

Health Services Research Related to Chiropractic:
Review and Recommendations for Research Prioritization
by the Chiropractic ProfessionThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Manipulative Physiol Ther. 2006 (Nov); 29 (9): 707–725 ~ FULL TEXT
Robert D. Mootz, DC, Daniel T. Hansen, DC, Alan Breen, DC, PhD,
Lisa Z. Killinger, DC, Craig Nelson, DC
State of Washington,
Department of Labor and Industries,
Olympia, Washington 98504-4321, USA.
PURPOSE: This project updates a previous effort to inventory health services research conducted on chiropractic and makes recommendations for a subsequent research agenda. A qualitative review of social sciences, medical, chiropractic, and health services research literature regarding chiropractic was done with emphasis on research published since the initial health services research agenda effort in 1995. This work informed development of updated health services research recommendations.
METHODS: Literature was gathered through searches of electronic health care database retrieval systems and citation tracking. In addition to general collecting of new studies, the authors considered to what extent the 1995 research recommendations had been addressed in the new literature. A seed set of refined recommendations was formulated and initially distributed expert review and revision. The recommendations were made available for public comment and hearing at the 10th Annual Research Agenda Conference for Chiropractic in March 2005.
DISCUSSION: The past 10 years have seen numerous health service research studies related to chiropractic; however, nearly all of the research priorities identified in 1995 remain unaddressed and remain as important priorities. Thus, recommendations were reprioritized and revised to submit for open comment and hearing.
CONCLUSION: A smaller number of more concise recommendations with more specific action steps are proposed for clinical quality improvement, performing cost analyses, and assessing use barriers for chiropractic.
From the FULL TEXT Article:
Background
This effort updated a 1997 report [1] making recommendations for chiropractic health services research priorities. The current effort identified key literature for annotation, inventory, and synthesis using a combination of a search of medical and health databases from 1996 through 2004 based on key word combinations of chiropractic with health services research, use, quality assurance, and practice guidelines, among other topics along with citation tracking by the authors.
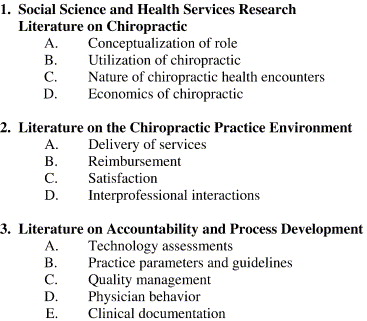
Figure 1 The original project reflected one component of a formal exercise conducted at the first annual Research Agenda for Chiropractic conference in 1995 to establish research priorities in the areas of basic science research, education research, clinical research, outcome research, and health services research, and [1-5] health service research literature was originally categorized into 3 general domains of literature related to social sciences and health services research literature, literature on chiropractic practice environments, and literature on accountability and process development (Figure 1). A companion annotated bibliography was also developed (and updated for the current project) and is available from Consortial Center for Chiropractic Research (CCCR).
Methods
1995 Health Services Research Recommendation Summary
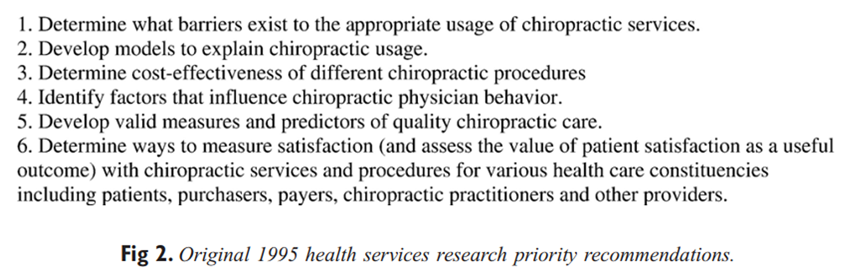
Figure 2 Six general priority areas for health services research topics were identified in 1995 with a detailed list of specific subtopics and examples of specific research questions (Figure 2). The original recommendations resulted from a grant proposal made by the Palmer Center for Chiropractic Research to the US Public Health Service, Health Resources and Services Administration, to develop a research agenda for the chiropractic profession. The center appointed a health services research team (as well as teams for each of the other research topic areas) that prepared an annotated bibliography and drafted a qualitative literature review on the topic. The team also drafted the seed research recommendations. [1]
A conference was convened in 1995 and an expert health services research panel was appointed by the Palmer Center (Davenport, Iowa) to consider the literature reviewed and the seed recommendations. The 6 voting panelists included a practicing doctor of chiropractic (DC), a chiropractic health services researcher at a chiropractic college, a medical health services researcher who had conducted chiropractic health services research, an attorney from a chiropractic trade association, a health services researcher from the Agency for Health Care Policy and Research (Rockville, Md), and a private sector health services researcher from a non–chiropractic-related health improvement foundation. The panel was chaired by a nonvoting DC employed as a health services researcher in the public sector, and several nonvoting content expert and resources were present to assist with answering questions and retrieving information for the discussion. Using a nominal group process consensus methodology, the group refined and finalized health services research recommendation.
In addition to each recommendation, the panel drafted a rationale for the recommendation and provided recommended specific logistical and technical action that would be needed to engage in research in the topic areas as well as potential groups that could conduct or facilitate the conduct of health service research.
Methodology for Updating the Health Services Research Recommendations
The process of updating the recommendations from 1995 involved identifying a team to update the previous literature review, assess the extent of progress in the literature relative to the previous recommendations, and draft new or revised seed recommendations to present for public comment via posting on the Palmer Center for Chiropractic Web page and through a hearing process at the 10th anniversary of the 1995 recommendations at the 2005 Research Agenda for Chiropractic conference.
The new health services research team included 2 participants from the 1995 team and 2 others who were not involved. An additional participant was added later to assist with literature review, retrieval, and manuscript review. A preliminary review of literature published since the original study was published was conducted using citation tracking based on the authors' knowledge of the subject area and topical literature searches using the National Library of Medicine's Pilot Health Services Research Filter Project (http://www.nlm.nih.gov/nichsr/hedges/search.html). The annotated bibliography developed for the original effort was updated with the subsequent publications and circulated among the authors.

Table 1

Table 2

Table 3 Concurrently, recommended health services research priorities developed at the first Research Agenda for Chiropractic1 were also reviewed. A scorecard was developed listing each recommendation from the 1997 report. All recommendations were rated independently by the initial 4 coauthors for research progress since 1995 and for their priority for inclusion into the 2005 recommendations (Table 1-3). The coauthors additionally noted any changes that might be needed to the 1997 recommendations. Conference calls among the authors were arranged to discuss respective (unblinded) conclusions, and an informal consensus was reached for a list of revised seed recommendations.
The seed recommendations, along with the annotated bibliography, were drawn up by the lead author for review by others and posted on the Palmer Center for Chiropractic Research Web site for public comment before the 2005 Research Agenda Conference as well. A peer review committee appointed by the Palmer Center for Chiropractic Research also reviewed the latest draft before the March 2005 meeting. The draft was available for public comment on the center's Web site. Input from the March 2005 meeting was considered as well in the development of the final 2005 recommendations.
Discussion
An Overview of Key Health Services Research Concepts, Definitions, and Issues
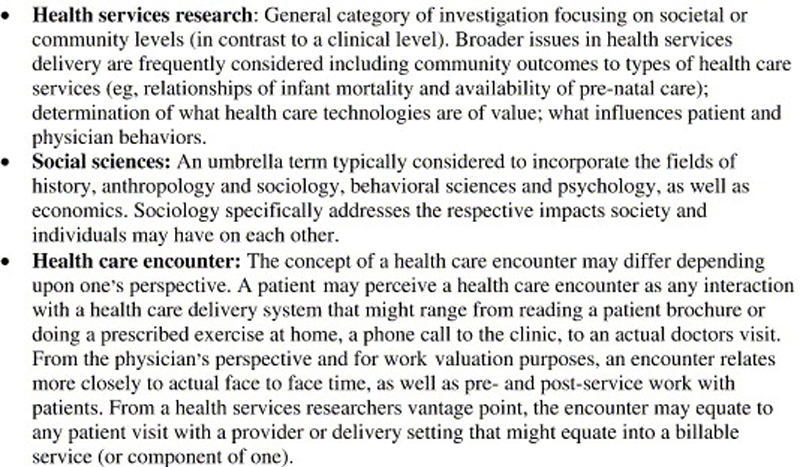
Figure 3 Health services research generally refers to a variety of systematic investigations into characteristics and attributes of health services. Figure 3 provides a glossary of key terms and concepts as used for this exercise.
In contrast to clinical outcomes research, health services research can encompass a broad array of issues and investigation strategies from vantage points that might include that of patients, providers, a community at large, and health care purchasers among others. Health services research is frequently used by policy makers and regulators to assist in determining community needs, prioritizing the use of resources, and formulating policy. Professions may use health services research to examine status, performance, quality of care, and other related issues.
Chiropractic as a social phenomenon has been studied rather extensively, particularly its often adversarial relationship with conventional medicine. Because medicine and chiropractic have experienced separate evolutions, each having its own training, research, political, social, and cultural experiences, distinct perspectives and institution have evolved. Yet in the delivery of their services, there is constant need for communication, sharing of “customers,” and impacting social institutions such as delivery settings (eg, hospitals) and health care financing bodies (eg, insurance companies and provider networks). Medicine actually played both positive and negative roles in chiropractic's early development and the two profession's social and political efforts have frequently required significant expenditures of each other's resources—legal, political, and academic.
Overview of Health Services Research Literature on Chiropractic Since 1995Conceptualizing chiropractic's role in health care Both internal and external discussion of the role chiropractic does, can, and should play in the health care system appeared in the scientific and policy literature. With more research available documenting effectiveness of interventions such as manipulation, along with information on high use of complementary and alternative health care, even Consumer Reports, traditionally rather negative against chiropractic, published a piece about alternative approaches becoming more mainstream. [6] Another trend noted has been the growth and use of physician extenders and nonphysician clinicians with analyses suggesting they may be cost-effective alternatives and offer access in underserved areas. [7]
Since 1995, chiropractic has been increasingly viewed closer to the mainstream of health care; however, less than 7% of DCs report practicing in multidisciplinary settings. [8] Debate continues over whether chiropractic should see itself as “complementary” or “alternative.” Rupert et al [9] discussed the role of chiropractic as wellness, health promotion, and prevention provider. Although most chiropractors report counseling patients on wellness activities such as physical activity or healthy diet, [8] the extent and frequency of these recommendations may be quite low. [10]
Chiropractic continues to be the most established of the alternative health care disciplines. However, a policy review conducted in 2003 suggests that because of issues surrounding the small magnitude of effects outcomes literature for manipulation, potential erosion of cost advantages over conventional medicine in low back treatment, and continued lack of clarity internally about chiropractic's role in health care, particularly resistance against a role with primary care, the profession is confronted with a number of challenges. [11] Reimbursement is shrinking, the number of DCs is increasing, and mainstream disciplines such as physical therapy, osteopathy, and physical medicine are increasingly competing with chiropractic's conservative, high-satisfaction approaches. [11] Chiropractors on the whole appear to recognize the importance of outcomes and cost-effectiveness research to its future. [12]
Despite clear evidence that the overwhelming majority of chiropractic services provided are for musculoskeletal back and neck pain conditions, [10, 13] internally the profession still grapples with and identifies itself as being strongly connected with primary care and preventative services. [9, 14] Although not at odds with chiropractic training and potential roles in health care, studies investigating delivery of chiropractic services indicate that chiropractors do not routinely provide such services in practice. [10, 13]
Use of chiropractic Consumer use of alternative health care, including chiropractic, continues to be significant and increasing; however, use of chiropractic may be leveling off. [14] More than one third of adults have used a complementary and alternative medicine service within the previous year. [15] Back and neck pain continue to be the leading reasons consumers seek chiropractic care based on chart extractions, patient interviews, and time-of-visit assessments in chiropractic offices. [10, 13, 15, 16]
Dispelling the notion that chiropractic patients' conditions are trivial, one well-done study documented that chiropractic patients are more severe than matched individuals in the general population and of similar functional limitation to medical patients, with chiropractic patients reporting significant worse mental health scores. [16]
Patient satisfaction and preference with chiropractic care continues to be high, and patients with adequate financial means appear to prefer to obtain chiropractic care over medical alternatives. [17] Based on data in the 1994 Robert Wood Johnson Access to Care survey, Paramore [18] estimated that 10% of the US population annually sought chiropractic, massage, or acupuncture care and predicted that with adequate financial coverage, the proportion seems likely to increase. CAM use among patients of rheumatologists was found to be 34%; however, patients who were CAM users reported no differences in outcomes. [19]
In some populations, use of chiropractic may be associated with lower use of other health services and higher measures of health status, although it is not possible to determine causation. A subanalysis of data from a randomized trial on comprehensive geriatric assessment indicated chiropractic users were more likely to report a better health status, exercise vigorously, and be mobile. They were also less likely to have been hospitalized, used a nursing home, and used less prescription drugs. [20]
A British observational cohort study on patients with acute low back pain presenting in general practice were retrospectively compared with similar patients prospectively followed after funding for manipulation service was made available. Use of chiropractic services increased substantially, and patients had shorter waiting times, fewer general practitioner (GP) consultations, less sickness certification, less drug use, and fewer referrals to specialist care. [21] Another British study assessed use of complementary and alternative medicine (CAM) services in 1998 and documented there was substantial use of 6 therapies, including chiropractic. [22] More than 90% of costs for these services were out of pocket.
Differences in patient health status, sociodemographic characteristics, insurance, and attitudes observed between patients who sought medical and chiropractic care were reported in an Oregon study. [23] Disability, insurance, and trust in provider types were particularly important predictors, and the importance of patient attitudes, health status, and insurance in self-referral decisions was emphasized.
Patient knowledge about complementary therapies appears to be low, except for chiropractic care, according to a survey of patients with chronic low back pain under primary care in Seattle and Boston. [24] Chiropractic and massage had been used by the largest fractions of respondents, mostly for back pain. Among prior users of specific CAM therapies for back pain, massage was rated most helpful. Users of chiropractic reported treatment-related “significant discomfort, pain, or harm” more often than users of other therapies. Overall, most patients with chronic back pain were interested in trying therapeutic options beyond conventional medicine, especially chiropractic massage and acupuncture.
A review of data from the Bureau of Health Professions' Area Resource File indicated that chiropractors in rural and high-shortage areas have busier, higher volume practices than do those in other locales and may provide a significant amount of care in underserved areas. [25, 26]
Nature of chiropractic health encounters A substantial number of well-done health service research studies have looked at what services chiropractors are providing in practice. Data on patient demographics, smoking status, referral source, reasons for visit, concurrent medical care, payment source, and visit duration was reported on consecutive visits to randomly sampled licensed CAM providers in 4 states. [27] About 80% CAM visits were by young and middle-aged adults, with two thirds by women. Children comprised 10% of naturopathic visits but only 1% to 4% of all other CAM visits. At least two thirds of visits were self-referrals, with 4% to 12% conventional physician referrals. Chiropractors and massage therapists primarily saw musculoskeletal problems, whereas acupuncturists and naturopathic physicians saw a broader range of conditions. Visits to acupuncturists and massage therapists lasted about 60 minutes compared with 40 minutes for naturopathic physicians and less than 20 minutes for chiropractors. Most visits to chiropractors and naturopathic physicians, but less than one third of visits to acupuncturists and massage therapists, were covered by insurance.
More than two thirds of practitioners of massage therapy and acupuncture were women, with about a quarter for chiropractic and conventional medicine. Only 5% of chiropractors reported being a member of any racial or ethnic group other than Caucasian. CAM providers were more likely than conventional physicians to practice solo (51%-74% vs 26%, respectively), and less than 10% practiced with medical physicians. Massage therapists saw the fewest patients per week (about 14), and chiropractors and conventional physicians the most (about 100). Chiropractors and conventional physicians saw about 3 patients per hour compared with roughly 1 patient per hour for the other CAM professions.
A Canadian focus group study of chiropractors assessed dimensions of return to work in occupational injuries.28 Participants indicated that timely return to work depends on patients' characteristics, severity of injury, clinical progress, the availability of work accommodation, and clinical judgment. The chiropractors commented that their treatment of injured workers rests on their strength in diagnosis and treatment and on providing patient-centered care. Positive human relations within workplaces and the ability to accommodate the work of an injured worker were described as important in return-to-work programs. The participants believed that a bias against chiropractic is present within the medical profession and workers' compensation boards. They viewed this bias as an important barrier when assisting their patients to successfully return to work.
Economics and cost analyses of chiropractic Cost study designs have matured, and research addressing cost components associated with chiropractic generally have become more sophisticated. Cost analyses that address cost elements without clinical outcomes are frequently of interest to purchasers of services (eg, employers, insurers, and individual patients). Cost-effectiveness studies consider the costs associated with achieving a particular outcome and are of particular interest to policy makers. Typical cost-effectiveness approaches report costs related to a specific clinical outcome (eg, cost per point improvement on a disability scale). Cost-utility approaches frame the effectiveness issue in terms of quality-adjusted life years in a population, whereas cost-benefit approaches address money spent to gain a health cost saving (monetary return) elsewhere in the system or over time.
Workers' Compensation Settings A number of cost analyses have been published in the past decade with improved designs and for the most part indicate that chiropractic care is cost-competitive with conventional alternatives. A number of new studies have examined workers' compensation administrative and claims databases. Health care economists have begun to develop more sophisticated models to adjust for the limitations of minimal information available from claims data. Johnson et al [29] developed a model to adjust for case complexity and offered a comparison of medical and disability costs in one California work compensation carrier's data set. The results suggested that chiropractors and physicians were equally effective in terms of claim duration and had similar total claims costs and concluded that medical and chiropractic care can substitute for each other in nonsurgical low back claims.
A retrospective review of 2000 nonsurgical back injury claims from 1986 and 1989 in the Utah Worker Compensation Fund compared medical and chiropractic costs.30 Treatment costs in cases managed by chiropractic physicians increased 12% between 1986 and 1989. Treatment cost in cases managed by medical physicians increased 71% in the same period. Compensation (wage replacement) costs increased 21% for the chiropractic group and 114% for the medical group. The authors attributed the reduced chiropractic costs to a preapproval program required of the chiropractic physician, whereas medical costs escalated in the absence of price controls.
A retrospective, actuarial review of Florida workers' compensation claims data commissioned by the Florida Chiropractic Association reported that claimants with musculoskeletal diagnoses who sought chiropractic services trended toward lower medical and claim costs had shorter durations of time loss and reached maximal medical improvement faster than those who did not. [31] It should be pointed out that Florida had a capped chiropractic benefit during the study period.
A comprehensive review of workers' compensation claim costs was undertaken in Texas because of significant economic pressures leading to a revamping of their workers' compensation system. [32] The study reported that the state had the highest medical costs of states in the region. Physical medicine (including chiropractic) and surgery accounted for the majority of costs, and it was noted that a small but substantial number of providers drove system costs. Because of the significant policy implications for many stakeholder including insurers and providers, reanalyses of the data set were subsequently undertaken by an industry-sponsored trade group and the Texas Chiropractic Association [33, 34] The industry report emphasized that a substantial proportion of physical medicine and chiropractic providers had extremely high costs, whereas the study funded by the chiropractic association emphasized that even with such claims, overall chiropractors treated nearly one third of all low back claims yet used 9% of overall costs (17% of direct medical costs).
A small UK case series study prospectively followed 32 workers with occupational back and neck complaints seeking chiropractic services in the UK. [35] Outcomes measured pain, disability, quality of life, perceived benefit, and satisfaction with care. Sickness costs to the companies and treatment use were also recorded over 2 years. Effect sizes were large for pain and for 7 out of 8 dimensions of the SF-36 health status questionnaire at 6-month follow-up, although not for disability. High levels of satisfaction and perceived improvement were reported, and sickness costs to the companies fell. However, the sample size in this pilot study was small and did not include controls.
Although several cost analyses have been done, the methodologies and perspectives vary, and as the Texas data with 3 different published analyses with different conclusions illustrate, there is need to build better cost analyses designs into prospective studies. As Baldwin et al36 point out, the literature suggests that DCs and MDs provide equally effective care for low back pain and that chiropractic patients are more satisfied with their care. However, the evidence on the relative costs of medical and chiropractic care is conflicting in existing studies. However, studies do trend toward lower or equal direct medical and disability costs and do not justify exclusion of a chiropractic option in workers' compensation benefits.
General Health Settings Several recent studies have also examined general health insurance coverage offers insight into health care expenditures. Conventional wisdom usually argues that allowing additional provider types results in increased expenditures by default. A 4-year retrospective claims data study compared 700,000 health plan members with an additional chiropractic coverage benefit and 1 million members of the same health plan without the chiropractic benefit. [37] Members with chiropractic insurance coverage, compared with those without coverage, had lower annual total health care expenditures. Having chiropractic coverage was associated with a 1.6% decrease in total annual health care costs at the health plan level. Back pain patients with chiropractic coverage, compared with those without coverage, had lower use (per 1000 episodes) of plain radiographs, low back surgery, hospitalizations, and magnetic resonance imaging. Patients with chiropractic coverage, compared with those without coverage, also had lower average back pain episode–related costs. The authors attributed the findings to several possible effects such as positive risk selection, substitution of chiropractic for medical care, less invasive treatment profiles of chiropractors, and lower health service costs associated with managed chiropractic care.
Another review of large claims databases from managed care health plans compared between groups with and without chiropractic coverage assessed the rates of plan use for patients seeking care for neuromusculoskeletal complaints. [38] The study concluded that patients with chiropractic coverage use it as a substitution for medical services. This is consistent with an earlier retrospective, actuarial review of total health care costs for comparable cases of neck and back pain for members in a health maintenance organization who sought chiropractic care and other treatment methods over a 1-year period. [39] Care, prescription, and imaging costs were lower in the group managed by chiropractors, with nearly identical patient satisfaction and surgical rates.
Sarnat and Winterstein [40] reported on a nonrandomized review of claims costs and outcomes (including patient survey) over a 4-year period in an integrative medicine Independent Practice Association using primary care physicians who specialized in nondrug, nonsurgical interventions compared to two health maintenance organization groups' experience in the same geographic area. Stratification and sample matching were used. Forty-three percent lower hospitalization and surgery costs were reported along with 58% fewer hospital days and 51% lower pharmaceutical costs.
A pilot study in the United Kingdom tested recommendations of the Clinical Standards Advisory Group (CSAG) in 1994 for a cost-neutral way to reduce back pain disability by incorporation referral to manipulation practitioners in primary care. [21] The design involved 194 patients with acute low back pain retrospectively presenting to 11 GP practices during a 6-month period and 344 prospectively to the same practices in a subsequent 6-month period. Increased referrals to manipulation practitioners occurred with the prospective patients. The study documented fewer referrals to secondary care than retrospective patients, fewer GP consultations, less drug use, and fewer certified sickness days in the prospective period where referrals were made. In addition, patients who were referred reported shorter waiting times and the authors reported that savings in sickness incapacity benefits were evident by following CSAG recommendations.
A larger, well-designed, prospective 4-arm trial randomizing 1,334 patients to 12 weeks of either medical care, manipulation, exercise, or exercise/manipulation combination was later conducted in the UK, which documented better function improvement in all physical medicine interventions. [41] A cost analysis was conducted as part of the trial to evaluate if inclusion of manipulation and exercise benefits within the British National Health Service could save health care costs while maintaining or improving outcomes of back pain treatment. [42] The study concluded that manipulation alone offered the best cost per quality-adjusted life year over a 1-year period.
In a randomized Swedish comparison of 332 patients into chiropractic and physical therapy treatment for back and neck pain, no differences in outcomes or costs were reported.43 However, subgroup analyses favored chiropractic treatment with pain of less than 1-week duration and physical therapy with pain of more than a month duration. In addition, a larger proportion of patients in the chiropractic group sought additional medical care.
General health care setting data offer more prospective designs and concur with the trend reported in workers' compensation settings that chiropractic obtains at least comparable outcomes to alternatives with potential cost savings and higher patient satisfaction. Most of the general health setting studies correlate with a decreased use of other system resources but appear to be most likely when offered in a managed care environment. None of the studies have attempted to assess relationships of managed cost containment strategies on practice overhead issues such as cost shifting to better insured populations such as injury care. Another concern may be that reduced reimbursement (such as is typical of Medicaid coverage) over time can contribute to access issues as providers willing to participate in reduce reimbursement plans decrease. [44, 45]
Chiropractic Practice Environments Delivery of services Since 1995, the National Board of Chiropractic Examiners has produced two job analysis monographs reporting results of two geographically stratified random national surveys of chiropractors in the United States regarding their perceptions of practice. [8, 46] The sample size represented nearly 10% of the profession in the US in the 2000 report and less than 5% in 2005. These studies updated a similar 1993 effort. An inventory on practice demographics is offered along with provider recall reports of patient characteristics, conditions evaluated and managed, and practice procedure preferences.
A UK survey of all chiropractors, osteopaths, and physical therapists belonging to a manipulation association achieved a 62% response rate and provided a description of the practice of chiropractic, osteopathy, and physiotherapy, and examined past and current levels of provision of musculoskeletal services by practitioners qualified in manipulation for British National Health Service patients. [47] Provider's delivery preferences and views on optimal models for future arrangements were recorded as well.
Cherkin et al [10, 27] conducted a prospective study at the time of the patient visit on what occurred with chiropractors, naturopaths, acupuncturists, and massage therapists. The study described the characteristics of the 4 largest licensed CAM providers and compared them to conventional physicians. Some 25% of chiropractors and medical physicians are women, compared with higher percentages of women in acupuncture, massage therapy, and naturopathy. Less than 5% of CAM providers report being a member of any racial or ethnic group other than Caucasian, most CAM providers are in solo practices, and less than 10% of CAM providers practice with a medical physician. Chiropractors and medical physicians both saw about 100 patients per week, averaging about 3 patients per hour. About 80% of visits were with young or middle-aged patients, two thirds of whom were women. Two thirds of CAM visits were self-referred. Chiropractors saw primarily patients with musculoskeletal complaints, spending on the average 20 minutes per visit with the patient, and most visits were covered by insurance.
Chiropractic care provided to geriatric populations was the focus of a few publications, including descriptions of techniques and recommendations made for geriatric populations, and the degree of training chiropractors receive on the subject. [48, 49] Despite extensive practice-based data that indicate chiropractors overwhelmingly provide care for musculoskeletal conditions, most chiropractors self-report that they are making evidence-based reco0mmendations such as increasing physical activity, dietary recommendations, or general healthy lifestyle recommendations such as smoking cessation and weight loss. [9] Using data from the Bureau of Health Professions Area Resource File, Smith and Carber26 reported that chiropractors in rural and high-shortage areas were found to have busier, higher volume practices than in other locales. Chiropractors were reported to be rendering a substantial amount of care to underserved and rural areas, potentially filling some of the need for providers in those areas.
Reimbursement of chiropractic services Sources of reimbursement for chiropractic patients were reported in a chart extraction study conducted by RAND (Santa Monica, Calif). [16] Visits per episode varied considerably by site (2-fold for medium low back pain–related visits, and 4-fold for non–low back pain). Patients tended to be between 35 and 50 years old, slightly more women, and married. Overall, approximately 40% were private fee for service, 20% self-pay, 20% worker's compensation or personal injury, and 20% other.
Trends in coverage and reimbursement for CAM care overall have been reported by Pelletier et al. [50, 51] A literature review was conducted to determine which new insurers had special policies for CAM from 1997 to 1998 and was updated in 2000 along telephone surveys of representative cohorts of managed care organizations and insurers. Overall, consumer demand for CAM is motivating more insurers and plans to assess the clinical and cost benefits of incorporating CAM services. Payers also want more outcomes studies on conventional, complementary, alternative, or integrative medicine interventions to inform coverage policy.
Traditionally, time spent with patients has served as a face-value means of determining how much to charge office visits with patients. Beginning in the late 1980s, however, Medicare moved away from prevailing and time-based methods for provider reimbursement to a resource-based model that considers physician work, practice overhead, and malpractice risk for individual interventions. [52]
One recent study examined time spent in acupuncture and chiropractic visits based on a random sample of 130 licensed chiropractors and 133 licensed acupuncturists surveyed in 1998-1999. [53] Data from 2,550 chiropractic and 2,561 acupuncture visits were reviewed: mean chiropractic visit length was 21.5 minutes and mean acupuncture visit length was 56.6 minutes. New patient visits took longer, whereas visits for wellness or chronic problems were shorter. Preventive counseling by the chiropractor increased visit time, as did use of manual (vs instrument) spinal manipulation, soft tissue techniques, and physiotherapeutics. Based on this, the authors concluded that a time-based model could be used for determining reimbursement.
The physician work component of chiropractic services has been studied and reported by using the methodology developed for Medicare's Resource-Based Relative Value Scales. [54, 55] The reliability and validity of the methodology was demonstrated on a national sample of chiropractors. A comparison of physician work estimates for evaluation and management, manipulation, and radiology services from chiropractors against resource costs previously reported for various medical specialties and osteopaths found that the magnitude of work performed by chiropractic physicians in clinical services is within ranges reported for medical and osteopathic physicians for all types of services.
Patient satisfaction with chiropractic care Reports of high chiropractic patient satisfaction continue to appear in the literature, but getting explanations for it are beginning to appear. Satisfaction between medical and chiropractic care was compared in a clinical trial at the University of California, Los Angeles. [56] Mean satisfaction score for chiropractic patients was greater than for medical patients. Self-care advice and explanation of treatment predicted satisfaction and reduced differences between satisfaction with chiropractic and medical care, leading authors to conclude that communication of advice and information to patients with low back pain increases satisfaction.
A British study attempted to determine which functional and affective outcomes may predict satisfaction and improvement. [57] Significant relationships between change scores and both improvement and satisfaction were reported, with most of the variance in satisfaction related to overall improvement and very little associated with improvements in activity. Pain, work, and ability to control pain together predicted less than a third of the variance in overall improvement, and no other variables predicted outcome (thus leaving 73% of the variance unexplained).
Chiropractors were among providers studied in a work compensation setting in Washington State that identified a correlation with patients' perceptions of their physicians technical competence at 3 to 5 months after injury and reduced disability status 12 to 18 month after injury. [58]
Interprofessional interactions and integration A substantial amount of literature has appeared examining interprofessional interactions between chiropractors and CAM providers and conventional health care delivery.
Communication Breen et al [59] surveyed GPs in the South of England to assess communication needs when making a referral to manipulation providers. A low response rate was obtained, but results suggested that GPs appear to prefer referring to disciplines with which they have personal experience. Reporting preferences were for a brief letter format upon treatment completion with the nature of treatment and advice given. Not surprisingly, for an initial report, a summary of the nature of the problem, a brief history, a summary of relevant findings from the examination, any investigations, and a prognosis were preferred. Many GPs commented that they were more comfortable in referring to physiotherapists because they felt they had a better understanding of the treatment involved. Furthermore, chiropractic and osteopathic terminologies were reported to be more confusing than physiotherapy terminology.
A Dutch survey assessed the nature and quality of communication between GPs and chiropractors by mailing questionnaires to GPs requesting personal and practice details and asking about their knowledge of chiropractic, present communications, opinions on chiropractic terminology, and preferences with regard to communications with patients. [60] Almost half (115 out of 252) responded. Although almost all respondents had heard of chiropractic, nearly 80% indicated that the information they obtained came from patients. Only 10% of the GPs refer their patients to a chiropractor on a regular basis. Referral of patients was found to be significantly related to the GPs' perceived knowledge of chiropractic and positive opinions regarding their past communications with chiropractors. More than 80% of the GPs said that they were interested in receiving (or continuing to receive) feedback reports, even if they did not personally refer the patient to the chiropractor. More than a third of respondents indicated that chiropractic reports contain confusing terminology that might negatively influence communication. General practitioners preferred typed, short reports, preferably sent after the last treatment.
The chiropractic perspective has also been reported. The type and extent of interprofessional contacts between chiropractors and conventional practitioners in Sweden was assessed from self-administered questionnaires and a structured telephone interview. [61] Twenty consecutive patients of 31 chiropractors (n = 616) participated in the questionnaire survey, and 15 randomly selected chiropractors participated in the telephone interview. Eighteen percent of patients were recommended to chiropractic care by some other health care practitioner. Only 1% of the participating patients were referred for chiropractic care with a written request. Almost all chiropractors (87%) could provide a list of the last 3 health care professionals with whom they had contact. The median number of interprofessional contacts per month was estimated by the chiropractors to be 10.
The nature and relevance of integration of chiropractic into the conventional delivery system has also been the subject of recent studies. A cross-sectional survey of 311 DCs in North Carolina evaluated DC reports of multiple facets of satisfaction with their work including compensation, intrinsic motivation of patient care, positive relations with DC colleagues, and dimensions interactions with MDs. [62] Overall satisfaction was relatively high and was unrelated to satisfaction with MD interactions. DCs who received more referrals from MDs correlated with a higher satisfaction in MD/DC interactions.
Barriers to integration of CAM into conventional reimbursement and coverage systems were explored in a multiyear work group in Washington State. [63, 64] Payers and representatives of CAM trade associations met regularly over a 2-year period with facilitators to systematically identify issues and potential solutions as seen from both sides' perspectives. Among key issues identified were that payers could not understand CAM syntax, they had no means to manage claims by predicting use due to high practice variation, the overall lack of standardized care pathways and clinical progress thresholds for CAM care, and the failure of CAM practitioners to distinguish noncovered elective, prevention, wellness, and maintenance care from covered condition care. CAM representatives issues included lack of willingness by payers to obtain internal CAM expertise to assist in adjudication.
Integration of chiropractic into other CAM settings has also been examined. [65] A survey of 25 nationally benchmarked alternative medicine clinics during 2000 found that less than half of the clinics (n = 12) included DCs, and 5 of the remaining clinics offered manipulation service by doctors of osteopathy, doctors of naturopathy, or physical therapists. The clinics with barriers to working with DCs appeared to be related to preferences of affiliations with conventional medicine settings (eg, hospitals) to not work with chiropractors.
Technology assessments related to chiropractic A panel of chiropractic scholars reported on the state of technique-oriented research relative to low back conditions. [66, 67] Various specific chiropractic adjustive procedures for the treatment of common types of low back pain were “rated” drawing on the clinical expertise of the panel members and the relevant literature. The 3 most studied adjustive procedures are side posture (high-velocity, low-amplitude), distraction (mostly flexion distraction), and mobilization, respectively. The clinical condition most commonly addressed by the included studies is low back pain and the specific procedure with the widest base of evidence support is high-velocity, low-amplitude side posture manipulation for low back pain. Other procedures with evidence of effectiveness were distraction technique and high-velocity, low-amplitude prone with drop table assist. The 3 procedures rated least effective based on the evidence were upper cervical technique, non–thrust reflex/low force, and lower extremity adjusting. The 4 conditions rated most amenable to chiropractic treatment were noncomplicated low back pain, sacroiliac joint dysfunction, posterior joint/subluxation, and low back pain with buttock or leg pain. Procedures rated highest were supported by the highest quality of literature. The authors caution that much more research is needed to understand which procedures maximally benefit patients for which conditions. Appropriateness methodology developed by RAND was used to assess manipulation and mobilization for cervical spine conditions.68 Along with a qualitative literature review that encompassed more than 500 articles, some 1,200 clinical indications were rated for appropriateness by a 9-member multidisciplinary expert panel. Of key interest is the nature of agreement on the appropriateness or inappropriateness of manipulation for various conditions. Panelists demonstrated agreement on nearly 40% of recommendations, with just 2% of the indications eliciting disagreement.
A prospective clinical trial that warrants mention in discussions of technology assessment is the clinical United Kingdom Back Pain Exercise and Manipulation trial as it was undertaken with the specific intent to assess benefit related to formulating policy decisions relative to coverage of manipulation in the British National Health Service. [42] The study concluded that manipulation followed by exercise and manipulation alone both provided a moderate benefit at 3 months and small benefit at 12 months, but exercise alone provided only a small benefit at 3 months and no benefit at 12 months. The companion cost analyses mentioned previously reported high value for manipulation. [42]
Chiropractic practice parameters and guidelines Very little work has occurred in the area of chiropractic guidelines. RAND conducted one study examining how congruent chiropractic practice patterns were with appropriateness recommendations for manipulation from their expert panels. [69] A chart extraction done on 1,310 patient records from 131 chiropractic offices in 6 North American metropolitan areas documented that 1,088 had spinal manipulation with 79% of those records adequate for determining if care decisions were congruent with an expert panels' appropriateness criteria. Overall 46% of records were congruent with appropriateness criteria, 25% were uncertain, and 29% were not congruent. Patients who did not undergo manipulation were more likely to have a presentation judged inappropriate than were patients who did undergo spinal manipulation. The proportions judged congruent with appropriateness criteria are similar to those described for medical procedures.
Two new chiropractic guideline documents appeared, both from narrow-scope chiropractic organizations. [70, 71] The Clinical Practice Guideline Number 1, Vertebral Subluxation in Chiropractic Practice from an organization calling itself the Council on Chiropractic Practice (CCP) is an update of a previous guideline from the World Chiropractic Alliance. The CCP document focused on various clinical assessment and intervention strategies for “subluxation-based” care (as distinguished from care that incorporates patient condition and diagnosis into management decisions). Literature review is more comprehensive than the first effort, but the quality of studies and literature unfavorable to recommendations is not appraised. The International Chiropractors Association also published its Recommended Clinical Protocols and Guidelines for the Practice of Chiropractic. [71] To their credit, the International Chiropractors Association guidelines acknowledge in their forward that they “intended to reflect the core values and policies of the International Chiropractors' Association” in the context of its views and policies on chiropractic. Overall the clarity of how evidence was assessed and related to recommendations was inadequate.
In an effort to appraise guideline quality, Cates et al [72, 73] used the standard Appraisal Instrument for Clinical Guidelines (Cluzeau instrument) to assess the attributes of each of the chiropractic guidelines. Ten independent experienced evaluators completed the instrument and made an independent, global assessment of two studies, the first evaluating the CCP's Clinical Practice Guideline Number 1, Vertebral Subluxation in Chiropractic Practice, [71, 72] and the Haldeman et al74 Guidelines for Chiropractic Quality Assurance and Practice Parameters. Mean scores for each of the instrument's 3 dimensions for the Haldeman Guideline were as follows: rigor of development, 77% (4.89); context and content, 69.17% (9.13); and application, 52% (13.32). The CCP scores were as follows: rigor of development, 20% (4.13); context and content, 10.83% (6.46); and application, 0% (not applicable). Mean scores for the International Chiropractors Association guideline were as follows: rigor of development, 27% (5.1); context and content, 18.3% (9.4); and application, 2% (3.9). The authors concluded that the CCP guidelines might be flawed as a result of biases and that they failed to document fundamental steps of quality guideline development and as a result were not recommended. The Haldeman et al [74] guidelines were considered “valid and useable”; however, their publication date of 1993 has made them outdated and their recommendation was provisional as a result. The unanimous global assessment for the International Chiropractors Association guidelines was “not recommended as suitable for utilization in practice.”
A guideline not geared at all toward chiropractic practice unexpectedly impacted chiropractic practice in California when it was adopted into law and then used as a justification to limit chiropractic coverage in their workers' compensation system. [75] The American College of Occupational and Environmental Medicine, a trade association of occupational health specialists, updated their 1997 guidelines in 2004 to assist occupational health specialists in considering care options. Although the new edition was much more favorably disposed to manipulation than the earlier edition, the recommendations were minimalist summaries for occupational health specialists considering referral for manipulation with general recommended thresholds at which clinical progress should be expected.
Overall, there appear to currently be no adequate evidence-based chiropractic practice guidelines or parameters available, and the case of regulators turning to nonchiropractic guidelines underscores the need to address this deficiency.
Quality management A small amount of literature has come out on quality management and improvement related to chiropractic. The Institute for Healthcare Improvement ran collaborative training effort to merge scientific evidence about back pain and knowledge about behavior change to help organizations improve care for back pain. [76, 77] Participating insurance plans, health maintenance organizations, and group practices focused on self-identified problems. Two chiropractic teaching clinics and one multidisciplinary tertiary spine center that employed chiropractors were among the participants. The yearlong program included quarterly meetings, coaching for rapid cycles of change, a menu of potential interventions, and recommendations for monitoring outcomes. Participants interacted through meetings, e-mail, and conference calls. Of the 22 participating organizations, 6 (27%) made major progress. Typical changes were reduced imaging, bed rest, and work loss, and increased patient education and satisfaction. Specific examples were a 30% decrease in plain radiographs, a 100% increase in use of patient education materials, and an 81% drop in prescribed bed rest. Chiropractic facilities reduce duration of examination times, unnecessary radiograph use and improved systematic incorporation of customer needs into clinical processes.
In Britain, a primary care audit tool was developed based on criteria derived from an evidence-based best practices low back pain guideline addressing diagnostic triage, psychosocial assessment, treatment in primary care, avoidance of bed rest, advice on staying active, and patient referral. [78] The tool was tested on more than 1000 primary care practitioners during a 2-year development period and included a 6-month audit cycle and was refined based on input from practitioners and audit administrators. Separate toolkits for GPs and manipulation therapists are included with instructions for conducting and analyzing the audit data.
In Australia, a formal regulatory mandated compliance testing program 3 years after implementation was evaluated. [79] The mandatory program called for all medical (including chiropractic and dental) equipment used in human diagnosis to be tested at prescribed frequencies using established protocols. The application of the required test methods demonstrated various noncompliance issues. Notices of noncompliance were received for approximately 60% of the equipment in the hospital following the equipment's first annual test. The reasons for, and the significance of, failure varied according to equipment category, test category, equipment use, and equipment age. However, at the end of the third year of testing, approximately 75% of the tested radiograph units satisfied the compliance criteria. The main reasons for noncompliance were found to be design limitations of old technology and the current radiation legislation that makes it difficult for some older equipment to meet the relatively stringent criteria.
Physician Behavior One study aimed at implementing guidelines was reported that had impact on the use of chiropractic services. [80] RAND and the Army Medical Department collaborated to develop a guideline implementation system and assess effects on patient care. Guidelines were implemented in 3 successive demonstrations targeting low back pain, asthma, and diabetes. Outcome evaluation revealed a significant downward trend in the percentage of patients with acute low back pain referred to physical therapy or chiropractic care (10.7%-7.2%) at demonstration sites and no such trend at control sites.
Pending Health Services Research Questions Health services research typically has substantial health policy implications that can impact policy and regulation related to chiropractic, insurance coverage, and the ability to make improvements in patient care that not only benefit patients but also enhance the profession's ability to remain competitive with other providers. Better descriptions of what chiropractors do have appeared; more sophisticated approaches to assess cost outcomes associated with care have been done. Recommendations for policy and coverage improvements relative to provision of manipulation services have arisen.
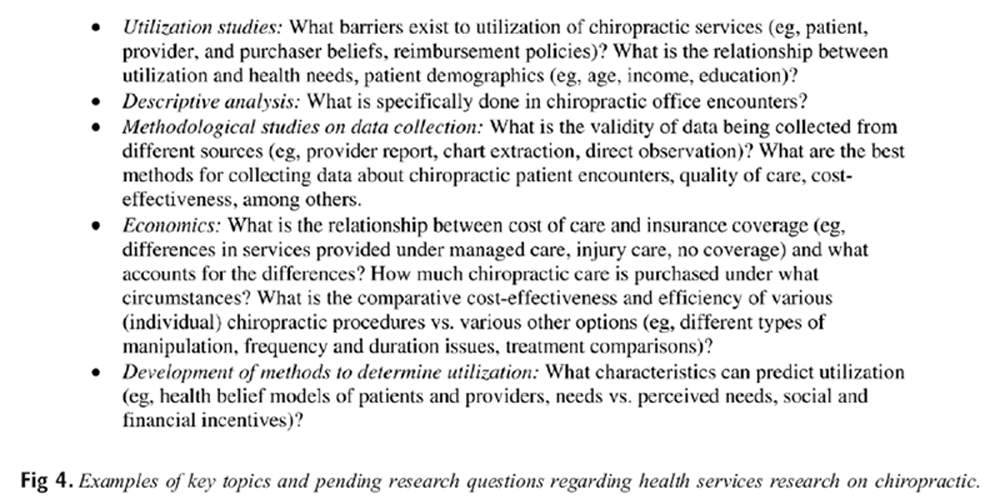
Figure 4
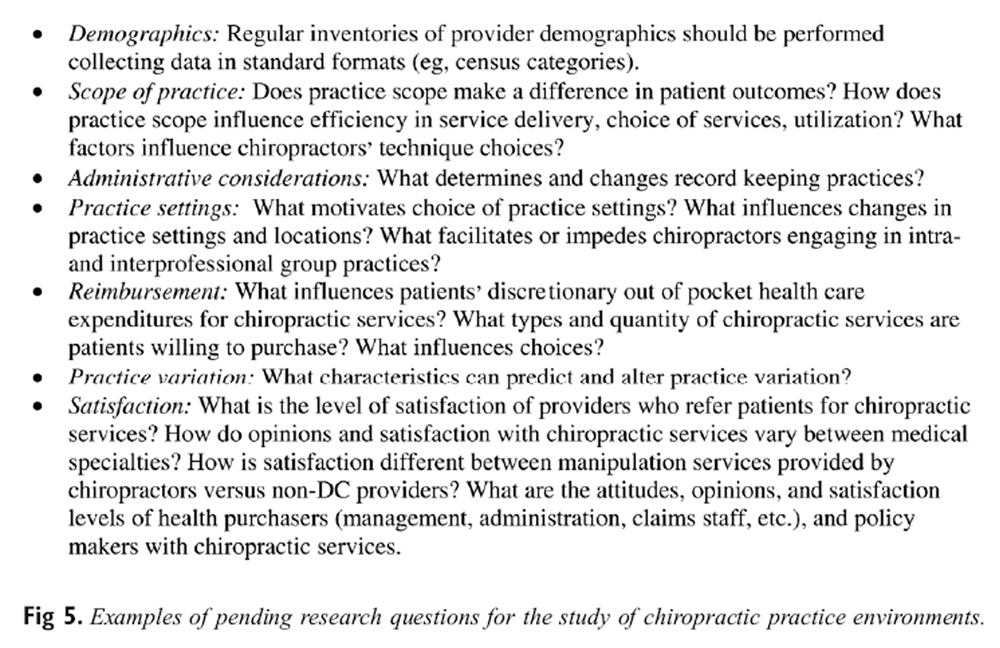
Figure 5
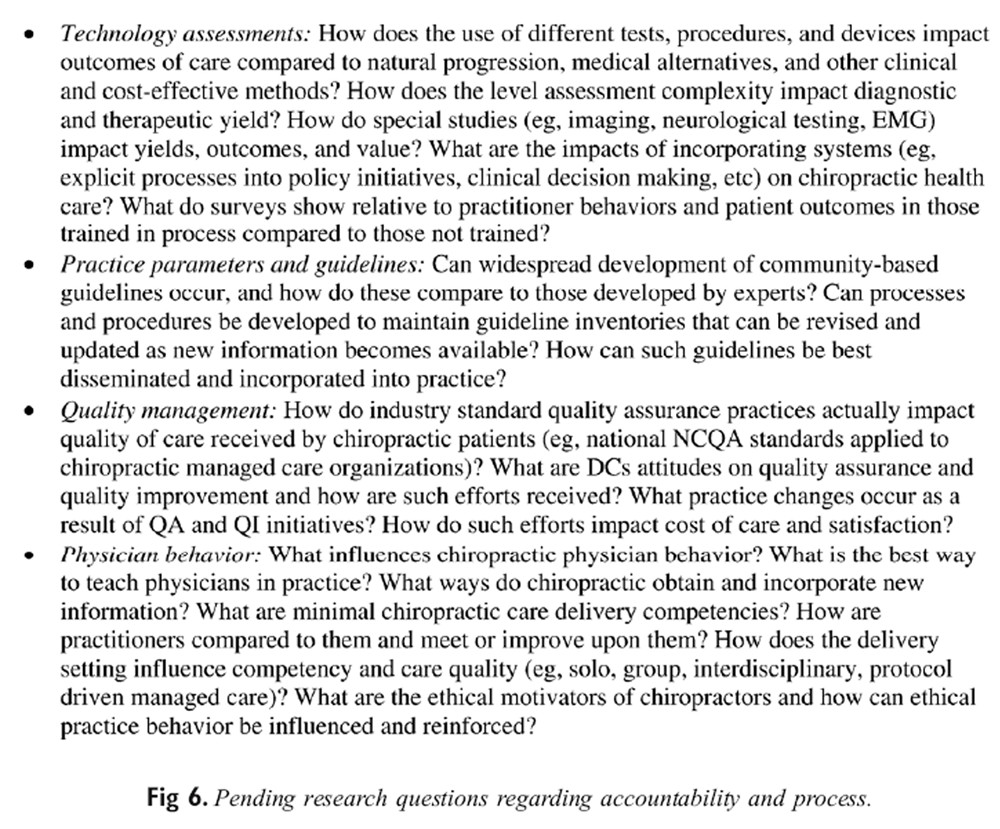
Figure 6 However, many health services research questions remain to be answered. Figures 4-6 summarize the domains and example of health services that were first presented 10 years ago1 but remain relevant nonetheless. The magnitude of research required to provide definitive answers is overwhelming and unlikely to be influenced significantly without dedicated effort to seek and obtain funding. A resource infrastructure issue is also at issue in that very few health services researchers exist within chiropractic, no specific career tracks exist, and interest in critical areas such as quality improvement and improving patient outcomes is lacking in any meaningful, sustainable form within organized chiropractic or the teaching institutions. It seems reasonable then that prioritization of research issues for health service research will be driven primarily by specific end users with business needs to have answers.
2005 Health Services Research Recommendations for Chiropractic The 2005 Health Services Research review team evaluated the progress of the chiropractic profession to address the recommendations from the 1997 prioritization exercise. The team found very little evidence of significant progress in any of the 9 original recommendations. The 2005 health services research review team strongly suggests that the same set of recommendations remain useful; however, because progress was minimal, the decision was made to reduce the number of recommendations to 3 that reflect areas with significant urgency to the profession over the next several years.
Accountability and Quality Research Prioritization The recent inventory of chiropractic-based health services research related to accountability and process development is compared to the ongoing advancement of health care accountability and related formal process issues resulting from the global movement of the health care industry over the past 10 years. As a result, other specific recommendations were presented to the 2005 Association of Chiropractic Colleges—Research Agenda Conference inviting discourse and testimony, and are summarized here.
Accountability infrastructure The health care industry is in the midst of significant and certain movement toward evidence-based medicine processes. Evidence-based practice has its own place in academic, clinical, and research applications with more formal critical appraisal and implementation tools used in clinical practice. Chiropractic health services research efforts and implementation/education strategies should:
Foster evidence-based practice—with “best current evidence.”
Keep up with changes in “hierarchy of evidence.”
Develop “push” and “pull” strategies for access to best current evidence.
Provide access to discipline-based preappraised databases (eg, Cochrane, PEDro, Hooked on Evidence).
Integrate information technology–based job aids and learning tools.
Provide education and training opportunities for “new blood” in health services research and EBP mechanisms.
Improvement processes consistent with Institutes of Medicine recommendations The Committee on Quality Health Care in America has been tasked by the Institutes of Medicine (National Institutes of Health) to investigate quality of care issues for the past several years. Their efforts have resulted in reports on medical errors [81] and, most recently, a set of comprehensive recommendations toward assuring quality improvement processes in health care delivery—Crossing the Quality Chasm: A New Health Care System for the 21st Century. The most prominent of those recommendations have a place in health services research planning and study, academic and continuing education curricula, and “best practice” implementation initiatives:
Quality improvement taught as an essential element of education and training
Matching best practice descriptions to meaningful outcomes
Integration of information technology, eg, electronic medical record
Benchmarking and quality measures
Identification of evidence-based, socially relevant quality indicators
Use of meaningful outcomes and/or practice indexes as scorecards for improvement purposes
Patient safety systems/IT-based computerized order entry
Efficient health care data exchange
Regain cultural authority The chiropractic profession, like most of the medical profession, has lost its cultural authority to health care economists, actuaries, and highly structured health delivery systems. Reimbursement and coverage decisions have been steered away from epidemiologic and clinically based guidelines and protocols to experience-rated systems—with very limited physician input. Short-term strategies for the chiropractic profession should include:
Skill and expertise to guideline/best practice development
Professional culture for implementation of best practice descriptions into communities of health care
Engage in ongoing improvement processes
Cost Analysis Research Prioritization There are two general kinds of cost studies. Those that consider only the cost element without any clinical outcomes are the most common in the chiropractic literature and simply ask: “How much did it cost?” Most of the insurance and workers' compensation cost studies in chiropractic have been of this type. In general, this type of study is of interest to employers, insurers, and to individual patients. Cost-effectiveness studies consider the clinical outcomes achieved along with the costs. Three approaches to cost-effectiveness research include standard cost-effectiveness analysis, which looks at the money paid to return a specific clinical benefit (such as a 1-point improvement in an Oswestry score). This approach is increasingly included in clinical trial designs. A cost-utility approach considers the money paid to obtain an improvement in “quality-adjusted life years,” which allows policy makers to “normalize” economic outcomes across different conditions and populations. Cost-benefit approaches attempt to translate a health benefit achieved from an intervention into a dollar amount.
Because the inclusion of any health care service in public or private plans is increasingly dependent on accurate and meaningful cost analyses, increasing sophistication is needed for how cost is considered in chiropractic research. Technical skill, access to administrative data, and expertise in policy implications of cost studies needs increased prioritization in the chiropractic research agenda.
Utilization Research Prioritization After a decade of apparent growth in the use of chiropractic, the most recent assessment indicates that American's use of chiropractic services has actually dropped from a 1990s high of 9.9% to 7.5%.14 In the 1997 recommendations, a key area of research proposed related to determination of barriers to use of chiropractic services. Although opinions on the matter are many (eg, high practice variation, poor understanding of professional role, continuing medical ostracism, fear of side effects, poor professional image), very little new research specifically designed to assess beliefs and opinions of policy makers and health purchasers has occurred. No systematic attempt has occurred to identify relevant constituencies, organizations, and decision makers who address chiropractic coverage issues.
Use and coverage for chiropractic services remains a high priority for the profession at large, and one might expect that chiropractic trade groups would devote resources to this area. However, the perspective from 1997 that an organized effort on the part of chiropractic organizations and institutions should occur does not appear to be likely; rather, only those with an economic interest in chiropractic coverage have engaged in such research to date. Thus, in the market place, various health plans and perhaps certain clinical organizations appear more likely to fund and conduct such work than chiropractic academic centers or trade associations.
In general, it was the consensus of the authors that although a significant amount of health services research related to chiropractic has been conducted since 1995, it has occurred without any organized effort, prioritization for funding, or input based on areas identified in the original Research Agenda for Chiropractic recommendations. It is suspected that the previous recommendations had virtually no impact on setting health services research priorities, and the extent to which topics for research conducted in the past 10 years was stimulated by them is negligible.
Although the organization of the recommendations was reasonable, it was decided that a smaller number of simplified recommendations would be offered, and a refinement of those who might fund or conduct such research be attenuated by considering what existing groups have done so in recent years and what organizations actually have a tangible business need for conducting it.
Although most of the recommendations from 1995 could still apply in 2005, a smaller number of more focused recommendations were deemed preferable.
Develop Valid Measures and Predictors of Quality Chiropractic Care
Recommendation 1:
Identify attributes of quality chiropractic care.
Identify instruments and processes to measure quality and changes in quality of care in delivery settings.
Develop quality improvement implementation strategies and verify effectiveness in improving identified indicators of quality.
Rationale
Improving the quality of patient care has become a national priority for health policy. Problems in care quality have been documented for decades and specific attention has been given to making improvements. Identified deficiencies include failure to provide needed care, provision of unnecessary or inappropriate care, commission of medical errors, the need for better organization of care support processes, evidence-based best practices, and better use of technology, and improved health work force training. Chiropractic research has not specifically assessed quality and appropriateness of care issues, comparative effectiveness and cost-effectiveness of chiropractic procedures, implantation of practice improvements, or change in physician behavior.
Because existing chiropractic institutions have limited resources and interest in health services research, and because social pressure to improve quality is likely to be seen at the delivery side, it seems likely that advances in this area will only arise through collaboration with private sector intuitions (eg, health purchasers) and interested external institutions (eg, health policy centers and think tanks).
Actions RequiredTechnical
Identify attributes of quality chiropractic care.
Develop instruments and processes to measure and audit attributes of quality in actual practice settings.
Identify strategies for developing capacities for improvement in quality in practice.
Logistical
Identify private sector and external institutions for potential interests in research collaborations.
Identify potential government and philanthropic funding support sources, including potential interest generation within existing academic centers that currently help set funding priorities.
Internal agents (within the chiropractic profession,
its institutions and organizations)
Funding organizations and foundations (eg, Foundation for Chiropractic Education and Research [FCER], CCCR)
Chiropractic purchasers, plans, networks
Independent chiropractic scientists and/or research centers
External Agents
Health purchasers
Public sector (federal and/or state) funding agencies (eg, Health Resources and Services Administration [HRSA], National Institutes of Health [NIH], Agency for Healthcare Research and Quality [AHRQ])
Academic health policy institutions
Recommendation 2: Develop and Refine Strategies to Perform Meaningful Cost Analyses Relative to Delivery of Chiropractic Services
Perform comparative cost analyses of different chiropractic procedures.
Specify different points of view regarding utility of chiropractic services (value priorities of patient, society, purchaser, profession).
Evaluate direct and indirect cost factors.
Include use at system-wide level in cost analysis designs (eg, net effect of cost of chiropractic benefits on member populations).
Focus on tools to facilitate efficiencies in the delivery of chiropractic services.
Rationale
Cost analysis methodologies have become more complex and sophisticated since early cost comparisons were performed on chiropractic services. [36] In addition, medical care for conditions commonly seen by chiropractors has improved dramatically. In the past, typical chiropractic care has compared favorably with now discredited “usual” medical interventions such as high complication medications, bed rest, and poor patient selection for surgery; more recent comparisons suggest outcomes and costs for best usual chiropractic care and best practices medicine may have similar outcomes. Some studies have suggested that chiropractic serves as a substitute for some medical services. [37, 40] Cost analyses methods will need to be more routinely included in clinical trial design and more sophisticated retrospective and use study designs will be needed, particularly in relation to making evaluating changes in cost outcomes relative to implementation of practice improvements.
Actions RequiredTechnical
Define specific methodological issues from existing cost-effectiveness studies.
Establish investigative teams with expertise in cost and economic analysis research.
Logistical
Develop specific training and collaborative opportunities for chiropractic investigators with established health care economics researchers and organizations.
Emphasize and develop research issues with practical relevance to foster improvements in clinical efficiency in collaboration with chiropractic teaching institutions.
Internal agents (within the chiropractic profession,
its institutions and organizations)
Chiropractic college research departments and individuals
Funding organizations and foundations (eg, FCER, CCCR)
Independent chiropractic scientists and/or research centers
Grant writers and managers
External Agents
Academic and policy centers for health care economics
Public sector (federal and/or state) funding agencies (eg, HRSA, NIH, AHRQ)
Private agencies and foundations (including health reimbursement organizations)
Academic health policy institutions
Recommendation 3: Determine What Barriers Exist to the Appropriate Use of Chiropractic Services
Conduct descriptive studies to assess beliefs and opinions toward chiropractic among policy makers and health purchasers.
Identify relevant constituencies, organizations, and decision makers that address chiropractic coverage and use issues.
Systematically develop consistent and relevant strategies for chiropractic groups to function as constructive community resources in policy development.
Rationale
Barriers to appropriate use of chiropractic services may arise from different sources. Beliefs and practices of “customers” who do (and do not) use chiropractic services need to be assessed. Of particular interest are beliefs and opinions of health policy decision makers and the role that existing approaches to communication regarding chiropractic services by individual practitioners and chiropractic organizations have played in shaping them.
Actions RequiredTechnical
Develop and validate instruments and processes to assess beliefs, attitudes, and practices regarding use of chiropractic services.
Develop a series of research projects to initially identify and assess barriers to use among patients, payers and purchasers, policy makers, providers, and appropriate others.
Logistical
Develop proposals incorporating multidisciplinary research teams and multistage pilots where appropriate.
Political leaders within the chiropractic profession may have particular interest in facilitating better understanding of use barriers and formulation of constructive strategies to overcome them both internally and externally.
Internal agents (within the chiropractic profession,
its institutions and organizations)
Chiropractic political organizations (eg, International Chiropractors Association [ICA], American Chiropractic Association [ACA], Congress of Chiropractic State Associations [COCSA])
Chiropractic regulatory and policy organizations (eg, FCLB, NBCE)
Funding organizations and foundations (eg, FCER, CCCR)
External Agents
Private sector health purchasers
Organizations with perceived interest in chiropractic health
services research issues:
Chiropractic colleges
National trade groups (ACA, ICA)
State trade groups (COCSA, state associations)
National regulatory/policy groups (Federation of Chiropractic Licensing Boards [FCLB], National Board of Chiropractic Examiners [NBCE])
Private insurers (third parties, managed care organizations, plans, networks)
Health purchasers (employer groups, governments)
Federal policy and research agencies (HRSA, AHRQ)
Non-DC academic policy centers
Stimulating research interest and projects
Request for interests.
Request for development of proposals with funders.
References:
Mootz, RD, Coulter, ID, and Hansen, DT.
Health Services Research Related to Chiropractic: Review and Recommendations
for Research Prioritization by the Chiropractic Profession
J Manipulative Physiol Ther. 1997 (Mar); 20 (3): 201–217Nyiendo, J, Haas, M, and Hondras, MA.
Outcomes Research in Chiropractic: The State of the Art and Recommendations
for the Chiropractic Research Agenda
J Manipulative Physiol Ther. 1997 (Mar); 20 (3): 185–200Sawyer, C, Haas, M, Nelson, C, and Elkington, W.
Clinical research within the chiropractic profession: status, needs and recommendations.
J Manipulative Physiol Ther. 1997; 20: 169–178Adams, AH and Gatterman, M.
The state of the art of research on chiropractic education.
J Manipulative Physiol Ther. 1997; 20: 179–184Brennan, PC, Cramer, GD, Kirstukas, SJ, and Cullum, ME.
Basic Science Research in Chiropractic:
The State of the Art and Recommendations for a Research Agenda
J Manipulative Physiol Ther. 1997 (Mar); 20 (3): 150–168Consumer Reports.
The mainstreaming of alternative medicine.
Consumer Reports May 2000;17-25.Cooper, RA.
Health care workforce for the twenty-first century: the impact of nonphysician clinicians.
Annu Rev Med. 2001; 52: 51–61Christensen, MG, Kollasch, MW, Ward, R, Webb, KR, Day, AA, and zumBrunnen, J.
Job Analysis of Chiropractic 2005
A project report, survey analysis, and summary of the practice of chiropractic within the United States.
National Board of Chiropractic Examiners, Greeley (CO); 2005Rupert, RL, Manello, D, and Sandefur, R.
Maintenance Care: Health Promotion Services Administered to US Chiropractic Patients
Aged 65 and Older, Part II
J Manipulative Physiol Ther 2000 (Jan); 23 (1): 10–19Cherkin, DC, Deyo, RA, Sherman, KJ, Hart, LG, Street, JH, Hrbek, A et al.
Characteristics of Visits to Licensed Acupuncturists, Chiropractors, Massage Therapists,
and Naturopathic Physicians
J Am Board Fam Pract. 2002 (Nov); 15 (6): 463-472Cooper, RA and McKee, HJ.
Chiropractic in the United States: trends and issues.
Q Milbank. 2003; 81: 107–138Kelner, MJ, Boon, H, Wellman, B, and Welsh, S.
Complementary and alternative groups contemplate the need for effectiveness, safety and cost-effectiveness research.
Complement Ther Med. 2002; 10: 235–239Hurwitz, EL, Coulter, ID, Adams, AH, Genovese, BJ, and Shekelle, PG.
Utilization of chiropractic services in the United States and Canada.
Am J Public Health. 1998; 88: 771–776Tindle, HA, Davis, RB, Phillips, RS, and Eisenberg, DM.
Trends in use of complementary and alternative medicine by US adults: 1997-2002.
Altern Ther Health Med. 2005; 11: 42–49Barnes PM , Powell-Griner E , McFann K , Nahin RL:
Complementary and Alternative Medicine Use Among Adults:
United States, 2002
Advance Data 2004 (May 27); 343: 1–19Coulter, ID, Hurwitz, EL, Adams, AH, Genoves, BJ, Hays, R, and Shekelle, PG.
Patients Using Chiropractors in North America:
Who Are They, and Why Are They in Chiropractic Care?
SPINE (Phila Pa 1976) 2002 (Feb 1); 27 (3): 291–298Ong, C-K, Doll, H, Bodeker, G, and Stewart-Brown, S.
Use of osteopathic and chiropractic services among people with back pain: a UK population survey.
Health Soc Care Community. 2004; 12: 265–273Paramore, LC.
Use of alternative therapies: estimates from the Robert Wood Johnson Foundation Nation Access to Care survey.
J Pain Symptom Manage. 1997; 13: 83–89Rao, JK, Kroenke, K, Mihaliak, KA, Grambow, SC, and Weinberger, M.
Rheumatology patients' use of complementary therapies: results from a one-year longitudinal study.
Arthritis Rheum. 2003; 49: 619–625Coulter ID, Hurwitz EL, Aronow HU, Cassata DM, Beck JC.
Chiropractic Patients in a Comprehensive Home-Based Geriatric Assessment, Follow-up
and Health Promotion Program
Topics In Clinical Chiropractic 1996 (Jun): 3 (2): 46–55Scheurmier, N and Breen, AC.
A pilot study of the purchase of manipulation services for acute low back pain in the United Kingdom.
J Manipulative Physiol Ther. 1998; 21: 14–18Thomas, KJ, Nicholl, JP, and Coleman, P.
Use and expenditure on complementary medicine in England: a population based survey.
Complement Ther Med. 2001; 9: 2–11Sharma, R, Haas, M, and Stano, M.
Patient attitudes, insurance and other determinants of self-referral to medical and chiropractic physicians.
Am J Public Health. 2003; 93: 2111–2117Sherman, KJ, Cherkin, DC, Connelly, MT, Erro, J, Savetsky, JB, Davis, RB et al.
Complementary and Alternative Medical Therapies for Chronic Low Back Pain:
What Treatments Are Patients Willing To Try?
BMC Complement Altern Med. 2004 (Jul 19); 4: 9Smith, M and Parry, A.
The practice of chiropractic in health professional shortage areas in Missouri.
J Neuromusculoskel Syst. 1998; 6: 17–23Smith, M and Carber, L.
Chiropractic healthcare in health professional shortage areas (HPSAs) of the U.S..
Am J Public Health. 2002; 92: 2001–2009Cherkin, DC, Deyo, RA, Sherman, KJ, Hart, LG, Street, JH, Hrbek, A et al.
Characteristics of Visits to Licensed Acupuncturists, Chiropractors, Massage Therapists,
and Naturopathic Physicians
J Am Board Fam Pract. 2002 (Nov); 15 (6): 463-472Cote, P, Clarke, J, Deguire, S, Frank, JW, and Yassi, A.
Chiropractors and return-to-work: the experiences of three Canadian focus groups.
J Manipulative Physiol Ther. 2001; 24: 309–316Johnson, WG, Baldwin, ML, and Butler, RJ.
The costs and outcomes of chiropractic and physician care for workers' compensation back claims.
J Risk Insur. 1999; 66: 185–205Jarvis, KB, Phillips, RB, and Danielson, C.
Managed care preapproval and its effect on the cost of Utah worker compensation claims.
J Manipulative Physiol Ther. 1997; 20: 372–376Folsom, BL and Holloway, RW.
Chiropractic care of Florida's workers' compensation claimants: access, costs, and administrative outcome trends from 1994-1999.
Top Clin Chiropr. 2002; 9: 33–53Research Oversight Council on Workers' Compensation, Med-FX, and LLC.
Striking the balance: analysis of the cost and quality of medical care in Texas workers' compensation.
Research Oversight Council on Workers' Compensation,
Austin (TX); 2001Victor, RA and Wang, W.
Patterns and cost of physical medicine: comparison of chiropractic and physician directed care (WC-02-07).
Workers Compensation Research Institute,
Cambridge (MA); 2002MGT of America, Inc.
Chiropractic Treatment of Workers' Compensation Claims in Texas
(Report commissioned by the Texas Chiropractic Association).
MGT of America, Inc., Tallahassee (FL); 2003Jay, TC, Jones, SL, Coe, N, and Breen, AC.
A chiropractic service arrangement for musculoskeletal complaints in industry: a pilot study.
Occup Med (Lond). 1998; 48: 389–395Baldwin ML, Cote P, Frank JW, et al.
Cost-effectiveness Studies of Medical and Chiropractic Care for
Occupational Low Back Pain. A Critical Review of the Literature
Spine J. 2001 (Mar); 1 (2): 138–147Legorreta, AP, Metz, RD, Nelson, CF, Ray, S, Chernicoff, HO, and Dinubile, NA.
Comparative Analysis of Individuals With and Without Chiropractic Coverage:
Patient Characteristics, Utilization, and Costs
Archives of Internal Medicine 2004 (Oct 11); 164 (18): 1985–1892Metz, RD, Nelson, CF, LeBrot, T, and Pelletier, KR.
Chiropractic Care: Is It Substitution Care or Add-on Care in Corporate Medical Plans?
J Occup Environ Med 2004 (Aug); 46 (8): 847–855Mosley, CD, Cohen, IG, and Arnold, RM.
Cost-effectiveness of chiropractic care in a managed care setting.
Am J Manag Care. 1996; 2: 280–282Sarnat, RL and Winterstein, J.
Clinical and Cost Outcomes of an Integrative Medicine IPA
J Manipulative Physiol Ther 2004 (Jun) ; 27 (5): 336–347Underwood M, UK BEAM Trial Team.
United Kingdom Back Pain Exercise and Manipulation (UK BEAM) Randomized Tial:
Effectiveness of Physical Treatments for Back Pain in Primary Care
British Medical Journal 2004 (Dec 11); 329 (7479): 1377–1384United Kingdom Back Pain Exercise and Manipulation (UK BEAM) Randomised Trial
Cost Effectiveness of Physical Treatments for Back Pain in Primary Care
British Medical Journal 2004 (Dec 11); 329 (7479): 1381–1385Skargren, EI, Carlsson, PG, and Oberg, BE.
One-year follow-up comparison of the cost and effectiveness of chiropractic and physiotherapy as primary management for back pain. Subgroup analysis, recurrence, and additional health care utilization.
Spine. 1998; 23: 1875–1883Cohen, LA, Manski, RJ, Magder, LS, and Mullins, CD.
A Medicaid population's use of physicians' offices for dental problems.
Am J Public Health. 2003; 93: 1297–1301Damiano, PC, Brown, ER, Johnson, JD, and Scheetz, JP.
Factors affecting dentist participation in a state Medicaid program.
J Dent Educ. 1990; 54: 638–643Christensen, MG, Kerkoff, D, and Kollasch, MW.
Job Analysis of Chiropractic 2000
a project report, survey analysis, and summary of the practice of chiropractic within the United States.
National Board of Chiropractic Examiners,
Greeley (CO); 2000Langworthy, J, Breen, A, Vogel, S, Collier, R, and Sutherland, G.
Manipulation services for NHS patients: precedents and future models for provision.
(Available from:) Institute for Musculoskeletal Research and Clinical Implementation,
Bournemouth, England; 2000
http://www.imrci.ac.uk/Publications/Exec_Summ/exec_summ.html)Hawk, CK, Long, CR, Boulanger, K, Morschhauser, E, and Fuhr, A.
Chiropractic care for patients 55 and over: report from a practice-based research program.
J Am Geriatr Soc. 2000; 48: 534–545Hawk, CK.
An evidence-based look at chiropractic: tailoring treatment for older adults.
J Gerontol Nurs. 2002; 27: 6–14Pelletier, KR, Astin, JA, and Haskell, WL.
Current trends in the integration and reimbursement of complementary and alternative medicine by managed care organizations (MCOs) and insurance providers: 1998 update and cohort analysis.
Am J Health Promot. 1999; 14: 125–133Pelletier KR, Astin JA.
Integration and reimbursement of complementary and alternative medicine by managed care and insurance providers: 2000 update and cohort analysis.
Altern Ther Health Med 2002;8(1):38-9, 42, 44.Mootz, RD, Hess, JA, and McMillin.
Valuation of chiropractic services: a status report and overview of the challenges of standardization.
Top Clin Chiropr. 1996; 3: 20–31Yeh, GY, Phillips, RS, Davis, RB, Eisenberg, DM, and Cherkin, DC.
Visit time as a framework for reimbursement: time spent with chiropractors and acupuncturists.
Altern Ther Health Med. 2003; 9: 88–94Hess, JA, Mootz, RD, Madden, CW, and Perrin, EB.
Establishment of total and intraservice work by chiropractic physicians in providing spinal manipulative therapy and evaluation and management services.
J Manipulative Physiol Ther. 1997; 20: 13–23Hess, JA and Mootz, RD.
Comparisons of work estimates by chiropractic physicians with those of medical and osteopathic providers.
J Manipulative Physiol Ther. 1999; 22: 280–291Hertzman-Miller RP, Morgenstern H, Hurwitz EL, et al.
Comparing the Satisfaction of Low Back Pain Patients
Randomized to Receive Medical or Chiropractic Care:
Results From the UCLA Low-back Pain Study
Am J Public Health 2002 (Oct); 92 (10): 1628–1633Breen A, Breen R.
Back Pain and Satisfaction with Chiropractic Treatment: What Role Does the Physical Outcome Play?
The Clinical Journal of Pain 2003 (Jul); 19 (4): 263–268Wickizer, TM, Franklin, G, Fulton-Kehoe, D, Turner, JA, Mootz, RD, and Smith-Weller, T.
Patient satisfaction, treatment experience, and disability outcomes in a population-based cohort of injured workers in Washington State: implications for quality improvement.
Health Serv Res. 2004; 39: 727–748Breen, A., Carrington, M., Collier, R., and Vogel, S.
Communication between general and manipulative practitioners: a survey.
Complement Ther Med. 2000; 8: 8–14Brussee, WJ, Assendelft, WJ, and Breen, AC.
Communication between general practitioners and chiropractors.
J Manipulative Physiol Ther. 2001; 24: 12–16Leboeuf-Yde, C, Andren, JA, Gernandt, M, and Malmqvist, S.
Interprofessional contacts between chiropractors and other health-care professionals in Sweden as seen from a chiropractic perspective.
J Manipulative Physiol Ther. 1997; 20: 241–245Konrad, TR, Fletcher, GS, and Carey, TS.
Interprofessional collaboration and job satisfaction of chiropractic physicians.
J Manipulative Physiol Ther. 2004; 27: 245–252Mootz, RD and Bielinski, LL.
Issues, barriers, and solutions regarding integration of CAM and conventional health care.
Top Clin Chiropr. 2001; 8: 26–32in: L.L. Bielinski, R.D. Mootz (Eds.)
Issues in the integration of complementary and alternative medicine.
Office of the Insurance Commissioner,
Olympia (WA); 2000Hanks, JW.
Chiropractic inclusion in complementary and alternative medicine clinics: analysis of current trends.
Top Clin Chiropr. 2001; 8: 20–25Cooperstein, R, Perle, SM, Gatterman, MI, Lantz, C, and Schneider, MJ.
Chiropractic technique procedures for specific low back conditions: characterizing the literature.
J Manipulative Physiol Ther. 2001; 24: 407–424Gatterman, MI, Cooperstein, R, Lantz, C, Perle, SM, and Schneider, MJ.
Rating specific chiropractic technique procedures for common low back conditions.
J Manipulative Physiol Ther. 2001; 24: 449–456Coulter, I, Hurwitz, E, Adams, A et al.
The Appropriateness of Manipulation and Mobilization
of the Cervical Spine PDF
Santa Monica, CA: RAND Corporation; 1996 Document No. MR-781-CR.Shekelle, PG, Coulter, I, Hurwitz, EL, Genovese, B, Adams, AH, Mior, SA et al.
Congruence Between Decisions to Initiate Chiropractic Spinal Manipulation
for Low Back Pain and Appropriateness Criteria in North America
Annals of Internal Medicine 1998 (Jul 1); 129 (1): 9–17Council on Chiropractic Practice.
Clinical practice guideline number 1
Vertebral Subluxation in Chiropractic Practice
Council on Chiropractic Practice/World Chiropractic Alliance,
Chandler (AZ); 1998International Chiropractors Association.
Recommended Clinical Protocols and Guidelines for the Practice of Chiropractic
International Chiropractors Association, Arlington (VA); 2000Cates, JR, Young, DN, Guerriero, DJ, Jahn, WT, Armine, JP, and Korbett, AB.
An independent assessment of chiropractic practice guidelines.
J Manipulative Physiol Ther. 2003; 26: 282–286Cates, JR, Young, DN, Guerriero, DJ, Jahn, WT, Armine, JP, and Korbett, AB.
Evaluating the Quality of Clinical Practice Guidelines
J Manipulative Physiol Ther 2001 (Mar); 24 (3): 170–176in: S Haldeman, D Chapman-Smith, D Petersen (Eds.)
Guidelines for Chiropractic Quality Assurance and Practice Parameters
Aspen Publishers, Gaithersburg (MD); 1993in: L Glass (Ed.)
Occupational medicine guidelines: evaluation and management of common health problems and functional recovery of workers. 2nd ed.
OEM Press, Beverly Farms (MA); 2004Deyo, RA, Schall, M, Berwick, DM, Nolan, T, and Carver, P.
Continuous quality improvement for patients with back pain.
J Gen Intern Med. 2000; 15: 647–655Mootz, RD, Hansen, DT, Souza, TA, Triano, JJ, and Weise, B.
Application of incremental change strategies in chiropractic and multidisciplinary clinical settings for quality improvement.
Qual Manag Health Care. 2000; 8: 42–64Breen, AC, Langworthy, J et al.
Primary care audit toolkit: acute back pain.
(Available from:)Institute for Musculoskeletal Research and Clinical Implementation,
Bournemouth, England; 2000
http://www.imrci.ac.uk/Back_Pain_Audit_Toolkit/BackPain/backpain.htmlTuchyna, T, Wilkinson, S, and Jacob, CS.
Compliance testing of medical diagnostic x-ray equipment: three years' experience at a major teaching hospital in Western Australia.
Australas Phys Eng Sci Med. 2002; 25: 22–30Cretin, S, Farley, DO, Dolter, KJ, and Nicholas, W.
Evaluating an integrated approach to clinical quality improvement: clinical guidelines, quality measurement, and supportive system design.
Med Care. 2001; 39: II70–II84Institute of Medicine Committee on Quality of Health Care in America.
Crossing the Quality Chasm: A New Health System for the 21st Century
Washington, DC: National Academies Press; 2001
Return to CHIROPRACTIC RESEARCH AGENDA
Since 1–01–2007


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |