

What Does Best Practice Care for Musculoskeletal Pain
Look Like? Eleven Consistent Recommendations From
High-quality Clinical Practice Guidelines:
Systematic ReviewThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: British J Sports Medicine 2020 (Jan); 54 (2): 79–86 ~ FULL TEXT
OPEN ACCESS Ivan Lin, Louise Wiles, Rob Waller, Roger Goucke, Yusuf Nagree, Michael Gibberd, Leon Straker, et. al.
WA Centre for Rural Health,
University of Western Australia,
Geraldton, Western Australia, Australia.
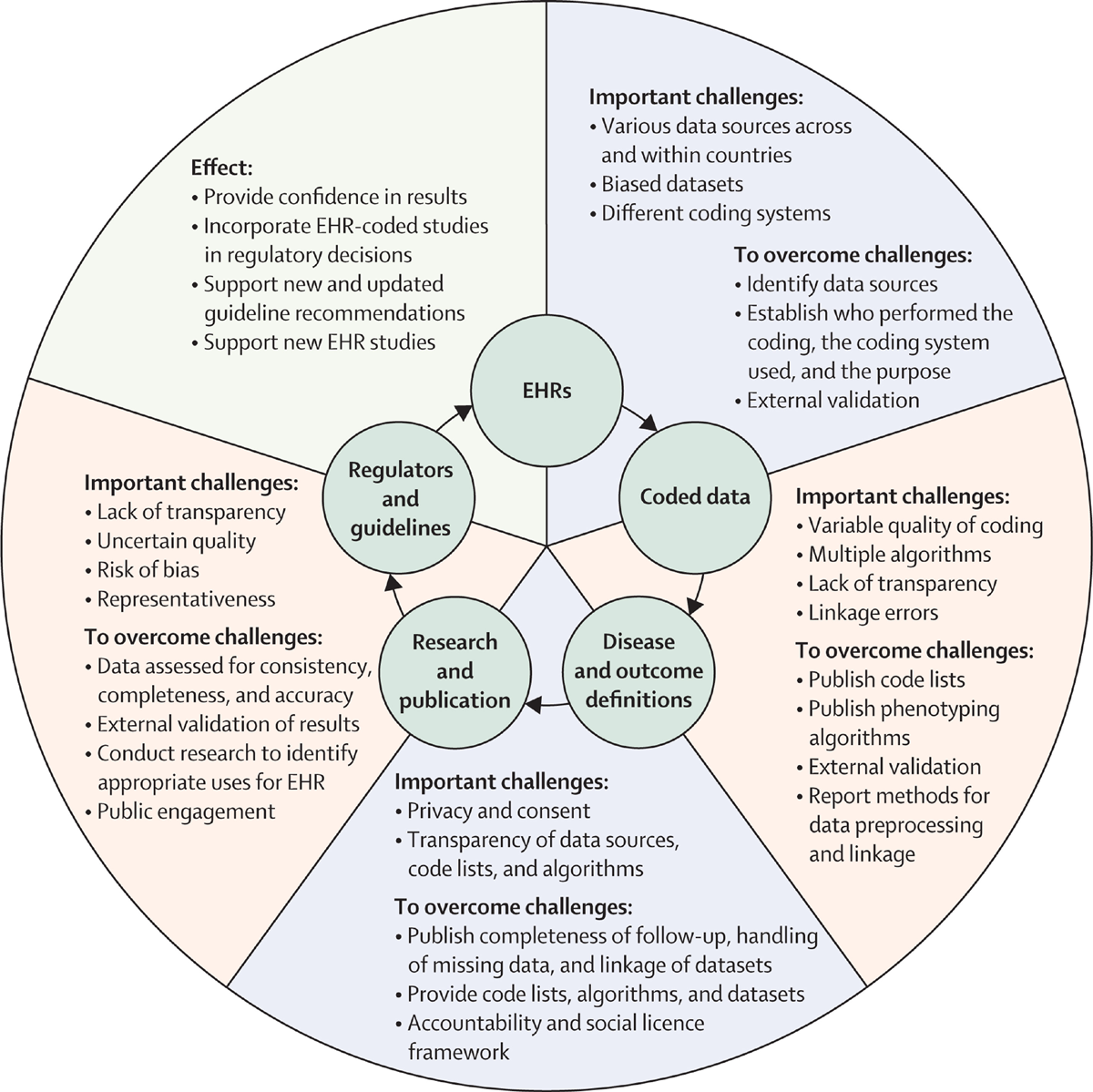
Lancet Digit Health 2022Objectives: To identify common recommendations for high-quality care for the most common musculoskeletal (MSK) pain sites encountered by clinicians in emergency and primary care (spinal (lumbar, thoracic and cervical), hip/knee (including osteoarthritis [OA] and shoulder) from contemporary, high-quality clinical practice guidelines (CPGs).
Design: Systematic review, critical appraisal and narrative synthesis of MSK pain CPG recommendations.
Eligibility criteria: Included MSK pain CPGs were written in English, rated as high quality, published from 2011, focused on adults and described development processes. Excluded CPGs were for: traumatic MSK pain, single modalities (eg, surgery), traditional healing/medicine, specific disease processes (eg, inflammatory arthropathies) or those that required payment.
Data sources: Four scientific databases (MEDLINE, Embase, CINAHL and Physiotherapy Evidence Database) and four guideline repositories.
Results: 6,232 records were identified, 44 CPGs were appraised and 11 were rated as high quality (low back pain: 4, OA: 4, neck: 2 and shoulder: 1). We identified 11 recommendations for MSK pain care: ensure care is patient centred, screen for red flag conditions, assess psychosocial factors, use imaging selectively, undertake a physical examination, monitor patient progress, provide education/information, address physical activity/exercise, use manual therapy only as an adjunct to other treatments, offer high-quality non-surgical care prior to surgery and try to keep patients at work.
Conclusion: These 11 recommendations guide healthcare consumers, clinicians, researchers and policy makers to manage MSK pain. This should improve the quality of care of MSK pain.
Keywords: education; effectiveness; evidence based; knowledge translation; review.
From the FULL TEXT Article:
Background

Box 1 Musculoskeletal pain (MSK) conditions are the biggest cause of disability internationally [1] and a major societal burden. One contributor to this burden, which is becoming increasingly recognised, is poor quality healthcare. [2] Common healthcare problems for MSK pain are summarised in Box 1 and include overuse of radiological imaging, surgery and opioids and a failure to provide patients with education and advice.
Evidence-to-practice gaps such as these are problematic because they waste healthcare resources and prevent patients from receiving appropriate care.
One of the ‘foundations of efforts to improve healthcare’, [3] and to reduce evidence-to-practice gaps, are clinical practice guidelines (CPGs). CPGs are ‘statements that include recommendations intended to optimise patient care that are informed by a systematic review of evidence and an assessment of the benefits and harms of alternative care options’. [4] CPGs aim to improve care in a number of ways including: guiding clinical and patient decision making, acting as a standard of care, contributing to the development of clinical decision-making aids, informing all stakeholders about what constitutes best practice and guiding allocation of healthcare resources. [4]
Care that is more concordant with CPG recommendations results in better patient outcomes and lower costs. [5, 6] However, CPGs have been criticised because clinicians have difficulty using them. Issues include: a multitude of CPGs for the one condition or when they are voluminous documents that are not user-friendly, [7] shortcomings in their quality such as when developers have undisclosed interests [8] and a lack of transparency in their development. [9] These problems are reflected in contemporary MSK pain CPGs. We recently reported that most MSK pain CPGs are of poor quality, use inconsistent terminology, over-represent some conditions (eg, low back pain [LBP] and osteoarthritis [ OA]) and under-representation other conditions (eg, cervical and thoracic spine pain) and fail to outline how to implement CPGs. [10] Nevertheless, we also identified a small number of higher quality CPGs that could be used to inform healthcare for MSK pain conditions.
There is increasing recognition that MSK pain conditions in different body areas share similarities with respect to mechanisms, prognostic factors and clinical course. [11, 12] We were interested in whether there was common ground among CPGs for MSK pain. We were also interested in recommendations of care across MSK pain conditions that could potentially be applied across different levels of healthcare (ie, primary, tertiary and emergency). Therefore, we aimed to identify a common set of recommendations, obtained from contemporary high-quality CPGs, to assess and manage a broad range of MSK pain conditions.
Methods
We undertook a systematic review and synthesis of contemporary MSK pain CPGs for three of the most common MSK pain sites [1, 13]: spinal pain (lumbar, thoracic and cervical spine), hip/knee pain including hip/knee OA and shoulder pain. The methods, including search strategy and selection processes, have been previously published. [10] We selected CPGs published within 5 years of the original search date (since 2011). This cut-off date was selected as CPGs developed or updated within the previous 5 years better reflect up-to-date research evidence. [4] The International Prospective Register of Systematic Reviews (PROSERO) registration number was CRD42016051653.
Our initial search included 34 CPGs that were developed between January 2011 and September 2016, for adults, in English, that reported development processes and were an original body of work. We excluded CPGs for: traumatic MSK pain, a single treatment modality (eg, surgery), traditional healing/medicine, specific disease processes (eg, inflammatory arthropathies) or those that were private for-profit and required payment to access. Article titles/abstracts were initially screened by one investigator (IL). Full text articles were then reviewed independently by two investigators (IL and LW). In August 2017, one investigator (IL) updated the search to identify any newly developed CPGs (online online supplementary file 1). The updated list was reviewed for completeness by all authors. Ten additional CPGs were included.
Appraisal
Three investigators (IL, LW and RW) independently appraised the quality of CPGs using the Appraisal of Guidelines for Research and Evaluation II (AGREE-II) instrument. The AGREE II instrument is the most widely used generic instrument to measure the development and reporting of CPGs and has acceptably high construct validity (significant differences in 18 of 21 item scores between high/low quality CPGs)14 and reliability (item internal consistency between 0.64 and 0.89). [14, 15]
Analysis
Using AGREE PLUS on the AGREE II website [16] individual item scores, domain scores (scope and purpose, stakeholder involvement, rigour of development, clarity of presentation, applicability and editorial independence) and overall AGREE II scores were calculated for each CPG. AGREE PLUS calculates domain and overall scores as a percentage of the maximum possible score. Data were entered and analysed using SPSS (IBM SPSS Statistics V.24.0). Means and SD for each of the 23 items (1–7 scale) and six domain scores (percentage) were calculated. Inter-rater agreement was determined using intraclass correlation coefficients (ICCs) with a two-way random effects model for each domain and overall rating scores. We classified level of agreement as poor (ICC <0.40), fair (ICC 0.40–0.59), good (ICC 0.60–0.74) or excellent (ICC 0.75–1.00). [17]
Similarly to our previous study, [10] we classified high-quality CPGs as those that had an AGREE II score equal to or greater than 50% of the maximum possible score in three domains: rigour of development (domain 3), editorial independence (domain 6) and stakeholder Involvement (domain 2). Our cut-off value of 50% is consistent with other studies, for example, ref [18], and the AGREE II developer’s recommendation that users decide on criteria for high and low quality CPGs based on the context of their work. [16]
CPG synthesis and identifying consistent recommendations
Synthesis consisted of four stages: extracting CPG recommendations, classifying recommendations, developing a narrative summary and, where possible, identifying consistent/common recommendations across MSK conditions. We also identified common recommendations within each MSK pain condition.
Extracting recommendations
Recommendations from high-quality CPGs were extracted independently by two reviewers (IL and either RW or LW). The evidence supporting each recommendation, as reported by each CPG, was recorded (eg, level of evidence and strength of recommendation). Extracted recommendations were compared and discrepancies resolved through discussion and consensus.
Classifying recommendations

Table 1 Two reviewers independently classified the recommendations. In order to accommodate the varying terminology used in different CPGs, we classified recommendations as ‘should do’, ‘could do’, ‘do not do’ or ‘uncertain’ (Table 1). CPGs for which there were no recommendations in a particular topic, that is, it was out-of-scope of the CPG and was not included, were not classified.
Narrative summary
A narrative summary was developed initially by one author (IL) and then reviewed and refined by all authors. This included grouping recommendations into theme areas. This was a deviation from our original PROSPERO protocol. In our original protocol, we proposed that two authors would independently undertake initial thematic analysis. The author group included three academic and practising physiotherapists (IL, RW and PPBO), two MSK pain researchers (CGM and LS), an indicator development researcher (LW), a specialist emergency care physician (YN), a senior medical officer in emergency medicine (MG) and a pain medicine physician (RG). We undertook multiple rounds of review with the summary refined following each round. For example, recommendations were reorganised with manual therapy and surgery initially classified under ‘physical therapies’ and ‘interventions’, and following review, classified under ‘passive interventions – non-invasive’ and ‘passive interventions – invasive’.
Identifying consistent recommendations
We identified consistent recommendations when there was a majority of ‘should do’ or ‘do not do’ recommendations and no conflicting recommendations in CPGs. Consistent recommendations applied across at least three MSK pain conditions. Additionally, we identified common recommendations within single MSK pain conditions based on the same criteria, a majority of ‘should do’ or ‘do not do’ recommendations in CPGs and no conflicting recommendations. We did not identify common recommendations when recommendations were weaker, that is, ‘could do’, ‘uncertain’ or there were conflicting recommendations.
Results
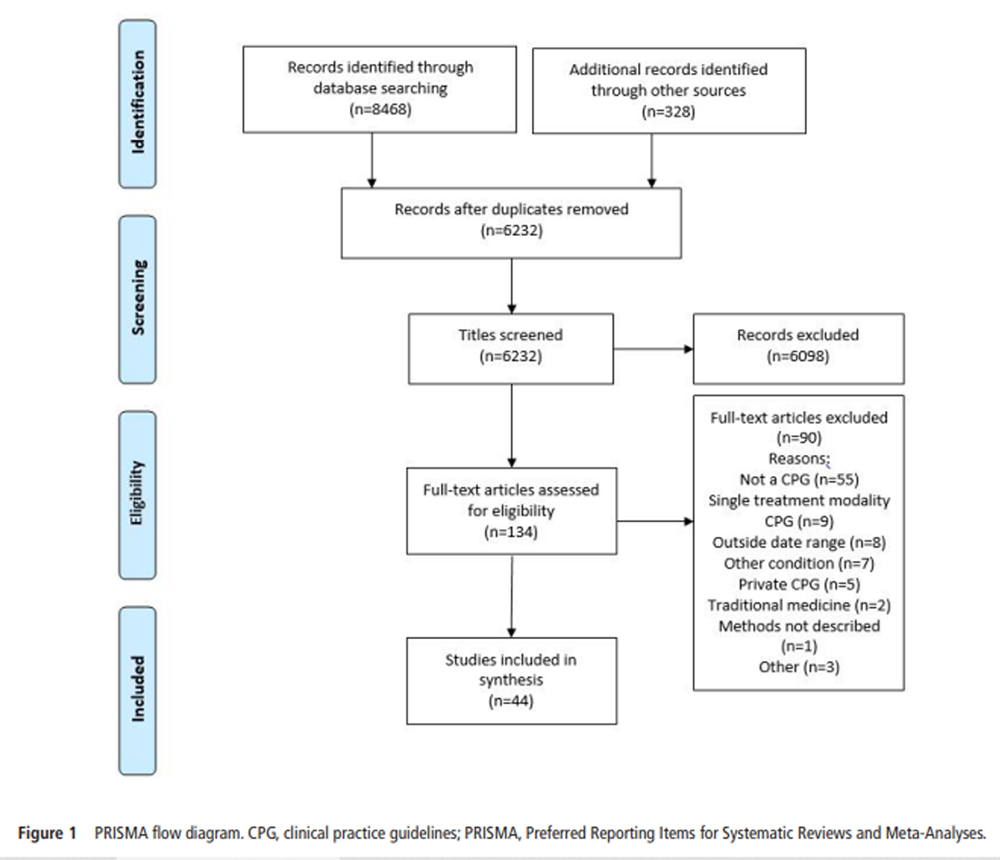
Figure 1 Our searches, including an updated search, identified 6,232 discrete records, from which 44 CPGs (34 CPGs initial search and 10 CPGs updated search) were selected for inclusion (Figure 1). Fifteen of the included CPGs were for LBP, 14 were for OA, 6 for shoulder conditions and 5 for the neck. We included single CPGs for the neck/thoracic spine, knee, ‘musculoskeletal injuries’ and lower limb (online online supplementary file 2).
Characteristics of included CPGs
With the exception of CPGs from Malaysia [19] and the Philippines, [20] all CPGs originated or involved panel members from high-income countries. CPGs were from 11 individual countries and ‘international’ collaborations, involving authors from multiple countries. Most were from the USA (n = 17), ‘international’ (n = 10) and Canada (n = 6). The Netherlands, UK and Italy each contributed two CPGs (online supplementary file 2).
CPGs from the USA were most commonly for LBP (n = 8), ‘international’ CPGs were most commonly for OA (n = 7), and half of Canadian CPGs were for neck pain (n = 3). The majority of CPGs were developed by medical societies (n = 23, 52.3%) which were either related to a profession/specialty group, [21], or MSK condition of interest, for example, ref [22].
Appraisal of CPGs: inter-rater agreement

Table 2

Table 3
Page 5

Box 2

Box 3 Inter-rater agreement was ‘fair’ for scope and purpose (domain 1), ‘good’ for clarity of presentation (domain 4) and ‘excellent’ for all other domains and overall AGREE II score (Table 2).
Appraisal of CPGs: quality
The mean (SD) AGREE II scores for each item, domain and overall scores across all guidelines are displayed in online online supplementary file 3. The domain with the lowest mean score was ‘Applicability’ (27.6%, SD = 18.3), and the highest mean score was for ‘Scope and Purpose’ (73.7%, SD = 13.8).
The AGREE II scores for each CPG are displayed in online online supplementary file 4. In our previous review, [10] eight high-quality MSK pain CPGs were identified for OA, [21–24] LBP, [25, 26] neck pain, [27] and shoulder pain. [28] Of the 10 additional CPGs identified in our updated search, three were rated as high-quality and included in our synthesis, including two for LBP [29, 30] and one for neck pain [31] (online supplementary file 3).
Consistent recommendations
Following synthesis (Table 3, online online supplementary file 5), 11 common/consistent recommendations were identified across MSK pain conditions (Box 2). NOTE: Box 3 is mentioned in Table 3.
Discussion
We identified 11 common recommendations for MSK pain care (box 2) that applied to patients with OA, LBP, neck pain and shoulder pain. These recommendations may provide clinicians, healthcare managers, funders, policy makers and researchers with a simple and clear consensus of current MSK pain priorities. In turn, this could help address the variable quality of clinical care delivered for MSK pain conditions. [34–36]
The common recommendations could be used in a number of ways to improve care. First, they could guide consumers in making informed healthcare decisions or assist them to identify when they are receiving suboptimal care. Second, clinicians could apply the recommendations to guide care decision making, to identify areas for learning and development and to assess their practice. Third, health services could assess the quality of care by applying them as minimum standards during clinical audit. Finally, a broader strategy (eg, for researchers, health planners/policy makers or funders) could be the continued development of the common recommendations into a set of quality indicators that could be used for reporting or to benchmark care quality. The recommendations could be used as a preliminary set of standards that could be refined via a rigorous, structured process. [37]
Our findings are similar to a recent review by Babatunde et al that was a synthesis of MSK pain management in primary care. [11] Recommended care included self-management advice, education and exercise as first-line treatments for MSK pain. The authors recommended short-term NSAIDs and opioids for pain relief provided risks and harms were considered. There was limited evidence for aids and devices (eg, taping and braces) and passive treatments (eg, acupuncture, transcutaneous electrical nerve stimulation and laser) and inconsistent evidence for surgery (equivalent to conservative care options in the longer term). [11] In contrast to our review, the authors reported support for psychosocial interventions, especially for those at risk of poor prognosis. We found that while CPGs in our review universally recommended psychosocial assessment, only LBP and neck pain CPGs reported on psychological treatments (‘could do’ recommendations for psychological therapies for LBP and contradictory recommendations for neck pain). Although our review included more recent CPGs, for example, [25–27, 29–31] CPGs for other common MSK pain conditions including OA and hip pain, Babatunde et al [11] included other sources of literature such as trials and systematic reviews. Psychological-informed management for MSK pain is an area that is currently lacking in CPGs.
Our review identified CPGs for LBP, OA, NAD and rotator cuff disorders. Arguably the common recommendations are relevant to other MSK pain conditions. For example, in tendinopathy, psychosocial factors are known predictors of outcome [38]; radiological imaging is of questionable clinical utility because of a moderate relationship between symptoms and outcome, [39] and high value non-surgical approaches to management such as education and exercise form the cornerstones of care. [40, 41] Although high-quality CPGs are currently lacking for other MSK pain conditions, we speculate that the consistent recommendations could be applied broadly to managing non-traumatic MSK pain.
Due to the potential for harm, an area we were interested in was opioid prescribing. We were unable to identify a consensus among CPGs relating to opioids, and there were conflicting recommendations both within and across MSK pain conditions. While there were conflicting views, almost all CPGs urged caution and/or discouraged opioid use. Recent research has reported no additional benefit of an opioid over a NSAID for acute LBP, [42] and further efficacy studies are underway. [43] Recent opioid-prescribing CPGs for patients with chronic pain [44, 45] recommend risk assessment to identify those at higher likelihood of opioid-related harms. Although outside the scope of this review, these recommendations should be considered by clinicians.
Our findings were similar to recent reviews of LBP management in emergency care. [46, 47] In emergency care, clinicians should use ‘red flags’ to assess the likelihood of serious pathology, apply judicious use of radiological imaging, identify psychosocial risk factors, provide targeted education and reassurance, offer exercise, cold and heat and promote early return to work and function. [46] The similarities of these recommendations and our findings suggest they could be applied in varied healthcare settings.
Results of our updated search reinforced our previous findings [10] that most MSK pain CPGs were of poor quality, which is a waste of resources. In addition to directing resources to fewer, higher quality CPGs, another way to reduce waste is for developers to focus on gaps in recommendations, areas for which there is currently limited consensus, and on other MSK pain conditions. As previously described, medication prescribing and psychologically oriented management of MSK pain are areas that lack research or have not been addressed by CPGs to date. CPGs targeting thoracic pain and non-OA knee pain are MSK pain areas that are lacking.
Limitations
The AGREE II instrument reflects methodological processes, not necessarily content, and scores may reflect reporting rather than methodological quality. The AGREE II developer’s suggest research groups identify their own criteria for CPG quality. [16] Our group defined high-quality CPGs as those who scored higher than 50% in three AGREE II domains. Although consistent with the AGREE II developer’s recommendations, investigator-developed criteria have the potential for bias by including or excluding CPGs based on non-empirically derived criteria. While a cut-off value of 50% is consistent with other studies, for example, [18] our criteria is somewhat generous when compared with some other reviewers for example. [48] CPGs were appraised by three authors and ideally four should be used. [14] Our research group was interprofessional; CPG appraisers were academic and clinical physiotherapists (IL and RW) and an indicator development researcher also with a background in physiotherapy (LW). Our synopsis of CPGs and interpretation of their recommendations (eg, as ‘should do’, ‘could do’ and so on), due to variations in the reporting and language of CPGs, relied on the interpretation of the research group. This is an inherent issue where there is heterogeneity in the way CPGs are conceptualised and their recommendations and underpinning evidence are presented. For example, some CPGs offer broad generalised recommendations [26] compared with others that address specific, highly targeted questions. [31] To account for this, we have ensured our interpretation and methodological steps have been clearly reported. As always, the search strategy may have failed to identify all relevant documents, and we only reviewed CPGs available in English. Nevertheless, our involvement of a reference librarian during searching and the experience of the research group means we are confident that relevant CPGs were included.
Conclusion
Variation in the quality of care is a barrier to providing high value musculoskeletal pain (MSK) care. Clinical practice guidelines (CPGs) are an important tool to address MSK pain care quality. We identified 11 consistent recommendations (Box 2) for the management of MSK conditions. These recommendations can be used by consumers, clinicians and at health services and policy levels to improve the quality of MSK pain care. Optimising the implementation of these recommendations comprises the next challenge.
Supplementary Online Files
Supplementary File 1 Medline searches undertaken
Supplementary File 2 Description of Clinical Practice Guidelines
Supplementary File 3 Overall mean (standard deviation) percentage scores
Supplementary File 4 CPG AGREE II domain scores and quality assessment (%)
Supplementary File 5 Narrative synthesis of CPG recommendationsAcknowledgments
We acknowledge Anne Smith for statistical assistance.
Contributors
All authors were involved in the conception, design and interpretation of data. IL, LW and RW performed the data analysis and initial interpretation. IL was responsible for initial writing and drafting of the article, which was reviewed by all authors. All authors revised critically for important intellectual content and approved the final version to be submitted.
Funding
IL is funded by an Australian National Health and Medical Research Council Early Career Fellowship (APP1090403). CGM’s fellowship (APP1103022) is funded by Australia’s National Health and Medical Research Council, and his research is supported by a Program Grant (APP1113532) and CRE Grant (APP1134856). LW works on a project funded by a National Health and Medical Research Council Program Grant (APP1054146).
Competing interests
None declared.
References
Disease GBD;
Global, Regional, and National Incidence, Prevalence, and Years Lived With
Disability for 328 Diseases and Injuries for 195 Countries, 1990-2016:
A Systematic Analysis for the Global Burden of Disease Study 2016
Lancet. 2017 (Sep 16); 390 (10100): 1211–1259Buchbinder R, van Tulder M, Öberg B, Costa LM, Woolf A, Schoene M, Croft P.
Low Back Pain: A Call For Action
Lancet. 2018 (Jun 9); 391 (10137): 2384–2388
This is the third of 3 articles in the remarkable Lancet Series on Low Back PainEccles MP , Grimshaw JM , Shekelle P , et al .
Developing Clinical Practice Guidelines: Reviewing, Reporting,
and Publishing Guidelines; Updating Guidelines; and the
Emerging Issues of Enhancing Guideline Implementability
and Accounting for Comorbid Conditions in Guideline Development
Implementation Science 2012 (Jul 4); 7: 62IOM (Institute of Medicine).
Clinical practice guidelines we can trust.
Washington (DC): National Academies Press, 2011.Childs JD , Fritz JM , Wu SS , et al
Implications of early and guideline adherent physical therapy for low back pain on utilization and costs.
BMC Health Serv Res 2015;15:15.
doi:10.1186/s12913-015-0830-3Rutten GM , Degen S , Hendriks EJ , et al
Adherence to clinical practice guidelines for low back pain
in physical therapy: do patients benefit?
Phys Ther 2010;90:1111–22.
doi:10.2522/ptj.20090173Baiardini I , Braido F , Bonini M , et al
Why do doctors and patients not follow guidelines?
Curr Opin Allergy Clin Immunol 2009;9:228–33.
doi:10.1097/ACI.0b013e32832b4651Williams MJ , Kevat DA , Loff B , et al
Conflict of interest guidelines for clinical guidelines.
Med J Aust 2011;195:442–5.
doi:10.5694/mja10.11130Scott IA , Guyatt GH
Clinical practice guidelines:
the need for greater transparency in formulating recommendations.
Med J Aust 2011;195:29.Lin I , Wiles LK , Waller R , et al
Poor overall quality of clinical practice guidelines
for musculoskeletal pain: a systematic review.
Br J Sports Med 2018;52:337–43.
doi:10.1136/bjsports-2017-098375Babatunde OO , Jordan JL , Van der Windt DA , et al .
Effective treatment options for musculoskeletal pain in primary care:
a systematic overview of current evidence.
PLoS One 2017;12:e0178621.
doi:10.1371/journal.pone.0178621Henschke N , Ostelo RW , Terwee CB , et al .
Identifying generic predictors of outcome in patients
presenting to primary care with nonspinal musculoskeletal pain.
Arthritis Care Res 2012;64:1217–24.
doi:10.1002/acr.21665Smith E, Hoy D, Cross M, et al.
The Global Burden of Other Musculoskeletal Disorders:
Estimates From the Global Burden of Disease 2010 Study
Ann Rheum Dis. 2014 (Aug); 73 (8): 1462–1469Brouwers MC , Kho ME , Browman GP , et al .
Development of the AGREE II, part 2:
assessment of validity of items and tools to support application.
CMAJ 2010;182:E472–8.
doi:10.1503/cmaj.091716Brouwers MC , Kho ME , Browman GP , et al .
Development of the AGREE II, part 1:
performance, usefulness and areas for improvement.
Can Med Assoc J 2010;182:1045–52.
doi:10.1503/cmaj.091714AGREE Enterprise.
AGREE: advancing the science of practice guidelines:
Canadian Institutes of Health Research. 2014
http://www.agreetrust.org/ (Accessed 29 Mar 2016).Cicchetti DV .
Guidelines, criteria, and rules of thumb for evaluating
normed and standardized assessment instruments in psychology.
Psychol Assess 1994;6:284–90.
doi:10.1037/1040-3590.6.4.284Bouwmeester W , van Enst A , van Tulder M , et al .
Quality of low back pain guidelines improved.
Spine 2009;34:2562–7.
doi:10.1097/BRS.0b013e3181b4d50dRosman A , Ismail A , Zain M , et al
Management of osteoarthritis. 2nd edn.
Putrajaya, Malaysia: Ministry of Health Malaysia, 2013.Philippine Academy of Rehabilitation Medicine.
Low back pain management guideline.
Quezon City, Philippines:
Philippine Academy of Rehabilitation Medicine (PARM), 2012.Jevsevar DS , Brown GA , Jones DL , et al .
Treatment of osteoarthritis of the knee:
evidence-based guideline - second edition.
Rosemont, IL: American Academy of Orthopaedic Surgeons, 2013.McAlindon TE , Bannuru RR , Sullivan MC , et al .
OARSI guidelines for the non-surgical management of knee osteoarthritis.
Osteoarthritis Cartilage 2014;22:363–88.
doi:10.1016/j.joca.2014.01.003Fernandes L , Hagen KB , Bijlsma JW , et al .
EULAR recommendations for the non-pharmacological core management
of hip and knee osteoarthritis.
Ann Rheum Dis 2013;72:1125–35.
doi:10.1136/annrheumdis-2012-202745National Institute for Health and Clinical Excellence (NICE).
Osteoarthritis: care and management (CG177).
London: National Institute for Health
and Clinical Excellence, 2014.National Institute for Health and Care Excellence (NICE):
Low Back Pain and Sciatica in Over 16s: Assessment and Management (PDF)
NICE Guideline, No. 59 2016 (Nov): 1–1067Globe G , Farabaugh RJ , Hawk C , et al .
Clinical Practice Guideline:
Chiropractic Care for Low Back Pain
J Manipulative Physiol Ther 2016 (Jan); 39 (1): 1–22Côté P , Wong JJ , Sutton D , et al
Management of Neck Pain and Associated Disorders:
A Clinical Practice Guideline from the Ontario Protocol
for Traffic Injury Management (OPTIMa) Collaboration
European Spine Journal 2016 (Jul); 25 (7): 2000–2022Hopman K , Krahe L , Lukersmith S , et al .
Clinical practice guidelines for the management of
rotator cuff syndrome in the workplace.
Port Macquarie (Australia):
University of New South Wales, 2013:80.Van Wambeke P , Desomer A , Ailiet L , et al .
Low Back Pain And Radicular Pain: Assessment And Management
KCE Report 287.
Belgian Health Care Knowledge Centre, (2017).Stochkendahl MJ , Kjaer P , Hartvigsen J , et al .
National Clinical Guidelines for Non-surgical Treatment of Patients
with Recent Onset Low Back Pain or Lumbar Radiculopathy
European Spine Journal 2018 (Jan); 27 (1): 60–75Bussières, AE, Stewart, G, Al Zoubi, F et al.
The Treatment of Neck Pain-Associated Disorders and
Whiplash-Associated Disorders: Clinical Practice Guideline
J Manipulative Physiol Ther. 2016 (Oct); 39 (8): 523–564Hill JC , Whitehurst DG , Lewis M , et al .
Comparison of Stratified Primary Care Management For Low Back Pain
With Current Best Practice (STarT Back): A Randomised Controlled Trial
Lancet. 2011 (Oct 29); 378 (9802): 1560–1571Linton SJ , Nicholas M , MacDonald S
Development of a short form of the Örebro Musculoskeletal
Pain Screening Questionnaire.
Spine 2011;36:1891–5.
doi:10.1097/BRS.0b013e3181f8f775Runciman WB , Hunt TD , Hannaford NA , et al .
CareTrack: assessing the appropriateness of health care delivery in Australia.
Med J Aust 2012;197:100–5.Buchbinder R , Staples MP , Shanahan EM , et al .
General practitioner management of shoulder pain in comparison with
rheumatologist expectation of care and best evidence: an Australian national survey.
PLoS One 2013;8:e61243.
doi:10.1371/journal.pone.0061243Williams CM, Maher CG, Hancock MJ et al.
Low Back Pain and Best Practice Care:
A Survey of General Practice Physicians
Archives of Internal Medicine 2010 (Feb 8); 170 (3): 271–277Campbell SM , Braspenning J , Hutchinson A , et al .
Research methods used in developing and applying
quality indicators in primary care.
Qual Saf Health Care 2002;11:358–64.
doi:10.1136/qhc.11.4.358Mallows A , Debenham J , Walker T , et al .
Association of psychological variables and outcome in tendinopathy:
a systematic review.
Br J Sports Med 2017;51:743–8.
doi:10.1136/bjsports-2016-096154Khan KM , Forster BB , Robinson J , et al .
Are ultrasound and magnetic resonance imaging of value in assessment
of Achilles tendon disorders? A two year prospective study.
Br J Sports Med 2003;37:149–53.
doi:10.1136/bjsm.37.2.149Coombes BK , Bisset L , Vicenzino B
Management of lateral elbow tendinopathy:
one size does not fit all.
J Orthop Sports Phys Ther 2015;45:938–49.
doi:10.2519/jospt.2015.5841Grimaldi A , Fearon A .
Gluteal tendinopathy: integrating pathomechanics and
clinical features in its management.
J Orthop Sports Phys Ther 2015;45:910–22.
doi:10.2519/jospt.2015.5829Friedman BW , Dym AA , Davitt M , et al .
Naproxen with cyclobenzaprine, oxycodone/acetaminophen, or placebo
for treating acute low back pain: a randomized clinical trial.
JAMA 2015;314:1572–80.
doi:10.1001/jama.2015.13043Lin CW , McLachlan AJ , Latimer J , et al .
OPAL: a randomised, placebo-controlled trial of opioid analgesia
for the reduction of pain severity in people with acute
spinal pain. Trial protocol.
BMJ Open 2016;6:e011278.
doi:10.1136/bmjopen-2016-011278Dowell D , Haegerich TM , Chou R .
CDC Guideline for prescribing opioids for chronic pain–United States, 2016.
JAMA 2016;315:1624–45.
doi:10.1001/jama.2016.1464The Diagnosis and Treatment of Low Back Pain Work Group.
VA/DoD Clinical Practice Guideline for Diagnosis
and Treatment of Low Back Pain PDF
Washington, DC: The Office of Quality, Safety and Value, VA, &
Office of Evidence Based Practice, U.S. Army MedicalCommand, 2017, Version 2.0.Strudwick K , McPhee M , Bell A , et al .
Review article: Best practice management of low back pain in the
emergency department (part 1 of the musculoskeletal injuries rapid review series).
Emerg Med Australas 2018;30:18–35.
doi:10.1111/1742-6723.12907Machado GC , Rogan E , Maher CG .
Managing non-serious low back pain in the emergency department:
time for a change?
Emerg Med Australas 2018;30:279–82.
doi:10.1111/1742-6723.12903Armstrong JJ , Rodrigues IB , Wasiuta T , et al .
Quality assessment of osteoporosis clinical practice guidelines
for physical activity and safe movement: an AGREE II appraisal.
Arch Osteoporos 2016;11:1–10.
doi:10.1007/s11657-016-0260-9Ivanova JI , Birnbaum HG , Schiller M , et al .
Real-world practice patterns, health-care utilization, and costs in
patients with low back pain: the long road to guideline-concordant care.
Spine J 2011;11:622–32.
doi:10.1016/j.spinee.2011.03.017Girish G , Lobo LG , Jacobson JA , et al .
Ultrasound of the shoulder: asymptomatic findings in men.
AJR Am J Roentgenol 2011;197:W713–19.
doi:10.2214/AJR.11.6971Adelani MA , Harris AH , Bowe TR , et al .
Arthroscopy for knee osteoarthritis has not decreased
after a clinical trial.
Clin Orthop Relat Res 2016;474:489.
doi:10.1007/s11999-015-4514-4Judge A , Murphy RJ , Maxwell R , et al .
Temporal trends and geographical variation in the use of subacromial
decompression and rotator cuff repair of the shoulder in England.
Bone Joint J 2014;96-B:70.
doi:10.1302/0301-620X.96B1.32556Ketola S , Lehtinen JT , Arnala I
Arthroscopic decompression not recommended in the treatment of rotator
cuff tendinopathy: a final review of a randomised controlled trial
at a minimum follow-up of ten years.
Bone Joint J 2017;99-B:799–805.
doi:10.1302/0301-620X.99B6.BJJ-2016-0569.R1Beard DJ , Rees JL , Cook JA , et al
Arthroscopic subacromial decompression for subacromial shoulder pain (CSAW):
a multicentre, pragmatic, parallel group, placebo-controlled,
three-group, randomised surgical trial.
The Lancet 2017.
doi:https://doi.org/10.1016/S0140-6736(17)32457-1Abdel Shaheed C , Maher CG , Williams KA , et al .
Efficacy, tolerability, and dose-dependent effects of opioid analgesics
for low back pain: a systematic review and meta-analysis.
JAMA Intern Med 2016;176:958.
doi:10.1001/jamainternmed.2016.1251Webster BS , Verma SK , Gatchel RJ
Relationship between early opioid prescribing for acute occupational
low back pain and disability duration, medical costs,
subsequent surgery and late opioid use.
Spine 2007;32:2127–32.
doi:10.1097/BRS.0b013e318145a731Sullivan MD , Howe CQ .
Opioid therapy for chronic pain in the United States:
promises and perils.
Pain 2013;154:S94–100.
doi:10.1016/j.pain.2013.09.009American Academy of Orthopaedic Surgeons.
Management of osteoarthritis of the hip: evidence-based clinical practice guideline.
Rosemont, Illinois, 2017.Hochberg MC , Altman RD , April KT , et al .
American College of Rheumatology 2012 recommendations for the use
of nonpharmacologic and pharmacologic therapies in
osteoarthritis of the hand, hip, and knee.
Arthritis Care Res 2012;64:465–74.
doi:10.1002/acr.21596Bruyère O , Cooper C , Pelletier JP , et al .
An algorithm recommendation for the management of knee osteoarthritis
in Europe and internationally: a report from a task force of the
European Society for Clinical and Economic Aspects
of Osteoporosis and Osteoarthritis (ESCEO).
Semin Arthritis Rheum 2014;44:253–63.
doi:10.1016/j.semarthrit.2014.05.014Bruyère O , Cooper C , Pelletier JP , et al .
A consensus statement on the European Society for Clinical and Economic
Aspects of Osteoporosis and Osteoarthritis (ESCEO) algorithm for the
management of knee osteoarthritis-from evidence-based
medicine to the real-life setting.
Semin Arthritis Rheum 2016;45:S3–11.
doi:10.1016/j.semarthrit.2015.11.010Peter WF , Jansen MJ , Hurkmans EJ , et al .
Physiotherapy in hip and knee osteoarthritis: development of a practice
guideline concerning initial assessment, treatment and evaluation.
Acta Reumatol Port 2011;36:268–81.Brosseau L , Wells GA , Tugwell P , et al .
Ottawa Panel evidence-based clinical practice guidelines for the management
of osteoarthritis in adults who are obese or overweight.
Phys Ther 2011;91:843–61.
doi:10.2522/ptj.20100104Brosseau L , Wells GA , Pugh AG , et al .
Ottawa Panel evidence-based clinical practice guidelines for
therapeutic exercise in the management of hip osteoarthritis.
Clin Rehabil 2016;30:935–46.
doi:10.1177/0269215515606198Goodman F , Kaiser L , Kelley C , et al .
VA/DoD clinical practice guideline for the non-surgical
management of hip and knee osteoarthritis:
Department of Veterans Affairs, Department of Defense, 2014:126.Qaseem A, Wilt TJ, McLean RM, Forciea MA;
Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain:
A Clinical Practice Guideline From the American College of Physicians
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 514–530Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, Weimer M, Fu R, Dana T.
Noninvasive Treatments for Low Back Pain
Agency for Healthcare Research and Quality (AHRQ)
Comparative Effectiveness Review Number 169 (Feb 2016)Delitto, A., George, S.Z., Van Dillen, L.R., Whitman, J.M., Sowa, G., Shekelle, P. (2012).
Low Back Pain: Clinical Practice Guidelines Linked to the International Classification
of Functioning, Disability, and Health from the Orthopaedic Section
of the American Physical Therapy Association
Journal of Orthopaedic & Sports Physical Therapy 2012; 42 (4): A1–A57Lee J , Gupta S , Price C , et al
Low back and radicular pain:
a pathway for care developed by the British Pain Society.
Br J Anaesth 2013;111:112–20.Cheng L , Lau K , Lam W , et al
Evidence-based guideline on prevention and management of
low back pain in working population in primary care.
The Hong Kong Practitioner 2012;34.State of Colorado Department of Labor and Employment:
Division of Worker’s Compensation.
Low back pain: medical treatment guidelines.
Denver, Colorado, 2014:112.Goertz M, Thorson D, Bonsell J, et al.
Adult Acute and Subacute Low Back Pain
Institute for Clinical Systems Improvement; Fifteenth Edition January 2012Kreiner DS , Hwang SW , Easa JE , et al .
An evidence-based clinical guideline for the diagnosis and treatment
of lumbar disc herniation with radiculopathy.
Spine J 2014;14:180–91.
doi:10.1016/j.spinee.2013.08.003Kreiner DS , Shaffer WO , Baisden JL , et al .
An evidence-based clinical guideline for the diagnosis and
treatment of degenerative lumbar spinal stenosis (update).
Spine J 2013;13:734–43.
doi:10.1016/j.spinee.2012.11.059Matz PG , Meagher RJ , Lamer T , et al .
Guideline summary review: an evidence-based clinical guideline for
the diagnosis and treatment of degenerative lumbar spondylolisthesis.
Spine J 2016;16:439–48.
doi:10.1016/j.spinee.2015.11.055Toward Optimized Practice (TOP) Program.
Evidence-informed primary care management of low back pain:
clinical practice guidelines. 3rd edn.
Alberta, Canada: Institute of Health Economics, 2015:49.State of Colorado Department of Labor and Employment:
Division of Worker’s Compensation. Shoulder injury: medical treatment guidelines.
Denver, Colorado, 2015:164.Diercks R , Bron C , Dorrestijn O , et al .
Guideline for diagnosis and treatment of subacromial pain syndrome:
a multidisciplinary review by the Dutch Orthopaedic Association.
Acta Orthop 2014;85:314–22.
doi:10.3109/17453674.2014.920991Eubank BH , Mohtadi NG , Lafave MR , et al .
Using the modified Delphi method to establish clinical consensus for the
diagnosis and treatment of patients with rotator cuff pathology.
BMC Med Res Methodol 2016;16:56.
doi:10.1186/s12874-016-0165-8Oliva F , Piccirilli E , Bossa M , et al .
I.S.Mu.L.T - Rotator cuff tears guidelines.
Muscles Ligaments Tendons J 2015;5:227.
doi:10.11138/mltj/2015.5.4.227Washington State Department of Labor and Industries.
Shoulder conditions: diagnosis and treatment guideline.
Washington, 2013:28.R. Bryans, P. Decina, M. Descarreaux, et al.,
Evidence-Based Guidelines for the Chiropractic Treatment
of Adults With Neck Pain
J Manipulative Physiol Ther 2014 (Jan); 37 (1): 42–63State of Colorado Department of Labor and Employment:
Division of Worker’s Compensation.
Cervical spine injury: medical treatment guidelines.
Denver, Colorado, 2014:96.Monticone M , Iovine R , de Sena G , et al .
The Italian Society of Physical and Rehabilitation Medicine
(SIMFER) recommendations for neck pain.
G Ital Med Lav Ergon 2013;35:36–50.Hegmann K , Travis R , Andersson GB , et al .
Cervical and thoracic spine disorders.
Elk Grove Village, Illinois, USA:
American College of Occupational and Environmental Medicine (ACOEM., 2016:1–711.Barton CJ , Lack S , Hemmings S , et al .
The ’Best Practice Guide to Conservative Management of Patellofemoral Pain':
incorporating level 1 evidence with expert clinical reasoning.
Br J Sports Med 2015;49:923–34.
doi:10.1136/bjsports-2014-093637Braddock E , Greenlee J , Hammer R , et al .
Manual medicine guidelines for musculoskeletal injuries.
Sonora (CA): Academy for Chiropractic Education, 2013:70.State of Colorado Department of Labor and Employment:
Division of Worker’s Compensation.
Lower extremity injury: medical treatment guidelines.
Denver, Colorado, 2016:264.Bussières AE , Patey AM , Francis JJ , et al .
Identifying factors likely to influence compliance with diagnostic
imaging guideline recommendations for spine disorders among chiropractors
in North America: a focus group study using the Theoretical Domains Framework.
Implement Sci 2012;7:82.
doi:10.1186/1748-5908-7-82
Return LOW BACK PAIN
Return to BEST PRACTICES
Return to SPINAL PAIN MANAGEMENT
Since 8-21-2022


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |