taekwondo Federation.
World taekwondo federation competition rules & interpretation in force
as of January 1, 2015. Seongnam, Korea: World Taekwondo Federation; 2014.
http://www.worldtaekwondofederation.net/
(accessed 6 June 2015)Sandoz R.
Some physical mechanisms and effects of spinal adjustments.
Ann Swiss Chiro Assoc. 1976;6(2):91–142Farrell SF, Osmotherly PG, Cornwall J, Rivett DA.
The Anatomy and Morphometry of Cervical Zygapophyseal Joint Meniscoids
Surg Radiol Anat. 2015 (Sep); 37 (7): 799–807Inami S, Kaneoka K, Hayashi K, Ochiai N.
Types of synovial fold in the cervical facet joint.
J Ortho Sci. 2000;5(5):475–480Inami S, Shiga T, Tsujino A, Yabuki T, Okado N, Ochiai N.
Immunohistochemical demonstration of nerve fibers in the synovial fold
of the human cervical facel joint.
J Ortho Res. 2001;19(4):593–596McLain RF.
Mechanoreceptor endings in human cervical facet joints.
Iowa Orthop J. 1993;13:149–154Vernon, H.
Qualitative Review of Studies of Manipulation-induced Hypoalgesia
J Manipulative Physiol Ther 2000 (Feb); 23 (2): 134–138Millan M, Leboeuf-Yde C, Budgell B, Amorim MA.
The Effect of Spinal Manipulative Therapy on Experimentally Induced Pain:
A Systematic Literature Review
Chiropractic & Manual Therapies 2012 (Aug 10); 20 (1): 26Coronado RA, Gay CW, Bialosky JE, Carnaby GD, Bishop MD, George SZ.
Changes in Pain Sensitivity Following Spinal Manipulation: A Systematic Review
and Meta-analysis
J Electromyogr Kinesiol. 2012 (Oct); 22 (5): 752–767Pickar JG, Kang Y.
Paraspinal muscle spindle responses to the duration of a spinal manipulation
under force control.
J Manipulative Physiol Ther. 2006;29(1):22–31Cao D, Reed WR, Long CR, Kawchuk GN, Pickar JG.
Effects of thrust amplitude and duration of high-velocity, low-amplitude
spinal manipulation on lumbar muscle spindle responses to vertebral position and movement.
J Manipulative Physiol Ther. 2013;36(2):68–77Pickar JG, Bolton PS.
Spinal Manipulative Therapy and Somatosensory Activation
J Electromyogr Kinesiol. 2012 (Oct); 22 (5): 785–794Stiell IG, Clement CM, McKnight RD, Brison R, Schull MJ, Rowe BH, et al.
The Canadian C-spine rule versus the NEXUS low-risk criteria in patients with trauma.
N Engl J Med. 2003;349(26):2510–2518Bandiera G, Stiell IG, Wells GA, Clement C, De Maio V, Vandemheen KL, et al.
The Canadian C-spine rule performs better than unstructured physician judgment.
Ann Emerg Med. 2003;42(3):395–402Guzman J, Hurwitz EL, Carroll LJ, et al.
A New Conceptual Model Of Neck Pain: Linking Onset, Course, And Care Results of the
Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S14–23Downie A, Williams CM, Henschke N, Hancock MJ, Ostelo RW, de Vet HC, et al.
Red flags to screen for malignancy and fracture in patients with
low back pain: systematic review.
BMJ. 2013;347:f7095McCrory P, Meeuwisse WH, Aubry M, Cantu B, Dvorak J, Echemendia RJ, et al.
Consensus statement on concussion in sport: the 4th International
Conference on Concussion in Sport held in Zurich, November 2012.
Br J Sports Med. 2013;47(5):250–Lehman GJ, McGill SM.
Spinal manipulation causes variable spine kinematic and trunk muscle
electromyographic responses.
Clin Biomech. 2001;16(4):293–299Dickenson AH.
Gate Control Theory of pain stands the test of time.
Br J Anaesth. 2002;88(6):255–257
Return to CASE STUDIES
Since 8-17-2016


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |