

Locating and Treating Low Back Pain of
Myofascial Origin by Ischemic CompressionThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Can Chiropr Assoc 2002 (Dec); 46 (4): 257–264 ~ FULL TEXT
OPEN ACCESS Guy Hains, DC
2930 Côte Richelieu,
Trois-Rivières-Ouest,
Canada.
The purpose of this article is to describe a method to identify and treat trigger points of myofascial origin by ischemic compression among patients with low back pain. In addition to a review of the literature, the author draws upon his own clinical experience to accomplish this goal. In general, thumb pressure is used for the identification, localization and treatment of trigger points and tender spots within the muscles of the lumbar, pelvic, femoral and gluteal areas. The management of low back pain of myofascial origin by ischemic compression can be used in any setting, without the need of specialized equipment. In addition to clinical effectiveness within a wide range of safety, this approach is easy on the practitioner and well tolerated by the patient.
Keywords: low back pain, trigger points, myofascial pain syndrome, ischemic compression, chiropractic.
From the FULL TEXT Article:
Introduction
Low back pain is the most common and costly neuromusculoskeletal (NMS) dysfunction in contemporary society, [1] and the most common reason for a patient to present to a chiropractor’s office. [2, 3] Over 80% of adults suffer from spinal pain at some time in their lives, affecting both a person’s physical abilities as well as their psychosocial health. [4, 5] Within health care circles, a number of different approaches are used to manage patients so afflicted, with variable results. Therapeutic approaches used to manage low back pain include: non prescription analgesics; prescribed pharmaceuticals; electrical modalities; acupuncture; shoe lifts; low back corsets and back belts; patient education and; manual procedures including soft tissue therapy, mobilizations, and spinal manipulative therapy. [6, 7] Although joint dysfunction, disc disease, degenerative arthritides, sprains, strains and other disorders associated with the position or movement of the spine (such as those caused by scoliosis or spondylolisthesis) are all recognized common causes of low back pain, [8] the role of muscular disorders are often under appreciated. However, some experts, such as Simons and Travel9 maintain that myofascial irritations are very common causes of low back pain, eminently treatable by a skilled practitioner, and should therefore be considered in all chronic pain patients.
In addition to a brief review of the literature, the author draws on his own clinical experience in order to describe an approach to identify, localize and treat low back pain of myofascial origin using ischemic compression technique.
Literature search
Using a standard search strategy, the author sought to identify articles describing the treatment of low back pain of myofascial origin using ischemic compression. Key words used for the search of health care databases (Pubmed, Mantis, Medline, CINAHL) were: low back pain/ myofascial pain syndrome/ ischemic compression/ and chiropractic.
Surprisingly few articles were found using this search strategy. Several articles from the late 1980s and early 1990s reported that trigger point therapy would be useful for patients with low back pain originating from myofascial structures, sacroiliac dysfunction, disc herniation, or cases of assumed neurologic involvement as evidenced by a positive straight leg length test. [10–14]
Two more recent articles were case reports of the treatment of the quadratus lumborum (QL) muscle associated with low back pain. [15, 16] In one article, DeFranca and Levine [15] describe the successful resolution of two patients suffering from low back pain, flank pain, buttock and lateral hip pain using myofascial therapy aimed at restoring QL muscle length and function, coupled with spinal manipulative therapy as indicated. The other article by Bryner [16] describes five cases of unilateral flank pain and local tenderness attributed to involvement of the quadratus lumborum muscle. Chiropractic treatment consisted of soft tissue therapies and spinal manipulation. In all five cases, patients reported significant improvement within the first few days of treatment, although two patients required 4 to 6 weeks of treatment in order to experience sustained pain relief and return to normal function. [16] These reports are congruent with the current literature that suggests the QL is the most important stabilizer of the low back. [17, 18]
In addition to ischemic compression, (see also [19]) other modalities have been successfully applied to elicited trigger points in order to diminish myofascial pain syndromes. Ultrasound and transcutaneous electrical nerve stimulation (TENS) have reportedly been used to successfully manage patients with low back pain of myofascial origin and for fibromyalgia. [20–22] Furthermore, several studies have reported clinically important results using more invasive procedures such as injection or acupuncture needling of trigger points. [20, 23–26]
Kovacs and his colleagues [8] recently revealed their results of a randomized, double-blinded controlled multicenter clinical trial assessing the efficacy of neuroreflexotherapy in the management of low back pain. In this study, Kovacs et al. assigned patients with chronic low back pain into either a control group (n = 37) or treatment group (n = 41). The treatment group intervention was characterized by temporary implantation of epidermal devices in trigger points in the low back at the sites of dermatomes clinically involved in each case, as well as referred tender points of the ear. The control group received a sham treatment consisting of placement of the same number of epidermal devices to within a 5 cm radius of the target zone. Patients were allowed to continue with their pain medication, the use of which was monitored during the trial. Evaluations were performed five minutes before the intervention, five minutes immediately after the intervention, and 45 days later. Patients in the treatment group showed immediate lessening of pain compared to patients in the control group. The pain relief was clinically relevant and statistically significant. [8]
In addition to low back pain, the author of this article has recently found ischemic compression techniques to also be effective in the treatment of fibromyalgia, [27] shoulder pain [28] and gastroesophageal reflux disease. [29]
Clinical presentation
In a recent article, Schneider [30] wrote that tender spots (TSs) differ from trigger points (TPs) in that TSs are defined as discrete areas of soft tissue that are painful to about 4 kg of digital pressure. By contrast, TPs are defined as hyperirritable spots located within the taut band of skeletal muscle that are painful to compression and give rise to characteristic referred pain patterns and autonomic symptoms. [26, 30] Both tender spots and trigger points may simultaneously exist in muscle, tendon, ligament, fascia or fibrous articular capsules.
Trigger points often give rise to characteristic pattern of referred pain distant from the point of contact. [31] The pain elicited is diffuse and radiates to an area representing the symptomatic site. [31] In almost all cases, digital pressure on the painful point will reproduce the symptoms of the chief complaint, or even worsen the level of reported pain. Inactivation of either TPs or TSs, however, may eradicate the patient’s pain. WhenTPs and TSs are localized in a palpable group of contracted muscle fibers, they may feel like a hypersensitive band. That group of fibers is called a taut band. [26]
In chiropractic, the most common method of treating these tension points is the use of sustained thumb pressure, called ischemic compression (see below).
Possible biological mechanisms
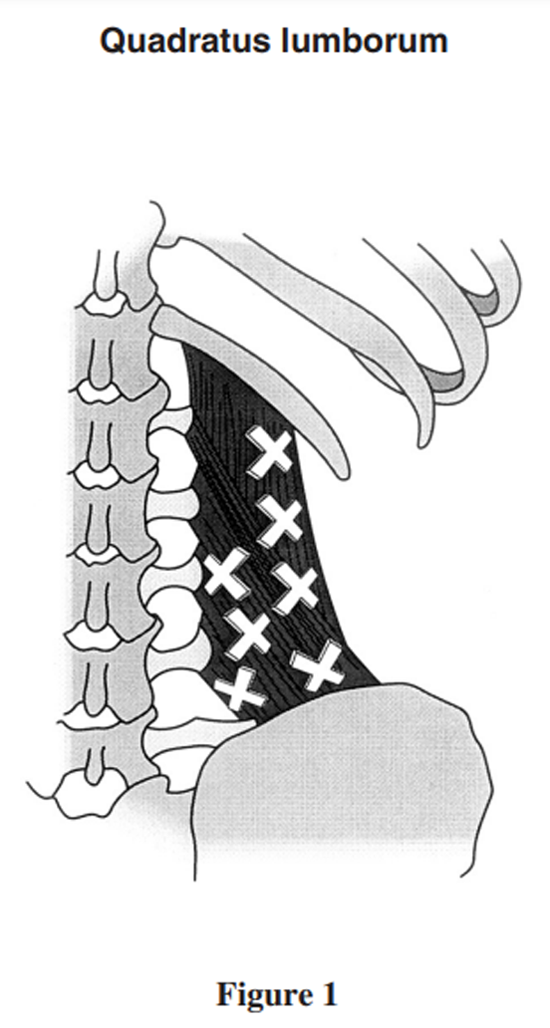
Figure 1
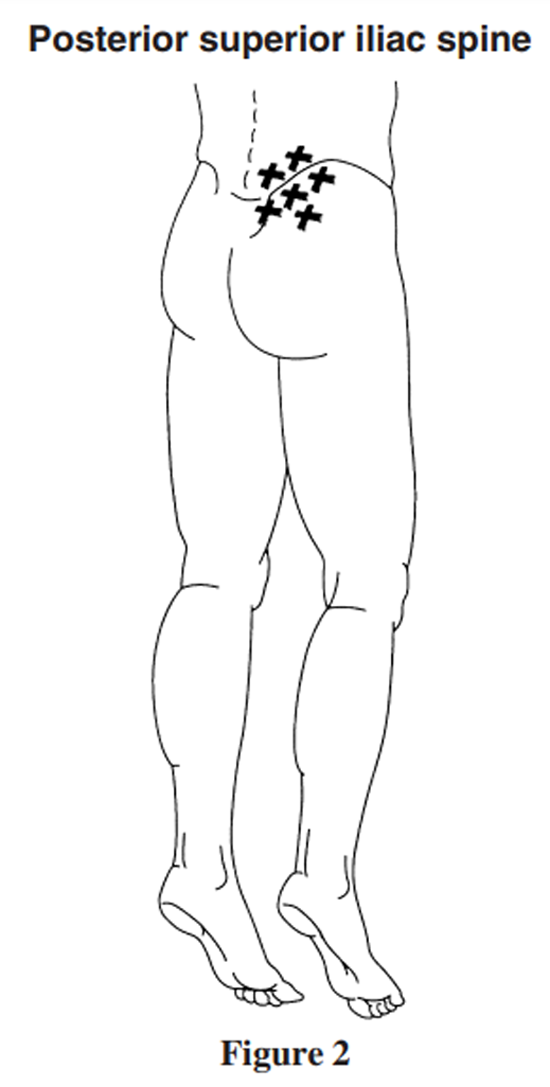
Figure 2
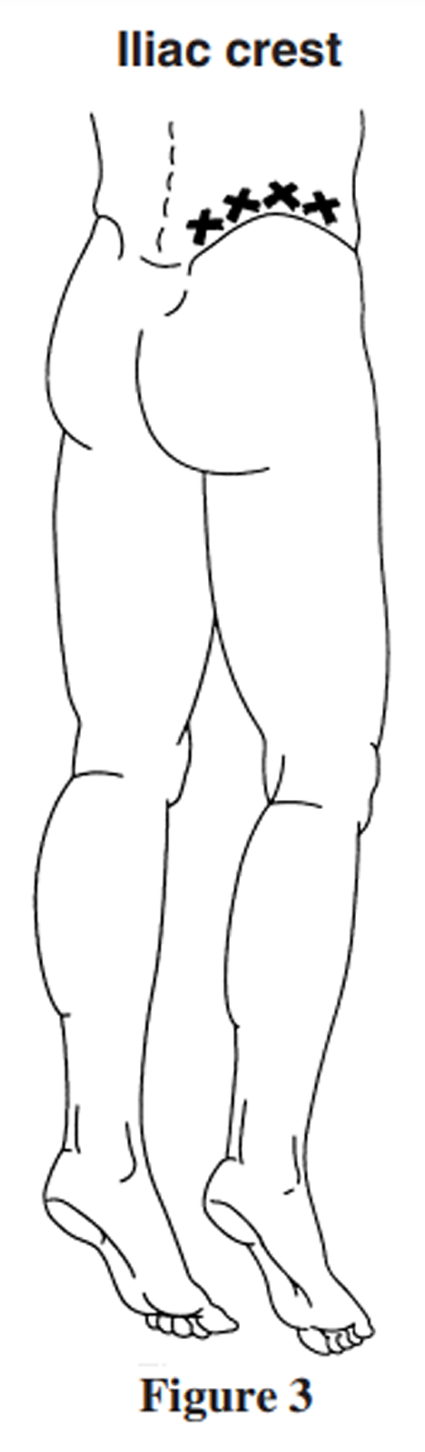
Figure 3
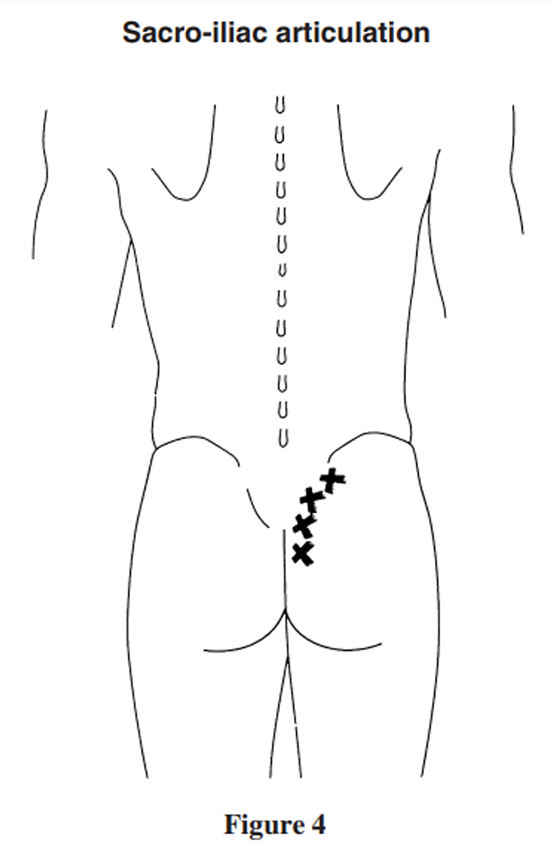
Figure 4
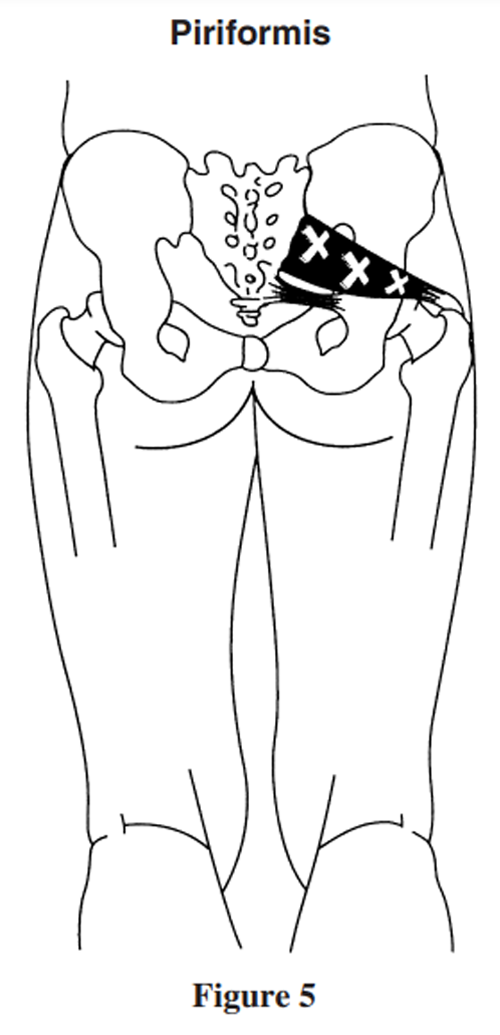
Figure 5
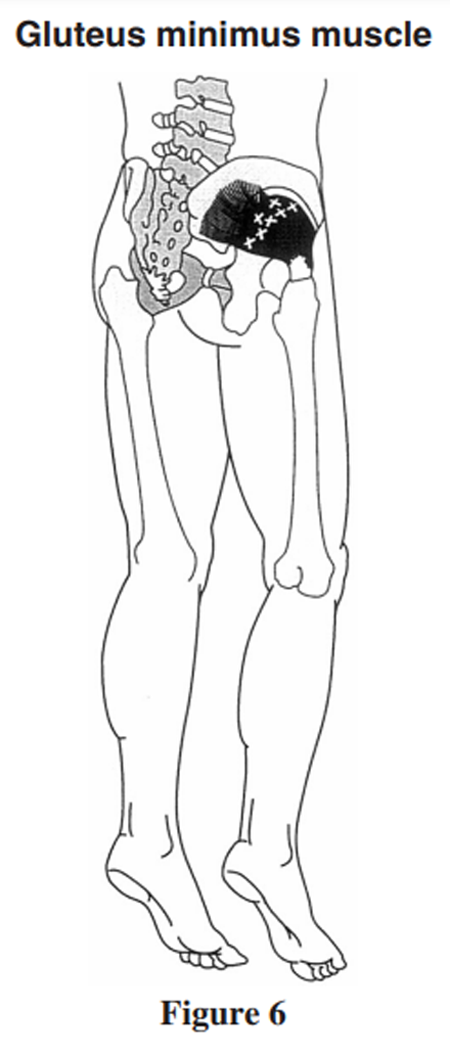
Figure 6
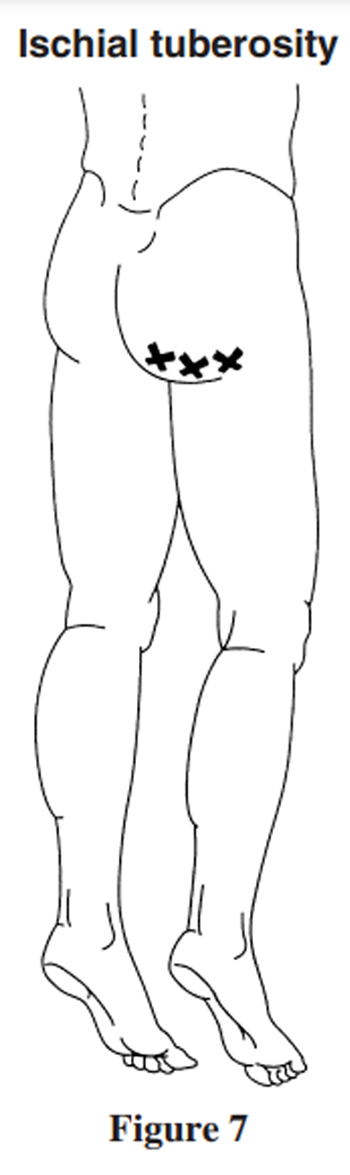
Figure 7
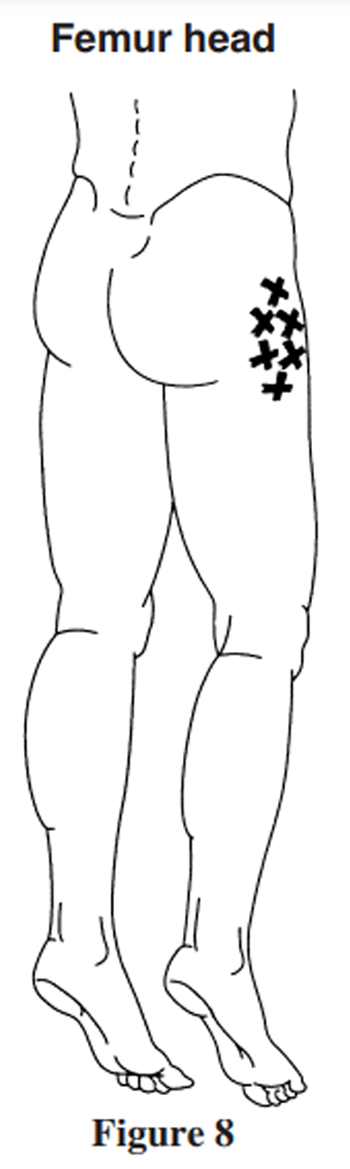
Figure 8
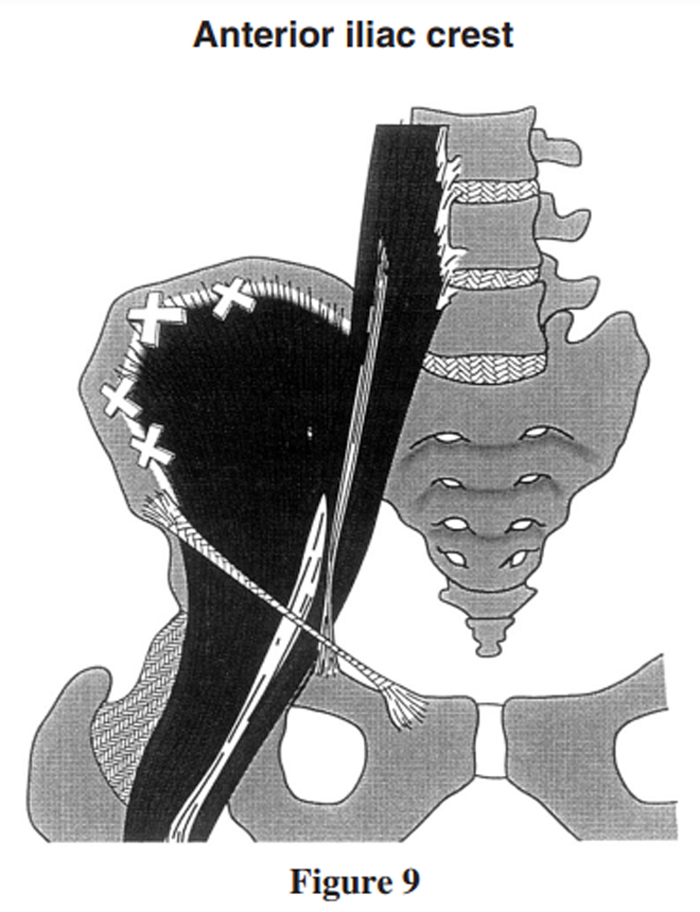
Figure 9 Many historians credit Nimmo with being the first chiropractor to make what was, for its time, a radical conceptual leap from a treatment model advocating ‘moving bones’ to one that addressed the muscles that move the bones. [33] Nimmo, a pioneer in the area of soft tissue techniques, theorized that hypersensitive areas, equivalent to the trigger points described by Travel, were abnormal neurological reflex arcs. [32] According to Gatterman and Lee [34] Nimmo referred to the inter-relationship of muscle tonus and the central nervous system as ‘reverberating circuits’, whereby the stimulus was self-perpetuating until the cycle was broken. Nimmo posited that what he referred to as hypermyotonia may result from trauma, exposure to cold drafts, or from occupations requiring an individual to maintain a prolonged period of postural strain such as typing or driving an automobile. [33] The net effect of this increased sensory input to the spinal cord resulted in increased streams of efferent impulses to muscles, resulting in a constant state of abnormal contraction. In turn, this abnormal contraction led to a further increase in aberrant sensory input and still more muscle contraction. This process was thought to occur in the sympathetic nervous system, and was thus beyond voluntary control. However, unlike Travel and Simons who advocated injections to trigger points, spray and stretch techniques and ischemic compression, Nimmo did not address the trigger point directly, instead suggesting that the sequential application of pressure to affected muscles would cause the nervous system to ‘release a hypertonic muscle’. [33]
Kovacs and his colleagues suggest that there is evidence to support the theory that physical stimulation of dermal nerve endings related to involved dermatomes could release enkephalins that, in turn, bind to the receptors of capaicin-sensitive fibers thus preventing the release of substance P. [8] This deactivates nociceptive neurons and inhibits the mechanism involved in the pathophysiology of low back pain. Moreover, these researchers suggest that structures in the thalamus and brainstem activated by stimuli applied far from the painful zone are capable of triggering pain-relieving effects. [8]
Management approach
Favouring as they do techniques that are low-tech, noninvasive and hands-on, chiropractors typically use cryotherapy, mobilization, manipulation and soft tissue techniques for the management of disorders of the spine and peripheral joints. [2, 3] Among the most popular method of treatment of myofascial pain syndromes is ischemic compression. This approach, also known as Pennel’s technique, Nimmo technique, trigger point therapy or acupressure has been used by chiropractors and other manual therapists for at least 40 years. [2] According to the 2000 Job Analysis of the National Board of Chiropractic Examiners, over 90% of chiropractors use trigger point therapy for passive adjustive care, 68% use acupressure, and 40% report using NIMMO or Receptor tonus technique. [2] It should also be mentioned chiropractors often provide patient education, lifestyle modifications and ergonometric suggestions to augment the care administered in the office. [2]
Locating trigger points
As suggested by Travel and Simons, [31] a practitioner locates trigger points by using the tip of his or her thumb to exert a pressure of about 4 kg on the muscles and tendons of the low back. Several experts have developed different strategies to help a practitioner identify the trigger points and tender spots most associated with low back pain. Simons [9] locates these trigger points by relying on the characteristic manner in which elicited pain is distributed throughout the low back. The author of this article goes further, suggesting a practitioner examine the entire symptomatic region of the patient’s low back, trying to identify TPs, TSs and taut bands. With regard to the low back, the author applies thumb-tip pressure to each square inch of the lumbar spine and hip area (with the obvious exception of the genital area). The author also investigates the femoral trochanters, sacrum and sacroiliac joints. This examination is conducted during the initial examination and elicited TGs and TSs are appropriately recorded in the patient’s health history file.
Since various muscles overlap, the author also relies on specific skeletal reference points that are well known and easily located. If necessary, specific muscle tests can be performed to better differentiate between overlapping muscles. A description of a method to locate and identify the most common sites of trigger points and tender spots associated with low back pain is described below.
Sites examined
The quatratus lumborum (see Figure 1). Although the QL muscle is a common cause of low back pain, it is often overlooked by practitioners. The patient is placed in the prone position. The practitioner may raise the patient’s pelvis by 2 to 6 cm (on the side of examination) using a knee or pelvic wedge and palpates the entire QL muscle from the inferior aspect of the 12th rib to the ipsilateral iliac crest.
The posterior superior iliac spine (PSIS). Trigger points are often located in close proximity to this structure, and within a 2 cm radius of it. The author has observed that most patients suffering from low back have trigger points at this site (Figure 2).
The iliac crest (see Figure 3). This structure is palpated moving from posterior to anterior.
The wider aspect of the posterior sacroiliac line (see Figure 4).
The piriformis area (see Figure 5). The trigger point of this muscle can be found 3 cm lateral from the second sacral tubercle. Alternatively, an imaginary line can be drawn from the PSIS to the greater trochanter of the femur. The trigger point of the piriformis can often be located by contacting a point 1 to 2 cm below the midway point of this line. Performing a Hibb’s maneuver can further isolate the piriformis muscle. To perform this test, the patient is placed in the prone position. The examiner bends the patient’s leg to 909 and the thigh is internally rotated by externally rotating the leg. [34] Thus, while the examiner is performing this maneuver he or she palpates the length of the piriformis from the greater trochanter to the mid-sacral region. The author has found it is easier to treat the piriformis muscle when the patient’s pelvis is raised about 4 cm by either the practitioner’s knee or using a pelvic block. Due to the anatomical proximity of the sciatic nerve, this area should be examined whenever a patient reports sciatic. It is not uncommon for piriformis hypertonicity to mimic sciatica of discal origin. [9, 31]
The gluteus minimus (Figure 6). Examination and treatment of this muscle is performed by positioning the patient on his or her side. The examiner may stand either in front of or behind the patient. In cases involving the gluteus minimus muscle, the patient often reports of pain in the outer aspect of the thigh.
The ischium (Figure 7), femoral trochanters (Figure 8) and anterior iliac crest (Figure 9), although less commonly involved, should each be individually examined as well.
Different muscles may overlap. To better differentiate between one muscle and another, the suspected muscle can be tested for its strength. For example, although the piriformis muscle and gluteus minimus muscle may both exhibit trigger points in close proximity to each other, the former is an external rotator of the leg, whereas the latter is an abductor and weak extensor of the pelvis. [36]
Treatment
Once TPs and TSs are identified, the author applies ischemic compression for between 5 and 15 seconds, depending on patient tolerance. In the author’s clinical experience, it is useful to sustain pressure for a longer period of time on those trigger points found to be more sensitive to digital pressure. However, the author has also found that the more trigger points the patient elicits, the less time each one should be treated. Again, this is monitored by closely observing the patient’s tolerance to the pain. Each elicited TP or TS is treated during the course of the patient’s visit. The intensity of digital pressure by the physician should induce local or referred pain that does not cause the patient to attempt to break the contact or protect the muscle being treated by contracting it. The treatment has to be painful but bearable. It is the author’s experience that only the symptomatic side should be treated, and this general principle has been followed by other practitioners.(see [16, 17])
Treatments are provided to the patient until such time as the identified TPs and TSs no longer elicit local or referred pain. [27] This may require anywhere from 5 to 30 treatment sessions. [27] The patient can be given a home-care stretching and strengthening program to further enhance recovery. [19] There are no contraindications to this treatment approach, and the only significant adverse effects reported by patients is soreness or stiffness and, more rarely, some minor bruising in the area being treated. In these cases, the examiner can use less pressure on each TP or TS during subsequent treatments.
Summary
Myofascial pain syndromes should be considered in all patients reporting low back pain. Chiropractors should carefully assess the lumbar spine, as well as the gluteal, femoral and pelvic regions, attempting to elicit those TPs and TSs that reproduce the patient’s chief complaint. Even in cases involving other causes of low back pain (joint dysfunction, discal disease and so on), the practitioner may augment the patient’s recovery by addressing involved soft tissues. Ischemic compression is a safe and effective method to successfully treat elicited trigger points or tender spots. This method does not require specialized equipment, it is well tolerated by the patient, and is not physically strenuous on the doctor. Although there exists some evidence to support this clinical approach, randomized controlled double-blinded studies or carefully monitored practice-based clinical trials should be conducted in order to better substantiate the effectiveness of this approach observed in private practice.
Acknowledgement
The author would like to thank Dr Brian Gleberzon D.C. for his assistance in preparing this manuscript.
References:
Vernon H, Cote P, Beauchemin D et al.
International conference on spinal manipulation, 1990
FCER, 1701 Clarendon Bouldvard, Arlington, Virginia.Christensen MG.
Job Analysis of Chiropractic 2000
National Board of Chiropractic Examiners. Greeley, Co.Meeker, W., & Haldeman, S. (2002).
Chiropractic: A Profession at the Crossroads of
Mainstream and Alternative Medicine
Annals of Internal Medicine 2002 (Feb 5); 136 (3): 216–227Vernon H.
Spinal manipulation for chronic low back pain:
a review of the evidence.
Top Clin Chirop 1999; 6(2):8–12.Hoffman B.
Confronting psychosocial issues in patients with low back pain.
Top Clin Chirop 1999; 6(2):1–7.Cooperstein R, Perle SM, Gatterman MI, Lantz C, Schneider MJ.
Chiropractic technique procedures for specific low back conditions:
Characterizing the literature.
J Manipulative Physiol Ther 2001; 24(6):407–424.Hawk C, Long CR, Boulanger KT, Morschhauser E, Fuhr A.
Chiropractic care for patients aged 55 years and older:
Report from a practice-based program.
J Am Geriatr Soc 2000; 48:534–545.Kovacs FM, Abraira V, Pozo F et al.
Local and remote sustained trigger point therapy for exacerbations
of chronic low back pain. A randomized, double-blinded,
controlled, multicenter trial.
Spine 1997; 22(7):786–797.Simons DG, Travel JG.
Myofascial origins of low back pain.
Principles of diagnosis and treatment.
Post graduate medicine 1983; 73:66–77.Immamura ST, Fisher AA, Immamura M.
Pain management using myofascial approach when other treatment failed.
Phys Med Rehab Clin North America 1997; 8:179–97.Garvey TA, Marks MR, Wiesel SW.
A prospective randomized double-blind evaluation of
trigger-points injection therapy for low back pain.
Spine 1989; 14:962–964.Cassissi JE, Sypert GW, Lagana L et al.
Pain, disability and psychological functioning in chronic low back
pain subgroups: myofascial versus herniated disc syndrome.
Neurosurgery 1993; 33:379–385.Shaw LJ.
The role of the sacroiliac joint as a cause of low back pain and dysfunction.
Presented at the World Congress on Low Back Pain,
University of California, San Diego, CA. Nov 5–6,1992.Sandman KB.
Myofascial pain syndrome: the mechanism, diagnosis and treatment.
J Manipulative Physiol Ther 1981; 4:135–140.Defranca GG, Levine LJ.
The quatratus lumborum and low back pain.
J Manipulative Physiol Ther 1991; 14(2):142–149.Bryner PB.
Unilateral back pain: a case series of quadratus lumborum involvement.
Chiropractic Tech 1996; 8(2):70–77.McGill S.
Low back exercise: evidence for improving exercise regiments.
Phys Ther 1998; 78:754–765.Byfield D.
Spinal rehabilitation and stabilization for the
geriatric patient with back pain.
In: Chiropractic Care of the Older Patient (Gleberzon BJ editor).
ButterworthHeineman, Oxford, UK. 2001; 407–440.Hanten WP, Olsen SL, Butts NL, Nowicki AL.
Effectiveness of a home program of ischemic pressure followed
by sustained stretch for treatment of myofascial trigger points.
Phys Ther 2000; 80(10):997–1003.Alvarez DJ, Rockwell PG.
Trigger points: diagnosis and management.
Am Fam Physician 2002; 65(4):653–660.Esenyel M, Caglar N, Aldemir T.
Treatment of myofascial pain.
Am J Phys Med Rehabil 2000; 79(1):48–52.Han SC, Harrison P.
Myofascial pain syndrome and trigger-point management.
Reg Anesth 1997; 22(1):89–101.Hong CZ, Hsueh TC.
Difference in pain relief after trigger point injection in
myofascial pain patients with and without fibromyalgia.
Arch Phys Med Rehabil 1996; 77(11):1161–1166.Van Tulder MW, Cherkin DC, Berman B, Lao L, Koes BW.
The effectiveness of acupuncture in the management of acute and chronic
low back pain. A systematic review within the framework of
the Cochrane Collaboration Back Review Group.
Spine 1999; 24(11):1113–1123.Cummings TM, White AR.
Needling therapies in the management of myofascial
trigger point pain: a systematic review.
Arch Phys Med Rehabil 2001; 82(7):986–992.Borg-Stein J, Stein J.
Trigger points and tender points: one and the same?
Does injection treatment help?
Rheum Dis Clin North Am 1996; 2292:305–322.Hains G, Hains F.
Combined ischemic compression and spinal manipulation in the treatment
of fibromyalgia: A preliminary estimate of dose and efficacy.
J Manipulative Physiol Ther 2000; 23:225–230.Hains G, Hains F, Descarreaux M.
Gastroesophageal Reflux Disease, Spinal Manipulative Therapy and
Ischemic Compression: A Preliminary Study
J Am Chiropr Assoc. 2007;44(1):7–19.Hains G.
Chiropractic Management of Shoulder Pain and Dysfunction of
Myofascial Origin Using Ischemic Compression Techniques
J Can Chiropr Assoc 2002; 46 (3): 192–200Schneider M.
Tender points/ fibromyalgia vs. trigger points/ myofascial pain syndromes.
A need for clarity in terminology and differential diagnosis.
J Manipulative Physiol Ther 1995; 18:398–406.Travel JG, Simons DG.
Myofascial pain and dysfunction. The Trigger Point Manual. Second Edition.
Williams and Wilkins, Baltimore. 1992Norregaard J, Jacobsen S, Kristensen JH.
A narrative review on classification of pain conditions of the upper extremity.
Scand J Rehab Med 1998; 31:153–164.Cohen JH, Gibbons RW,
Raymond L. Nimmo and the evolution of trigger point therapy, 1929-1986.
J Manipulative Physiol Ther 1998; 21(3):167–172.Gatterman M, Lee HK.
Chiropractic adjusting technique.
In: Chiropractic: An illustrated history (Ed: Peterson D, Weise G).
Chicago, Mosby; 1995:240–261.McGee DJ.
Orthopedic physical assessment. Third Ed.
WB Saunders Co. Philadelphia, PA. 1997; 441.Moore KL, Dalley AF.
Clinically oriented anatomy. 4th ed.
Lippincott, Williams and Wilkins. Baltimore, MA. 1999.
Return to LOW BACK PAIN
Return to MYOFASCIAL TRIGGER POINTS
Since 3-10-2023


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |