

The Musculoskeletal Diagnosis Cohort:
Examining Pain and Pain Care Among VeteransThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Pain 2016 (Aug); 157 (8): 1696–1703 ~ FULL TEXT
OPEN ACCESS Joseph L Goulet, Robert D Kerns, Matthew Bair, William C Becker, Penny Brennan, Diana J Burgess et al,
Pain Research,
Informatics, Multi-morbidities, and Education Center (PRIME),
VA Connecticut Healthcare System,
West Haven, CT, USA.
Musculoskeletal disorders (MSDs) are highly prevalent, painful, and costly disorders. The MSD Cohort was created to characterize variation in pain, comorbidities, treatment, and outcomes among patients with MSD receiving Veterans Health Administration care across demographic groups, geographic regions, and facilities. We searched electronic health records to identify patients treated in Veterans Health Administration who had ICD-9-CM codes for diagnoses including, but not limited to, joint, back, and neck disorders, and osteoarthritis. Cohort inclusion criteria were 2 or more outpatient visits occurring within 18 months of one another or one inpatient visit with an MSD diagnosis between 2000 and 2011. The first diagnosis is the index date.
Pain intensity numeric rating scale (NRS) scores, comorbid medical and mental health diagnoses, pain-related treatments, and other characteristics were collected retrospectively and prospectively. The cohort included 5,237,763 patients; their mean age was 59, 6% were women, 15% identified as black, and 18% reported severe pain (NRS ≥ 7) on the index date. Nontraumatic joint disorder (27%), back disorder (25%), and osteoarthritis (21%) were the most common MSD diagnoses. Patients entering the cohort in recent years had more concurrent MSD diagnoses and higher NRS scores. The MSD Cohort is a rich resource for collaborative pain-relevant health service research.
Keywords: Pain, musculoskeletal disorders, mental health comorbidity, cohort studies, Veterans, epidemiology
From the FULL TEXT Article:
Introduction
The Veterans Health Administration (VHA) is the largest integrated healthcare system in the United States, serving nearly 10 million veterans between 2000 and 2011. As in the general population, [21] musculoskeletal disorders (MSD), including joint, back and neck disorders, osteoarthritis, and fractures are among the most prevalent and costly disorders affecting both veterans and active duty personnel. [9, 10, 26] The prevalence of low back pain among VHA patients is increasing more rapidly than depression or diabetes. [34] Among veterans of Operations Enduring Freedom, Iraqi Freedom, and New Dawn (OEF/OIF/OND), the prevalence of MSD has increased each year, especially among women. [18]
Musculoskeletal pain is common in adult populations, with up to 48% of men and 52% of women reporting persistent pain ‘all the time’ for at least one year. [17] According to a seminal report from the Institute of Medicine (IOM) as many as 100 million US adults currently experience chronic pain, at an estimated annual cost of $635 billion. [21] MSD will likely increase in incidence and prevalence given the aging of the US population. [37] However, little is known about the characteristics of patients with MSD, including the co-occurrence of other medical and mental health conditions, and whether rates of non-MSD comorbidities vary by the level of reported pain.
The VHA is ideally positioned to address these issues: it has one of the most comprehensive electronic health record (EHR) systems in the US which includes longitudinal clinical assessments (e.g. pain intensity screening), treatments, and outcomes data. [25, 31] Based on these data, the VHA maintains multiple disease-specific cohorts and registries that enable research and quality improvement initiatives. [2, 4, 6, 23, 33] These large, national longitudinal cohorts represent a census of VHA patients that avoids some of the problems of selected samples recruited for research studies or trials, and they provide a wealth of information for understanding chronic illness management. [11, 24] Of particular importance, the large size and lengthy follow-up also allows for detection of rare events occurring after years of observation, as well as examination of relationships within small but important subgroups.
Given the scarcity of epidemiologic data on the incidence, prevalence, and consequences of MSD, the IOM specifically called upon VHA and other healthcare organizations to improve their collection of and reporting on painful disorders. [21]
As one response to this recommendation, the MSD Cohort was constructed with three primary aims:1) create a comprehensive registry of veterans with MSD diagnoses,
2) assess variation in pain treatment and outcomes across demographic groups, geographic regions, and VHA facilities, and
3) estimate costs of MSD pain care.Here, we describe the creation of the MSD Cohort, and present data on socio-demographic and clinical characteristics of cohort members. We purposely chose a wide variety of MSD conditions, many of which are under-studied, and selected patients without presumption of or requirement for pain in order to examine pain intensity, including its absence, and variation over time and by patient, clinician, and facility characteristics. In this report we present data at the time of cohort entry; future studies will focus on longitudinal data.
Methods
Study population
We adapted an algorithm previously validated to identify veterans with specific conditions using VHA electronic clinical and administrative data sources. [23] Specifically, we searched for International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9CM) codes consistent with MSD, which were identified from a review of recent research literature. [8] We supplemented this list with additional codes that the MSD Cohort team believed were prevalent yet understudied in the VHA (e.g. temporomandibular disorders (TMD), and gout [29]). A total of 1,685 distinct ICD-9CM codes were identified, encompassing conditions of the back and neck, fractures, and degenerative disorders (Supplementary table).
We next searched VHA electronic clinical and administrative data for outpatient and inpatient records with an MSD diagnosis. To be included in the cohort, a veteran had to have two or more outpatient visits with an MSD diagnosis occurring within 18 months of each other, or one or more inpatient stays with an MSD diagnosis. The index date for entry into the cohort was the date of the patient’s first outpatient or inpatient MSD diagnosis. This algorithm was chosen because outpatient diagnostic codes are entered by the provider at the time of the clinical encounter, and we had concerns about the accuracy of a single outpatient code. Only one record is required for an inpatient stay since professional coders assign codes after medical record review, with the intent to be as comprehensive as possible as it influences VHA and independent carrier reimbursement. [14] To maximize representativeness, there were no other inclusion or exclusion criteria.
Given the need for a second confirmatory outpatient MSD diagnosis within 18 months, and to allow for identification of comorbid conditions occurring near the time of the MSD diagnosis, we present data only on veterans with an MSD index date between January 1, 2000 and December 31, 2011. A veteran could have had more than one MSD diagnosis on the index date. ICD-9CM codes for MSD conditions were grouped based on the cited literature (e.g.733.00 Osteoporosis, unspecified,
733.01 Senile osteoporosis,
733.02 Idiopathic osteoporosis,
733.03 Disuse osteoporosis, and
733.09 Other osteoporosisfor Osteoporosis) or using Agency for Healthcare Research and Quality (AHRQ) Clinical Classifications Software (CCS) for ICD-9-CM. [1]
Linkage with other clinical and administrative data
For those veterans identified with an MSD, we then obtained additional information from other VHA electronic data sources including demographic characteristics, such as age on the MSD index date, sex, and race/ethnicity. Because race/ethnicity data are frequently missing in VHA administrative data sources, [28] we include veterans with missing data under the subgroup ‘Missing’. We then searched for historical information, including the era of last military service (e.g. Korean War, Vietnam era).
We next searched VHA Vital Signs data for a pain intensity NRS score on the MSD index date. [12, 35] As recommended by VHA clinical practice guidelines, the NRS is used in routine clinical care to screen for pain by asking the patient “On a scale of 0 to 10, where 0 means no pain and 10 means the worst possible pain, what is your current pain level?” The NRS is a global measure of pain that does not ask the patient to attribute pain to specific diagnoses. When multiple NRS were recorded on the index date, we retained only the highest. An invalid NRS (e.g. 99) was considered as missing. We categorized NRS scores into four levels: 0, no pain; 1 to 3, mild; 4 to 6, moderate; and 7 or greater, severe, and report missing as a separate category. [16, 36] In addition, scores of four or greater are reported here as moderate to severe pain.
We then identified comorbid medical and mental health conditions including: hypertension (HTN), diabetes mellitus (DM), coronary artery disease (CAD), depressive disorder, post-traumatic stress disorder (PTSD), and addictive disorders. In accord with established VHA registries, depressive disorder was defined using ICD-9CM codes 296.2x, 296.3x, 298.0, 300.4, 309.0, 309.1, 311, 296.90, 296.99, 293.83, or 301.12. [38] All comorbid conditions were collected in the same manner as MSD diagnoses (i.e. required two or more outpatient codes within 18 months, or one or more inpatient code). However, only comorbid conditions noted in the year prior to and up to six months after the MSD index date were retained for the present analysis, as they were likely active at the time of the MSD diagnosis. Body mass index (BMI) was calculated from the height and weight recorded on the MSD index date, or within the year prior to or up to six months after if missing on the index date.
Longitudinal Data
The cohort was constructed to allow for longitudinal analyses by collecting retrospective data prior to the MSD index date and prospective data after. Retrospective data can be used, for example, to identify patients with sufficient prior visits in order to determine incident MSD diagnoses and potential risk factors. Prospective data, not presented in this report, will allow for future examinations of acute, episodic, or chronic conditions. Combined, such data can also be used to identify temporal sequences of events, such as depression diagnoses occurring before or after the MSD diagnosis. Data on cohort members are collected until the end of the currently available administrative data.
Additional data
Additional data on cohort members includes: VHA pharmacy dispenses, specific medication, dose, fill/refill date, length of fill, and medication quantity; date of death; VHA hospitalizations, admission and discharge diagnoses and lengths of stay; CPT procedure codes; VHA care provided by specific services such as general medicine or mental health; and non-VHA health services provided by fee-for-service and/or Medicaid/Medicare. Cohort updates, including the addition of new patients, are conducted on a regular basis.
Analysis
Analyses presented here focus on comparisons of patient characteristics across cohort entry years. Because the large sample size increases the likelihood of finding statistically significant differences that may not be clinically relevant, we focus on results that reflected at least 2% absolute difference or a 2–fold difference in overall proportions (e.g., 1% vs. 2%). All analyses were performed using SAS, version 9.4 (SAS Institute).
Human Subjects Protection
The MSD Cohort has been approved by the Institutional Review Boards of the VA Connecticut Healthcare System and the Yale School of Medicine and has been granted a HIPAA waiver and waiver of informed consent.
Results

Table 1 The MSD cohort currently includes data on 5,237,763 veterans diagnosed with one or more MSD diagnoses between 2000 and 2011, representing nearly 55% of the 9,567,189 VHA service users during that time. The majority (98.5%) met cohort inclusion criteria via outpatient diagnoses. Overall, 37.4% of cohort members were aged 65 or older, 6% were women, 73.6% identified as white, 15.4% as Black, and 4.7% as Hispanic (Table 1). Over 20% (n = 1,109,775) entered the cohort in 2000, with decreasing numbers in subsequent years. This is consistent with other observational cohorts, and likely reflects a high proportion of pre-existing, or prevalent, cases entering in the year 2000 relative to later years. Veterans entering in more recent years were on average younger, more likely to be women and to report Hispanic ethnicity than those entering in earlier years. Vietnam War era veterans constituted the largest proportion of military service eras in each year, remaining relatively stable at 35–39%. The proportion of patients who identified as Hispanic increased from 4.0% to 5.9%.
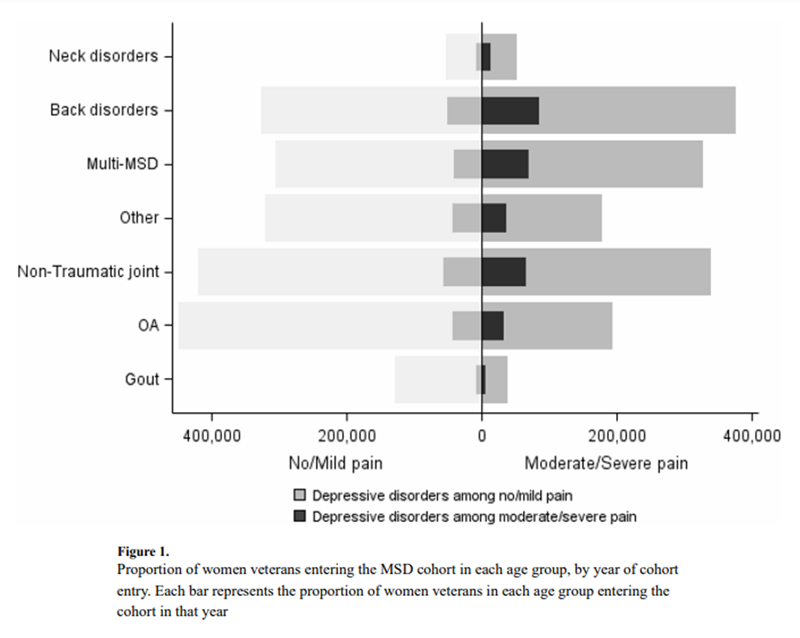
Figure 1

Table 2 Of the 314,266 women veterans in the cohort, 35.9% (n=112,838) were aged ≥50 on the index date, 13.9% (n=43,565) were ≥65, and 1.6% (n=5,092) were aged ≥85. The proportion age ≥65 entering decreased each year, from 22.8% in 2000 to 5.0% in 2011, with a corresponding increase in women under 40. (Figure 1) In bivariate analyses, women compared to men veterans (50.8% vs. 42.7%), black veterans compared to white veterans (57.3% vs. 40.4%), and Vietnam era service veterans compared to others (46.0% vs. 41.5%) were each significantly more likely to report moderate to severe pain (all p<0.0001). Veterans aged 65 and older compared to those 40 and younger were significantly less likely to report moderate to severe pain (29.9% vs. 55.2%).
Table 2 presents the proportion of veterans with specific MSD diagnoses by their cohort entry year. Each diagnosis represents those patients who met criteria for only that condition on the cohort entry date; patients meeting criteria for more than one MSD on the cohort entry date are included in the >1 MSD category. The top three diagnoses were: non-traumatic joint (26.5%); back (25.4%); and osteoarthritis (20.9%). Women veterans were significantly more likely to have non-traumatic joint (30.4%) and back (27.4%) disorders than men, but less likely to have osteoarthritis (12.8%) (all p<0.0001). While these three conditions remained the most common diagnoses throughout the 12 years in which cases were identified, their relative ranking changed. In year 2000, 15.8% of veterans entering the cohort had a non-traumatic joint disorder, 17.6% a back condition, and 21.5% an osteoarthritis diagnosis; while among entrants in 2011, 22.5% had a non-traumatic joint diagnosis, 18.8% a back condition diagnosis, and 9.0% an osteoarthritis diagnosis.
The proportion of veterans with two or more concurrent MSD diagnoses on the index date increased from 12.2% in 2000 to 20.3% in 2011. Among those with multiple MSD diagnoses, the median number of conditions was 2, and the most common were back disorders (49.8%) and non-traumatic joint disorders (47.8%). The most frequent combinations were back and non-traumatic joint (19.6%), and back and OA (11.9%).
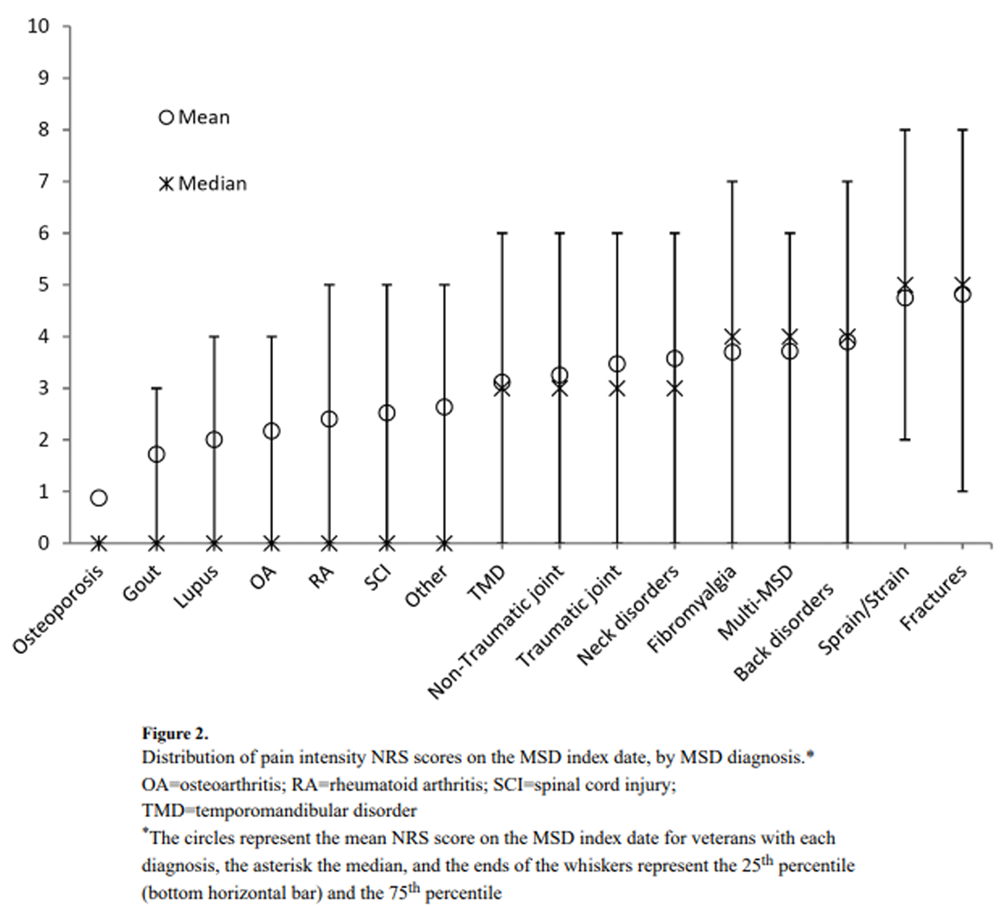
Figure 2

Table 3
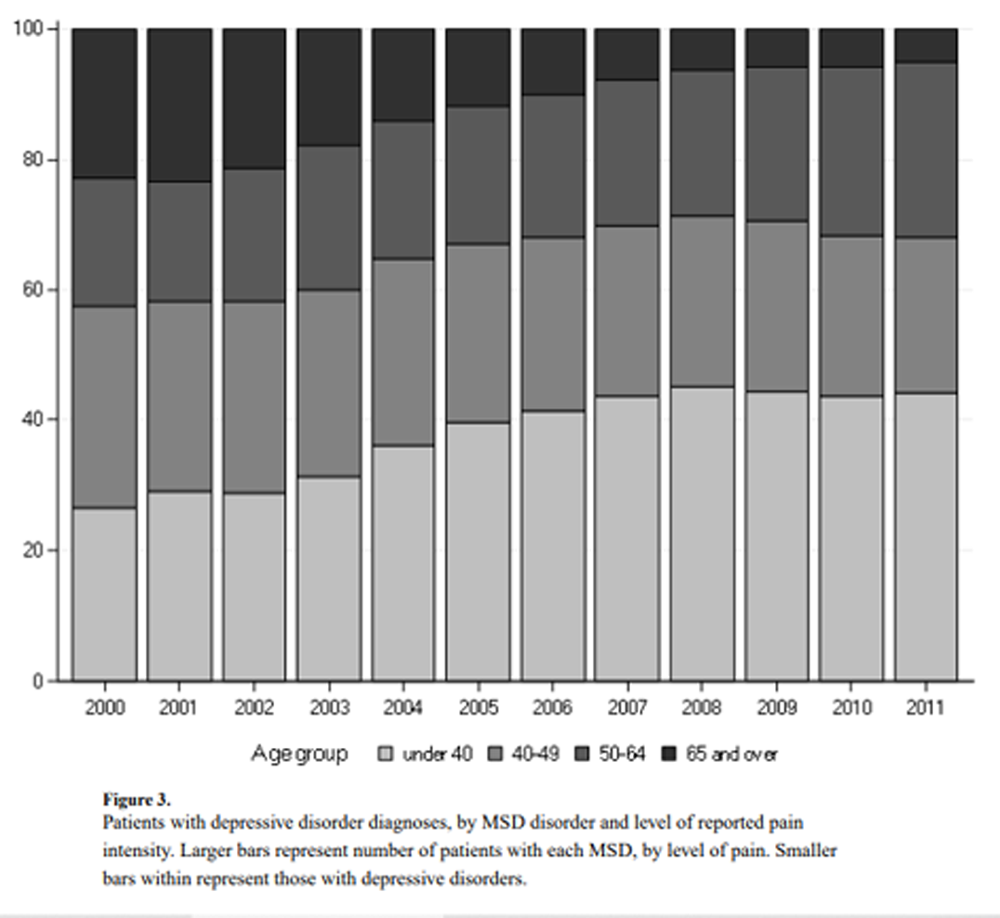
Figure 3 The proportion of veterans with available pain intensity NRS scores on the index date increased each year from 2000 on, as did the proportion reporting moderate or severe pain. Among veterans with NRS scores, there was substantial variation by MSD diagnosis. Figure 2 presents the mean, median, and interquartile range (IQR) of the NRS score on the index date, by each MSD diagnosis. As seen in Figure 2, veterans with a diagnosis of osteoporosis had the lowest average pain NRS score (mean=0.9, median=0, IQR=0), while veterans with sprains and strains or fractures had the highest score (mean = 4.8, median=5, IQR=7). Of note, those with back disorders had the next highest scores, followed by those with multiple MSD diagnoses.
Table 3 presents the prevalence of selected concurrent comorbid medical and mental health conditions active on the MSD index date. Overall, 48.0% of veterans in the cohort had a HTN diagnosis, 19.4% diabetes, and 16.2% CAD. Depressive disorder diagnoses were documented for 15.7% of the cohort overall: the prevalence increased from 13.6% to 19.9% between 2000 and 2011. Similarly, the overall prevalence of PTSD was 8.0%, increasing from 6.7% to 12.2%. Alcohol use disorders were also common, affecting between 6.0% and 8.6% of cohort entrants each year. The prevalence of diabetes, stroke, substance use diagnoses, and obesity/overweight remained relatively stable among new entrants over the cohort period, while the prevalence of chronic obstructive pulmonary disease decreased.
As an example of the relationships among specific MSD, specific comorbidities, and pain intensity, Figure 3 presents the number of veterans with depressive disorders, within each MSD diagnosis, by level of reported pain. The bars represent the number of veterans with each MSD diagnosis. The left side of the graph represents the number of veterans reporting no pain or mild pain (NRS <4) within each MSD. The darker bars within each represent those with a depressive disorder diagnosis. The largest number of veterans with depressive disorder diagnoses was among those with a diagnosis of back disorders who reported moderate to severe pain. While relatively few veterans had neck disorder MSD diagnoses, those with neck disorders reporting moderate to severe NRS pain scores (4–10) were most likely to have comorbid depressive disorder diagnoses. Veterans with gout were least likely to report moderate to severe pain, and least likely to have a depressive disorder diagnosis.
Discussion
We describe the creation of the VHA Musculoskeletal Disorders (MSD) cohort, a comprehensive registry of veterans in VHA care with MSD. The MSD cohort is responsive to a call from the IOM for VHA and other government and non-government healthcare organizations to capture data to improve the characterization of pain and its management. The MSD cohort is made possible by the availability of VHA’s comprehensive electronic health record (EHR). [22, 25] Available data include longitudinal diagnostic, health services use, and pharmacy data as well as routinely collected pain intensity ratings. Since establishing its “Pain as the fifth vital sign initiative” in 2000, VHA has required screening for the presence and intensity of pain at clinical encounters in which other vital signs are elicited and documented in the EHR. [31] Data from this study suggest increasing adherence to this requirement, with less than 15% of records failing to record an NRS on the MSD diagnosis date by 2011. Among veterans with a newly diagnosed MSD, the proportion reporting moderate to severe pain (NRS 4+) reached over 47% by 2011. Figure 2 characterizes the level of pain intensity commonly reported by veterans with different MSD at the time of diagnosis. This figure appears to reflect that, on average, acute conditions such as strains and fractures are associated with higher levels of current pain intensity. In contrast, these data remind us that many common degenerative MSD such as osteoarthritis and rheumatoid arthritis may not always be associated with reports of pain in the clinical setting. [16] It also further highlights the need to differentiate between acute, episodic, and chronic conditions, and to examine pain in a longitudinal context.
Consistent with US and international epidemiologic studies, MSD are also common and increasing in prevalence among veterans enrolled for care in VHA. Consistent with published data from community samples, the most commonly diagnosed MSD are non-traumatic joint disorders, back disorders and osteoarthritis (unspecified site). [7, 21, 30] Over time, diagnoses of non-traumatic joint disorders and back disorders increased, while the proportion of veterans with osteoarthritis diagnoses decreased. The proportion of veterans with neck disorders, although relatively small, also increased. Other studies within and outside of VHA have previously documented the increasing proportion of persons with back disorders. [13, 34] These observations raise questions about the etiology of these disorders and about factors associated with their increasing incidence and prevalence. Most troubling are observations that these disorders, particularly back conditions, are among the most debilitating health problems. [7] The fact that they appear to be emerging at a younger age is concerning.
Because the MSD cohort relies on diagnoses recorded in the VHA EHR, increasing percentages of MSD conditions over time may be explained by several factors. First, patients who are actively and routinely engaged in VHA services may be experiencing the onset of additional MSD conditions. Second, patients new to VHA, many of whom are younger veterans of recent conflicts, may be entering VHA with existing MSD conditions and requesting treatment. This may partly explain the observed drop in the age at first diagnosis. Finally, older veterans, Vietnam and post-Vietnam in particular, are using VHA services in increasing numbers as they age into Medicare coverage years. These veterans may also present to VHA with an existing MSD that is not incident. These observations have important scientific, practice and policy implications and encourage more focused investigation.
Veterans in care with MSD have substantial multi-MSD morbidity, pain, and mental health and medical comorbidities. Despite the decreasing age of the new veterans entering the cohort over time, the proportion with more than one MSD increased to over 22% by 2011. Observations about the commonality of co-occurring pain conditions including MSD have been cited as evidence supporting hypotheses about central nervous system mechanisms in the perpetuation of painful conditions and pain sensitivity. [39] A growing number of consensus statements from subject matter experts assert that in some circumstances, chronic pain may be best understood as a “disease” rather than a symptom. [21]
Medical and particularly mental health and substance use disorders are known to be highly co-prevalent with persistent pain conditions. Data from this large cohort confirm and extend these observations. Of particular importance are observations that an increasing proportion of veterans with MSD also have diagnosed comorbid mental health conditions. By 2011, for example, nearly 20% of veterans with newly diagnosed MSD had concurrent diagnosed depressive disorders, and co-prevalence rates of PTSD, other anxiety disorders and alcohol use disorders were also common. There is considerable speculation for these and similar observations about the co-occurrence of pain and other health related problems. [15, 20] Equally concerning is that among this sample of veterans with newly diagnosed MSD in 2011, the proportion that could be classified as overweight or obese was over 78%. Importantly, recent published research on veterans has focused on these comorbidities, and they report on the effectiveness of integrated approaches to treat chronic pain and depression or PTSD in this population. [27, 32] Perhaps due to public health attention to obesity, research has also emerged with a focus on chronic pain and overweight/obesity. [19] Data from this study encourage attention to anxiety and alcohol use disorders, as well. In contrast to these observations and despite considerable focus on the misuse and abuse of prescription pain medications in the recent past, there was little evidence of a trend in the co-prevalence of drug use disorders among veterans with MSD. [5]
Analyses reported here demonstrate the value of the MSD cohort as an opportunity to study complex interactions among socio-demographic and clinical characteristics of veterans with MSD, including the ability to examine changes over time. For example, Figure 1 reveals changes in the proportion of women veterans by age group over the years of observation, and highlights the ability to examine pain among women veterans across the age span. [3] Future analyses may examine clinical characteristics that are unique and reliably discriminate women from men within specific age ranges. Given the large and comprehensive nature of the MSD cohort, there are many additional opportunities to examine, for example, pain among veterans aged 85 and over, correlates of specific MSD such as temporomandibular disorders, variation in trajectories of pain by facility, the use of and outcomes associated with non-pharmacologic pain treatments.
Limitations
While the MSD cohort is a rich resource of data on MSD, there are limitations. First, as data are from an EHR that was not primarily intended for research, they are subject to the errors inherent in all clinical and administrative data, including missing or miscoding of diagnoses, vital signs, procedures, and medications. Second, the data cannot capture most healthcare and prescriptions provided outside the VHA system, so veterans who use both VHA and non-VHA healthcare will be under-represented. Third, the proportion of women in the cohort varies substantially from civilian samples with MSD. According to the VHA’s Office of Women’s Health Services, women comprised 6.5% of Veteran VHA patients in FY12 and the cohort reflects this overall number. While the proportion of women Veterans is increasing, they still represent a minority of users at this time. Fourth is the inability to capture a cohort member’s lifetime diagnostic history. While this limits conclusions about etiology and incidence, cohort members do represent patients whose diagnoses may be new to the VHA. Therefore, they are still valuable as a resource for understanding systemic variability, utilization patterns, quality of care, and cost to the VHA. Finally, since the VHA prioritizes patients with disabilities, who are older, and who have lower incomes, VHA patients as a group are not representative of the US population, and likely not of the veteran population as a whole. This limits generalizability of findings to those larger groups. However, the size and variation in the cohort suggests that although not completely generalizable, similar findings might be observed in other populations.
Conclusions
This report suggests that over 50% of all veterans receiving care in VHA facilities have diagnosed MSD and that the number is growing each year. The demographic and clinical characteristics of veterans with MSD are described and draw attention to several potentially important findings. For example, the observation that MSD, and multiple concurrent MSD, are increasingly being diagnosed among younger veterans is concerning and deserves further investigation. Examples also highlight the apparent complexities of interactions among individual difference variables such as age, race/ethnicity, and gender and reports of pain and diagnosis of co-occurring medical and mental health conditions. The MSD Cohort is a rich resource of information about pain and pain care in veterans and can serve as a platform for collaborative pain-relevant epidemiological and health service research. Data from this report may also encourage VHA’s sustained commitment to policy and practice initiatives designed to provide safe and effective care for the large proportion of veterans with MSD.
Supplementary Material
Supplementary Figures + Tables (68K, docx)
Acknowledgments
This work was supported by the Veterans Health Administration Health Services Research & Development grants CREATE 12-012 (Kerns, Goulet, Brandt PIs) and CIN 13-407 (Kerns PI)
Disclaimer:
The opinions expressed here are those of the authors and do not represent the official policy or position of the US Department of Veterans Affairs.
Conflicts of interest:
The authors declare that they have no conflicting interests.
References
Agency for Healthcare Research and Quality.
HCUP Clinical Classifications Software (CCS) for ICD-9-CM.
Rockville, MD: Healthcare Cost and Utilization Project (HCUP); 2014. 2006–2009Backus L, Mole L, Chang S, Deyton L.
The Immunology Case Registry.
Journal of clinical epidemiology. 2001;54(Suppl 1):S12–S15. S12–S15Bastian LA, Bosworth HB, Washington DL, Yano EM.
Setting the stage: Research to inform interventions, practice and policy
to improve women veterans' health and health care.
Journal of General Internal Medicine. 2013;28(Suppl 2):S491–S494. S491–S494Blow FC, Zeber JE, McCarthy JF, Valenstein M, Gillon L, Bingham CR.
Ethnicity and diagnostic patterns in veterans with psychoses.
Soc Psychiatry Psychiatr Epidemiol. 2004;39:841–851Bohnert AS, Ilgen MA, Trafton JA, Kerns RD, Eisenberg A, Ganoczy D, Blow FC.
Trends and regional variation in opioid overdose mortality among
Veterans Health Administration patients, fiscal year 2001 to 2009.
Clinical Journal of Pain. 2014;30:605–612Box TL, McDonell M, Helfrich CD, Jesse RL, Fihn SD, Rumsfeld JS.
Strategies from a nationwide health information
technology implementation: the VA CART story.
Journal of General Internal Medicine. 2010;25(Suppl 1):72–76. 72–76Centers for Disease Control and Prevention (CDC)
Prevalence and most common causes of disability among adults--United States, 2005.
MMWR Morb Mortal Wkly Rep. 2009;58:421–426Cherkin DC, Deyo RA, Volinn E, Loeser JD.
Use of the International Classification of Diseases (ICD-9-CM) to
identify hospitalizations for mechanical low back problems in administrative databases.
Spine (Phila Pa 1976) 1992;17:817–825Cohen SP, Brown C, Kurihara C, Plunkett A, Nguyen C, Strassels SA.
Diagnoses and factors associated with medical evacuation and return
to duty for service members participating in Operation Iraqi Freedom
or Operation Enduring Freedom: a prospective cohort study.
Lancet. 2010;375:301–309Cohen SP, Kapoor SG, Nguyen C, Anderson-Barnes VC, Brown C, Schiffer D.
Neck pain during combat operations:
an epidemiological study analyzing clinical and prognostic factors.
Spine (Phila Pa 1976) 2010;35:758–763Concato J, Shah N, Horwitz RI.
Randomized, controlled trials, observational studies,
and the hierarchy of research designs.
N Engl J Med. 2000;342:1887–1892Dobscha SK, Morasco BJ, Kovas AE, Peters DM, Hart K, McFarland BH.
Short-term variability in outpatient pain intensity scores in
a national sample of older veterans with chronic pain.
Pain Med. 2015;16:855–865Freburger JK, Holmes GM, Agans RP, Jackman AM, Darter JD, Wallace AS.
The rising prevalence of chronic low back pain.
Arch Intern Med. 2009;169:251–258Fultz SL, Skanderson M, Mole LA, Gandhi N, Bryant K, Crystal S, Justice AC.
Development and verification of a "virtual" cohort using
the National VA Health Information System.
Med Care. 2006;44:S25–S30Gatchel RJ.
Comorbidity of chronic pain and mental health disorders:
the biopsychosocial perspective.
Am Psychol. 2004;59:795–805Goulet JL, Brandt C, Crystal S, Fiellin DA, Gibert C, Gordon AJ.
Agreement between electronic medical record-based and self-administered
pain numeric rating scale: clinical and research implications.
Medical Care. 2013;51:245–250Gummesson C, Isacsson SO, Isacsson A, Andersson HI, Ektor-Andersen J.
The transition of reported pain in different body regions - a one-year follow-up study.
BMC Musculoskeletal Disorders. 2006;7:17Haskell SG, Ning Y, Krebs E, Goulet J, Mattocks K, Kerns R, Brandt C.
Prevalence of Painful Musculoskeletal Conditions in Female and Male
Veterans in 7 Years After Return From Deployment in
Operation Enduring Freedom/Operation Iraqi Freedom.
Clinical Journal of Pain. 2012;28:163–167Higgins DM, Buta E, Dorflinger L, Masheb RM, Ruser C, Goulet JL, Heapy A.
Prevalence and correlates of painful conditions and multi-morbidity
in a national sample of overweight/obese veterans.
Journal of Rehabilitation Research and Development. 2015 in pressHiggins DM, Kerns RD, Brandt CA, Haskell SG, Bathulapalli H, Gilliam W, Goulet JL.
Persistent pain and comorbidity among Operation Enduring Freedom/
Operation Iraqi Freedom/operation New Dawn veterans.
Pain Med. 2014;15:782–790Institute of Medicine (IOM)
Relieving Pain in America: A Blueprint for Transforming Prevention,
Care, Education, and Research
Washington, DC: The National Academies Press, 2011.Jha AK, Perlin JB, Kizer KW, Dudley RA.
Effect of the transformation of the Veterans Affairs
Health Care System on the quality of care.
N Engl J Med. 2003;348:2218–2227Justice AC, Dombrowski E, Conigliaro J, Fultz SL, Gibson D, Madenwald T.
Veterans Aging Cohort Study (VACS): Overview and description.
Medical Care. 2006;44(Suppl-24)Justice AC, Erdos J, Brandt C, Conigliaro J, Tierney W, Bryant K.
The Veterans Affairs Healthcare System:
A unique laboratory for observational and interventional research.
Medical Care. >2006;44(8 Suppl 2):S7–S12Kizer KW, Dudley RA.
Extreme Makeover: Transformation of the Veterans Health Care System.
Annu Rev Public Health. 2009;30:313–339Knox J, Orchowski J, Scher DL, Owens BD, Burks R, Belmont PJ.
The incidence of low back pain in active duty
United States military service members.
Spine (Phila Pa 1976) 2011;36:1492–1500Kroenke K, Bair MJ, Damush TM, Wu J, Hoke S, Sutherland J, Tu W.
Optimized antidepressant therapy and pain self-management in primary
care patients with depression and musculoskeletal pain:
a randomized controlled trial.
JAMA. 2009;301:2099–2110Long JA, Bamba MI, Ling B, Shea JA.
Missing race/ethnicity data in Veterans Health Administration
based disparities research: a systematic review.
J Health Care Poor Underserved. 2006;17:128–140Malik A, Dinnella JEFAU, Kwoh CKFAU, Schumacher HR.
Poor validation of medical record ICD-9 diagnoses of gout in a veterans affairs database.
J Rheumatol. 2009;36(6):1283–1286National Center for Health Statistics.
Hyattsville (MD): National Center for Health Statistics (US);
2011. Health, United States, 2010: With Special Feature on Death and DyingNational Pain Management Coordinating Committee.
Pain as the 5th Vital Sign Toolkit, revised edition.
Veterans Health Administration; 2000.
http://www1.va.gov/pain_management/docs/TOOLKIT.pdfOtis JD, Keane TM, Kerns RD, Monson C, Scioli E.
The development of an integrated treatment for veterans with
comorbid chronic pain and posttraumatic stress disorder.
Pain Med. 2009;10:1300–1311Pfeiffer PN, Szymanski BR, Valenstein M, McCarthy JF, Zivin K.
Trends in antidepressant prescribing for new episodes of depression
and implications for health system quality measures.
Med Care. 2012;50:86–90Sinnott P, Wagner TH.
Low Back Pain in VA Users.
Arch Intern Med. 2009;169:1338–133bStrong J, Ashton R, Chant D.
Pain intensity measurement in chronic low back pain.
Clin J Pain. 1991;7:209–218Tan G, Jensen MP, Thornby JI, Rintala DH, Anderson KO.
Categorizing pain in patients seen in a veterans health
administration hospital: Pain as the fifth vital sign.
Psychological Services. 2008:239–250Tsang A, Von KM, Lee S, Alonso J, Karam E, Angermeyer MC, Borges GL.
Common chronic pain conditions in developed and developing countries:
gender and age differences and comorbidity with depression-anxiety disorders.
J Pain. 2008;9:883–891Valenstein M.
The promise of large, longitudinal data sets.
Psychiatr Serv. 2013;64:503Woolf CJ.
Central sensitization: implications for the diagnosis
and treatment of pain.
Pain. 2011;152:S2–S15.
Return to SPINAL PAIN MANAGEMENT
Return to CHIROPRACTIC CARE FOR VETERANS
Since 12-17-2022


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |