

Cervicogenic Dizziness This section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Oxford Medical Case Reports 2019 (Dec 9); 2019 (11): 476–478 ~ FULL TEXT
OPEN ACCESS Eric Chun Pu Chu, Wui Ling Chin, and Amiya Bhaumik
New York Chiropractic & Physiotherapy Center,
New York Medical Group
Cervical muscles have numerous connections with vestibular, visual and higher centres, and their interactions can produce effective proprioceptive input. Dysfunction of the cervical proprioception because of various neck problems can alter orientation in space and cause a sensation of disequilibrium. Cervicogenic dizziness (CGD) is a clinical syndrome characterized by the presence of dizziness and associated neck pain in patients with cervical pathology. Here, we report a 24–year-old female, who was diagnosed with CGD based on the correlating episodes of neck pain and dizziness. Both symptoms improved with targeted chiropractic adjustment and ultrasound therapy. CGD is a seemingly simple complaint for patients, but tends to be a controversial diagnosis because there are no specific tests to confirm its causality. For CGD to be considered, an appropriate management for the neck pain should not be denied any patient.
KEYWORDS: cervical proprioception; cervicogenic dizziness; chiropractic adjustment; neck pain
From the FULL TEXT Article:
INTRODUCTION
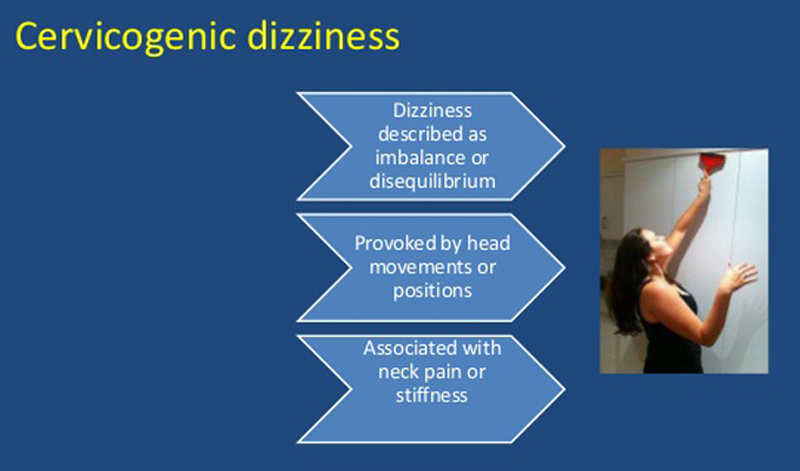
Cervicogenic dizziness (CGD) is a syndrome of neck pain accompanied by an illusory sensation of motion and disequilibrium due to neck pathology. [1] Current theory suggests that episodes of dizziness are due to disturbed sensory afferents from the neck, leading to a sensory mismatch between cervical, visual and vestibular inputs. [1, 2] The diagnosis is dependent upon the correlating symptoms of disequilibrium and dizziness with neck pain and excluding other vestibular disorders. [1] Given that cervical proprioception disturbed by persistent neck pain can affect spatial orientation, an appropriate treatment for the neck pain should not be denied any CGD patient. A number of clinical studies including randomized controlled trials [3–6] support the efficacy of manual therapy for CGD.
CASE REPORT
A 24–year-old female complained of intermittent neck pain and dizziness triggered by head motion for 2 years. When neck pain was severe, she usually experienced dizziness which could be exacerbated by head movement. She denied any tinnitus, aural fullness or hearing loss. There was no history of head injury, vestibular or systemic disorder. Brain magnetic resonance (MR) imaging and cervicocerebral MR angiography excluded intracranial pathology, vessel stenosis, aneurysm, vascular malformation or dural sinus thrombosis. Caloric irrigation and ocular vestibular evoked myogenic potential test revealed normal responses on both sides. The patient was prescribed ibuprofen and acetaminophen, with only partial relief of her symptoms.
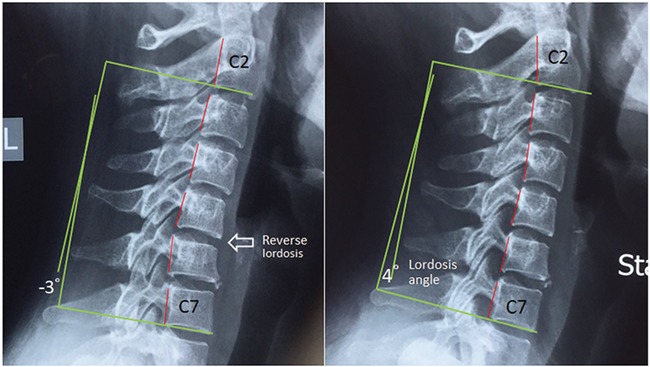
Figure 1 On initial evaluation, the patient presented with a guarded neck posture and forward head carriage. She rated her peak pain intensity to be 8/10 on the Numeric Pain Scale (PNS) and scored 60 points on the Dizziness Handicap Inventory (DHI > 54 denotes a severe handicap). Joint mobility was assessed, showing restriction at C5/6 and C6/C7 levels, cervical range of motion was limited and painful at 10° extension (normal >60°) and 30° of right rotation (normal >80°). Spinal palpation revealed tenderness at the cervicothoracic junction. Cervical radiographs showed a picture of degenerative spondylosis of the lower cervical spine, with osteophytes at posterior C5 and 6; C7/T1 disc-space narrowing; and reverse cervical lordosis (Figure 1). Based on the symptoms of dizziness relating with neck pain, and the exclusion of systemic, neurological and vestibular disorders, the patient was given a diagnosis of CGD.
The patient was treated with cervical adjustment and thermal ultrasound therapy three times a week, with emphasis on restoring mobility to stiff joints and relieving muscle tightness in the neck. At the end of 4 weeks, the patient reported that her neck pain went away, and the symptoms of dizziness had concurrently eliminated. Patient continued to receive chiropractic adjustment once a month for correcting forward head posture. Restoration of the cervical curvature was demonstrable on cervical radiographs at the 7–month follow-up (Fig. 1). In general, there is a statistically significant relationship between cervical pain and lordosis angle of less than 20°. [7] Currently, 18 months after the initiation of treatment, the patient remained medication-free status and was not complaining of any symptoms.
DISCUSSION
The proprioceptive inputs from the neck play an important role in head-eye coordination and postural processes. Fish do not have necks like humans do. For their orientation in space, the function of the lateral-line system is enough during swimming. [8] Their head and trunk move as a unit. With erect bipedal posture and a heavy mobile head in human beings, the interaction of the neck and trunk proprioception with the vestibular sense has reached a highly developed grade. Mere vestibular signals cannot distinguish dynamics of the head or of the whole body when the head moves on a stationary trunk. Neck proprioception, thus, provides the necessary information about head movements relative to the trunk. [8] Accordingly, neck muscles, especially in the suboccipital region, are richly endowed with spindles, which have a complex sensory and motor innervation within the muscles. [8] Furthermore, mechanoreceptive nerve endings in the facet joint capsules are also important for proprioception and pain sensation in the cervical spine. [9] The sensory input from the neck participates in perceptual functions and reflex responses, thereby interacting with signals of the vestibular and visual system to stabilize the eyes, the head and posture.
CGD has been a controversial entity since early in the 20th century because of lack of a confirmatory diagnostic test. Sustained loadings of the neck, e.g. long smartphone use, mobile gaming and desktop work, are common symptom triggers. With strong connections between cervical receptors and equilibrium function, it is apparent that degenerative or traumatic changes of the spine and problems in the neck muscles could induce distorted sensations and cause symptoms of disequilibrium. [1] To diagnose CGD, masquerading pathologies must be identified and excluded. The list of differential diagnosis may include benign paroxysmal positional vertigo, perilymphatic fistula, labyrinthine concussion, migraine-related vertigo and central or peripheral vestibular dysfunction. [1] Once vestibular and neurovascular pathologies have been ruled out, the diagnosis of CGD should be established by a correlation between dizziness and the cervical spine.
A potential mechanism of CGD would have to be based on altered upper cervical somatosensory input associated with neck problems. If the firing characteristics (the symmetricity) of the cervical somatosensors alter as a consequence of neck pain, a sensory mismatch between vestibular and cervical inputs would be expected to result in CGD. Physiological studies have shown that small flexion of the upper cervical joints can cause major changes in firing rate of the spindle afferents from perivertebral muscles. [10] Clinically, the amelioration of dizziness in response to cervical traction [11] implicates that a cervical origin is more consistent with CGD than with a vestibular dysfunction.
A recent literature review emphasized the importance of identifying the constitute conditions behind a patient’s CGD, which are relevant clinically as well as for interpreting the results of the intervention trials. [12] For instance, in CGD patients with degenerative cervical spine disorders, the cause of dizziness with neck rotation could be due to the reduced vertebral blood flow, impingement of the sympathetic nerve fibres, or proprioceptive receptor dysfunction of the neck structures. If vascular compression is identified as the cause of dizziness, also seen in bow hunter’s syndrome and beauty parlor stroke syndrome, individualized vascular decompression will be required. Mechanoreceptor dysfunction can be a cause of dizziness in patients with cervical spondylosis, cervical myofascial pain syndrome and whiplash injury, in which case cervical physiotherapy and manual therapy will then be the preferred treatment modalities. [12] In subjects with orthostatic hypotension, suboccipital and paracervical neck pain (in a coat-hanger distribution) is a common symptom due to hypoperfusion in these bulky muscle groups. More caution is required to distinguish between musculoskeletal diseases and cerebrovascular conditions that require acute treatment in these populations experiencing dizziness. [13] Determining the cause of dizziness is crucial to tailoring the most appropriate treatment regimen.
Results from clinical studies [3–6] do show promise for the use of manual approaches in the treatment of Cervicogenic dizziness (CGD). The underlying mechanism for the efficacy of manual therapy includes stimulation of cervical proprioceptors and normalization of the afferent input. [14] It must be emphasized that manual therapies should be applied with great caution in patients with CGD. Ruling out neurovascular aetiologies is of utmost importance before starting the manual therapy to prevent any untoward events in CGD.
Acknowledgements
None.
Conflict of Interest statement
No conflicts of interest to declare.
Funding
No sources of funding.
References:
Wrisley DM, Sparto PJ, Whitney SL, Furman JM.
Cervicogenic dizziness: a review of diagnosis and treatment.
J Orthop Sports Phys Ther 2000;30:755–66Moustafa IM, Diab AA, Harrison DE.
The effect of normalizing the sagittal cervical configuration on dizziness, neck pain, and cervicocephalic kinesthetic sensibility: a 1-year randomized controlled study.
Eur J Phys Rehabil Med 2017;53:57–71Bronfort G, Evans R, Nelson B, Aker PD, Goldsmith CH, Vernon H.
A Randomized Clinical Trial of Exercise and Spinal Manipulation for Patients with Chronic Neck Pain
Spine (Phila Pa 1976). 2001 (Apr 1); 26 (7): 788–797Hawk C, Cambron JA, Pfefer MT.
Pilot Study of the Effect of a Limited and Extended Course of Chiropractic Care
on Balance, Chronic Pain, and Dizziness in Older Adults
J Manipulative Physiol Ther. 2009 (Jul); 32(6): 438–447Hawk C, Cambron J.
Chiropractic Care for Older Adults: Effects on Balance, Dizziness, and Chronic Pain
J Manipulative Physiol Ther. 2009 (Jul); 32 (6): 431–437Maiers M, Bronfort G, Evans R, Hartvigsen J, Svendsen K, Bracha Y, et al.
Spinal Manipulative Therapy and Exercise For Seniors with Chronic Neck Pain
Spine J. 2014 (Sep 1); 14 (9): 1879–1889McAviney J, Schulz D, Bock R, et al.
Determining the Relationship Between Cervical Lordosis and Neck Complaints
J Manipulative Physiol Ther 2005 (Mar); 28 (3): 187-193Pettorossi VE, Schieppati M.
Neck proprioception shapes body orientation and perception of motion.
Front Hum Neurosci 2014;8:895McLain RF.
Mechanoreceptor endings in human cervical facet joints.
Spine 1994;19:495–501Kulkarni V, Chandy MJ, Babu KS.
Quantitative study of muscle spindles in suboccipital muscles of human foetuses.
Neurol India 2001;49:355–9Clendaniel RA, Landel R.
Physical therapy management of cervicogenic dizziness
In: Herdman SJ, Clendaniel RA. eds.
Vestibular Rehabilitation, 4th edn.
Philadelphia: F.A. Davis Co, 2014, 597–616Devaraja K.
Approach to Cervicogenic Dizziness: A Comprehensive Review of its Aetiopathology and Management
Eur Arch Otorhinolaryngol. 2018 (Oct); 275 (10): 2421–2433Morinaka S.
Musculoskeletal diseases as a causal factor of cervical vertigo.
Auris Nasus Larynx 2009;36:649–54Kristjansson E, Treleaven J.
Sensorimotor Function and Dizziness in Neck Pain: Implications for Assessment and Management
J Orthopaedic Sports Physical Therapy 2009 (May); 39 (5): 364–377
Return to VERTIGO and/or BALANCE
Since 5-19-2018


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |