

Non-serious Adverse Events Do Not Influence
Recovery in Patients with Neck Pain
Treated with Manual Therapy;
An Observational StudyThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Musculoskelet Sci Pract 2022 (Oct); 61: 102607 ~ FULL TEXT
OPEN ACCESS Renske Peters, Emiel van Trijffel, Joost van Rosmalen, Bert Mutsaers, Annelies Pool-Goudzwaard, Arianne Verhagen, Bart Koes
SOMT University of Physiotherapy,
Amersfoort, the Netherlands;
Department of General Practice,
Erasmus Medical Centre,
Rotterdam, the Netherlands.
Highlights
Non-serious adverse events do not influence recovery in patients with neck pain.
Duration of neck pain does influence recovery in patients with neck pain.
The role of non-serious adverse events should be re-evaluated in a larger sample.
Keywords: Adverse events; Neck pain; Perceived recovery; Prognosis.
From the FULL TEXT Article:
Introduction
Up to 70% of individuals experience an episode of neck pain (NP) once in their life (Fejer et al., 2006). The course of NP is often episodic; evidence indicates that between 50 and 75% of people who experience NP at some initial point will still report NP 1–5 years later (Carroll et al., 2009). In a Dutch study, 47% of the patients in primary care reported to have ongoing NP (Vos et al., 2008). A recurrent course is common with almost 25% of patients reporting aggravation of NP after full recovery (Chaibi et al., 2021; C ô t é et al., 2004). Consequently, the estimated economic burden of NP is substantial (Hoy et al., 2014).
Physiotherapy, with or without manual therapy (MT) techniques, and chiropractic are common treatment options for patients with NP (Chaibi et al., 2021). Physiotherapy for NP is diverse and commonly used MT techniques include spinal manipulations, spinal mobilisations, exercise, and information and advice (Gross et al., 2015). Despite evidence to support the benefits of cervical manipulation and mobilisation (Gross et al., 2015), the use of these treatment modalities remains a matter of debate because of their potential risks of serious adverse events (SAEs), e.g. stroke, cervical artery dissection, transient ischemic attack. (Cagnie et al., 2004), (Ernst, 2007), (Rubinstein et al., 2007) However, the occurrence of SAEs seems rare (Kerry and Taylor, 2014; Chaibi and Russell, 2019). Besides these SAEs, several non-serious adverse events (NSAEs) e.g. aggravation of complaints, stiffness, irradiating pain are described. Other than SAEs, the NSAEs after MT are common, benign, and transient (Cagnie et al., 2004; Rubinstein et al., 2008). The incidence of minor or moderate transient adverse events after MT was estimated as 41% from cohort studies and 22% from randomised controlled trials (Carnes et al., 2010). Another study showed that half of patients experience minor to moderate adverse events after MT treatment, with most NSAEs being musculoskeletal or pain-related (Rubinstein et al., 2008). It is generally assumed that there is an under-reporting of cases with (N)SAEs (Carnes et al., 2010; Kranenburg et al., 2017).
Patient characteristics such as age, gender, fear avoidance, concomitant symptoms, previous musculoskeletal complaints, patient expectancies, poor general health, and smoking, as well as pain-related factors such as pain intensity, duration of pain, and recurrence of NP are known to influence recovery (Groeneweg et al., 2017; Artus et al., 2017; Bier, 2016; Walton et al., 2013; Carroll et al., 2008; Palml ö f et al., 2016). However, it is unknown whether NSAEs can influence recovery after multimodal treatment including MT in patients with NP. Therefore, our research question was: What is the influence of NSAEs, additional to other prognostic factors, on perceived recovery in patients with NP treated with usual multimodal care inclusive of MT?
Methods
A prospective multicentre cohort study with 12-month follow-up was conducted in primary care physiotherapy in the Netherlands of which the current study used the post-treatment follow-up data. The Medical Ethical Committee of the Erasmus MC Rotterdam approved this study. The design of the complete study was published elsewhere (Peters et al., 2019). The reporting of this study was guided by the STROBE statement (Von Elm et al., 2007).
Physiotherapists with postgraduate qualifications in MT
During a 3-month inclusion period, patients with NP were recruited by 263 participating physiotherapists with postgraduate qualifications in MT in The Netherlands. The physiotherapists provided usual care to their patients with NP. Although the definition of usual care has not been standardised, it includes the routine care received by patients for prevention or treatment of diseases (Harlapur et al., 2013). The type of routine care can vary by the grade of neck pain and severity, the practice in which patients present themselves, and individual therapists. Physiotherapy in our study is mostly provided in the context of a multimodal management program including information, advice, MT and exercise.
Patients
Patients with non-specific NP of any duration and aged between 18 and 80 years of age were eligible for inclusion in the study. Exclusion criteria were not being able to fluently read and write the Dutch language and having specific NP due to severe trauma, systemic disorders, or generalised neurologic syndromes. Patients reported on (N)SAEs within 48 h after every treatment session. All patients signed an informed consent prior to enrolment in the study.
Outcome measures
A literature search in the databases MEDLINE (PubMed), CINAHL, Embase, and PEDro was conducted to identify potentially relevant prognostic factors on outcomes of MT. Age (Walton et al., 2013; Feleus et al., 2007; Bruls et al., 2013; Bot et al., 2005; Keijsers et al., 2010), gender (Vos et al., 2008), pain intensity (Walton et al., 2013; Bot et al., 2005; Hoving et al., 2004), recurrent NP (Carroll et al., 2009), disability (Artus et al., 2017), duration of pain (Artus et al., 2017; Mallen et al., 2007), fear avoidance (Mallen et al., 2007), concomitant symptoms (Vos et al., 2008; Walton et al., 2013; Feleus et al., 2007; Bot et al., 2005; Keijsers et al., 2010; Leaver et al., 2013), patient expectancies (Bischop et al., 2013), smoking (Vineis, 2008), and sport participation (Hoving et al., 2004) were identified and measured at baseline. NP characteristics included intensity as measured by the Numeric Rating Scale (NRS, range 1–10) and patients’ self-reported recurrence and duration (<6 weeks; acute, >6 but <12 weeks; subacute, or >12 weeks; chronic NP). The Neck Disability Index (NDI) was used to measure disability due to NP (range 0–50) (Schellingerhout et al., 2012; Vernon, 2008). The Fear Avoidance Beliefs Questionnaire (FABQ subscale physical activities (FABQ-PA) range 0–30) (Landers et al., 2008; Cleland et al., 2008) was used to measure avoidance of physical activities due to fear of NP. Additionally, patients were asked to provide additional information on possible risk factors for (N)SAEs such as comorbidities (e.g., hypertension, (history of) heart failure, diabetes mellitus, hypercholesterolemia, atherosclerosis, migraine). (Paanalahti et al., 2014), (Haldeman et al., 1999), (Haldeman et al., 2002)
During the treatment period, patients reported on (N)SAEs using the Adverse Events Questionnaire (AEQ), which was filled out by the patient within 48 h after each treatment. The AEQ has been used before (Cagnie et al., 2004; Rubinstein et al., 2007; Hurwitz et al., 2005) and consists of several questions on possible reactions potentially occurring after treatment. The AEQ measures if the patient experienced any unpleasant reaction after treatment, and, additionally, the type of reaction, time of onset (range 1–4), duration (range 1–4), and intensity of symptoms (range 1–10) (See Appendix 1). In order to grade NSAEs, we decided that the occurrence of uncommon NSAEs such as cramps, dizziness, blurred vision, nausea, tinnitus, vomiting, dizziness, and weakness of the limbs are undesirable and their occurrence (intensity >1 on the 10-point NRS) was defined as NSAEs. For common NSAEs like headache, stiffness, aggravation of complaints, radiating pain, and fatigue, the intensity should be > 5 on the 10-point NRS and the duration longer than 24 h to be defined as a NSAE. All other reactions of lesser intensity and duration were defined as ‘absence of an (N)SAE’. (N)SAEs were registered throughout the treatment episode and dichotomised as ‘present’ or ‘absent’, regardless the number of adverse events, the number of treatment sessions, or the treatment modality applied.
At the end of the treatment episode, the primary outcome, patients' self-rated recovery, was assessed using the Global Perceived Effect (GPE) scale. The GPE is scored on a 7-point Likert scale ranging from ‘total recovery’ to ‘worse than ever’. A priori, recovery was defined as ‘total recovery’, ‘much improved’ or ‘somewhat better’ as reported by the patient. Being a single question, GPE is easy and quick to administer and the results are seemingly simple to interpret. Test-retest reliability of the GPE is excellent (Kamper et al., 2010). After collecting the data, treatments were categorised into manipulation, mobilisation, manipulation and mobilisation or ‘other treatment modalities’, including information/advice and exercise. The distribution of applied modalities and their reported (N)SAEs are shown in Appendix 2.
Data analysis
Differences in gender were tested using the chi-square test, and differences in age between patients who filled out and those who did not fill out the GPE did not have normal distribution and were therefore tested using Mann-Whitney U tests. Univariable and multivariable logistic regression analyses were performed to estimate the relationship between potential prognostic factors and perceived recovery, measured by the GPE. The independent variables in these models were selected from NSAEs, gender, age, initial pain, recurrent NP, duration of NP, concomitant complaints, expectancies with regard to recovery, disability, fear avoidance, smoking, and sport participation. All independent variables with P values < 0.2 in univariable analysis were included in the subsequent multivariable logistic regression analysis. The independent variables were checked for correlation to prevent multicollinearity. In case of high correlation, one of the two variables was selected based on lower correlation with other independent variables. Univariable associations between independent variables and the outcome were expressed as odds ratios (OR) with their 95% confidence intervals (CI).
Subsequently, multivariable logistic regression analysis was applied to test prognostic variables for perceived recovery measured by GPE immediately after the multimodal treatment episode. To account for missing values in the data, multiple imputation using fully conditional specification was applied (25 iterations). Based on the evidence (Carroll et al., 2009; Artus et al., 2017; Walton et al., 2013) gender, age, and initial pain were forced as independent variables into the analysis. To estimate the added prognostic value of AE on GPE (additional to the other independent variables), two separate logistic regression models were constructed; one model without NSAEs and one with NSAEs included. The explained variance was calculated using Nagelkerke's R2. The Hosmer-Lemeshow test was performed to assess how well the model fits the data (Hosmer and Lemeshow, 2010). Associations between independent variables and the outcome were expressed as odds ratios (OR) with their 95% confidence intervals (CI). The dichotomous dependent variable ‘GPE’ was coded as ‘1’ (no recovery) and ‘0’ (recovery). To prevent overfitting, the total number of variables included in this model was limited to eight variables according to the one-in-ten-rule (Steyerberg et al., 2000). The significance level was set at α = 0.05. Data were analysed using the IBM SPSS 24 software package.
Results
Study flow and baseline measurements
Two hundred and sixty-three physiotherapists with postgraduate qualifications in MT participated in the study and enrolled patients during the recruitment period. The majority of the physiotherapists were male (79%), aged ≥40 years, with a mean of 20 years of clinical working experience.
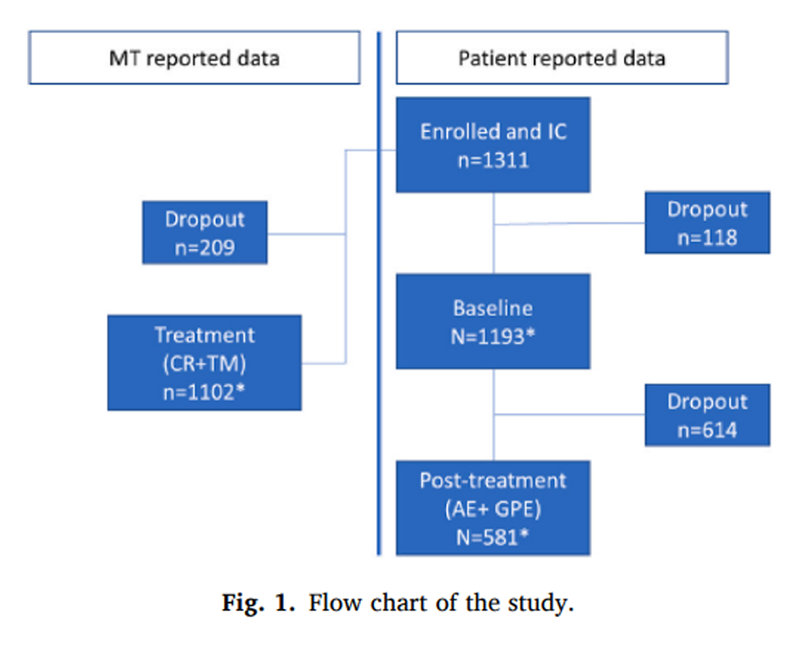
Figure 1

Table 1

Table 2 During the recruitment period, 1,311 patients were eligible and 1,193 patients with NP provided baseline measurements (Figure 1). Mean age (SD) of the participating patients was 44.7 (13.7) years and 823 (69.4%) participants were female. Five hundred and thirteen (47.9%) patients had NP longer than 12 weeks and 755 (66.9%) had recurrent NP. Five hundred and eighty-one (48.6%) participants filled out the GPE post-treatment and 460 (79%) of patients reported to be recovered. Table 1 presents the baseline characteristics of the study sample. There was a significant difference in age between patients who filled out a GPE questionnaire (median age 47 years), and those who did not (42 years) (p < 0.001), but there was no significant difference (X2(df = 1) = 2.028, p = 0.166) in gender. In our sample, no SAE occurred. A number of 297 (51%) patients reported a NSAE during a treatment episode.
Missing value analysis showed that the percentage of missing values per variable ranged between 0 and 10.4%. Within the cases that filled out the GPE (n = 581), missings were completely at random (Little's MCAR, X2(df = 8) = 3.079, p = 0.929.
Univariable analyses
Univariable associations are shown in Table 2. The duration of NP at baseline (acute NP OR 0.39 (95% CI 0.19–0.81), p < 0.001 and subacute NP (OR 0.32 (95% CI 0.19–0.52), p = 0.012)), with chronic NP serving as a reference category, recurrent NP (OR 1.43 (95% CI 0.91–2.24), p = 0.117), fear avoidance (OR 1.03 (95% CI 1.00–1.03), p = 0.077), and patient expectancies (OR 3.78 (95% CI 0.53–27.08) (p = 0.186)) were associated with perceived recovery and were subsequently entered into the multivariable analysis.
Multivariable analyses
Seven independent variables (age, gender, pain intensity, duration of NP, recurrent NP, fear avoidance, patient expectancies) were entered into the multivariable model. The full model containing all variables was statistically significant (p < 0.001). The model as a whole explained 9.5% (Nagelkerke R2) of the variance in recovery and correctly classified 81.5% of patients. The Hosmer-Lemeshow test indicated that the model adequately fitted the data (p > 0.05). ORs and CI are presented in Table 2. Duration of NP at baseline made an independent statistically significant contribution to the model, recording an OR of 0.39 (95% CI 0.24–0.64) for acute NP as compared with chronic NP. For subacute NP, an OR of 0.46 (95% CI 0.23–0.95) was found. The values of these odds ratios suggest that the longer a patient suffers from neck pain, the less likely it is that a patient recovers. No other variables were found to be significantly associated with recovery in this model and therefore our next analysis contained age, gender, pain intensity, and duration of NP as independent variables. This model was statistically significant (p < 0.001), with an explained variance in the reporting of recovery of 7.3% (Nagelkerke R2). The Hosmer-Lemeshow test showed goodness of fit (p > 0.05). ORs and confidence intervals are presented in Table 2.
Adding NSAE to the independent variables showed that NSAE did not significantly contribute to the model, with p = 0.351 and an OR of 1.24 (95% CI 0.79–1.94) (Table 2). Acute NP at baseline made an independent statistically significant contribution to the model with an OR of 0.40 (95% CI 0.26–0.64). For subacute NP an OR of 0.45 (95% CI 0.22–0.90) was found.
Discussion
Main findings
We found that the occurrence of an AE during a multimodal treatment episode including MT did not influence patients' perceived recovery. Only duration of NP at baseline had prognostic value to predict recovery, whereas the remaining prognostic factors did not contribute to the model. The significant influence of duration of NP on outcome is in accordance with existing evidence; patients suffering from NP less than six weeks have better chance of recovery than patients with chronic NP (Hush et al., 2011). Adverse events do not seem to be uniquely assigned to MT. Recent studies by Paanalahti et al. and Tabell et al. showed that NSAE are commonly reported in the treatment of NP, regardless whether the intervention consisted of manipulation or other modalities. This underlines the hypothesis that the occurrence of NSAEs may be associated with patients’ characteristics and less with treatment characteristics (Tabell et al., 2019; Paanalahti et al., 2014b). A systematic review by Carnes et al. also suggests that risk is inherent in all health interventions and should be weighed against patient-perceived benefit and alternative available treatments (Carnes et al., 2010).
Considering the transient and benign effects of NSAEs one could ask if the patients' benefits of adding MT to a multimodal treatment outweigh the possible discomfort of an NSAEs after treatment. Evidence from chiropractic and physiotherapeutic research on this topic is contradictory. One chiropractic study reported frequent NSAEs with none of the subjects reporting to be ‘worse’ or ‘much worse’ at the end of the study episode (Ernst, 2007). Therefore, these adverse events should in no way be misconstrued as a measure or indication of harm or be confused with (the lack of) perceived recovery. Another chiropractic study, however, showed that self-reported benign adverse events after chiropractic care for NP were associated with worse short-term outcomes (Rubinstein et al., 2008). Intense adverse events after chiropractic treatment were associated with more neck disability and clinically relevant differences at the short-term. However, there was no association between adverse events and worse outcomes at 3 months. In another chiropractic study, subjects reporting adverse reactions were less satisfied with care and less likely to have clinically meaningful improvements in pain and disability at 6, 13, and 26 weeks (Hurwitz et al., 2004). A point of discussion with regard to the conclusion of this study are the relatively small estimates and wide confidence intervals, which might also be consistent with no effect of adverse reactions on clinical outcome.
With regard to the independent variables, only about 7.7% of the total variance could be explained by our model. Although the choice of independent variables was largely in accordance with previous reports on significant predictors of outcome, the set of variables used in the present study might not have been the most relevant. It is striking that only one of the predictors identified in our study or previous studies, consistently showed an impact on GPE. Future studies should consider including other variables such as coping, illness beliefs, socio-economic factors, and lifestyle. Evidence suggests that patients’ self-reported measures are stronger predictors of outcome than physical signs, therefore no physical signs were included in this study (Walton et al., 2013; De Pauw et al., 2015). Nevertheless, these physical signs might have contributed to the variance in outcome and should therefore be considered for further research.
Limitations
Although our results suggest that the occurrence of an adverse event (AE) during a multimodal treatment episode including MT does not influence patients’ perceived recovery, this conclusion may be too simplistic. Currently, the one-in-ten rule (10 events per predictor parameter (EPP)) has generated much debate. Some authors claim that the EPP can sometimes be lowered below 10 (Vittinghoff and McCulloch, 2007). In contrast, others recommend at least 15 EPP, (Harrell, 2015) and others identify situations where at least 20 EPP or up to 50 EPP are required (Ogundimu et al., 2016; Austin and Steyerberg, 2017; Wynants et al., 2015; Van der Ploeg et al., 2014). However, a concern is that any blanket rule of thumb is too simplistic, and that the number of participants required will depend on many intricate aspects, including the magnitude of predictor effects, the overall outcome risk, the distribution of predictors, and the number of events for each category of categorical predictors (Ogundimu et al., 2016). Keeping in mind these above-mentioned criticism on the one-in-ten rule, we cannot exclude the possibility that our study was underpowered. The occurrence of NSAEs could have contributed to poor recovery but we may not have been able to demonstrate this because of the limited number of non-recovery events. Validating the results of this study in a larger sample size (with more events) and taking the intricate aspects into account, will give a better outline of the influence of NSAE on outcome.
Information on independent and dependent variables is generally captured through self-report, and this method is prone to recall or social desirability bias. On the other hand, while measurement error in the independent variables is prone to make a model unstable, in our study the 95% CIs of the ORs are rather narrow which indicates that estimates are quite precise and the influence of this error in our study is limited.
Unfortunately, only 581 (48.6%) of participants from the total study population returned the post-treatment booklets to the research centre. The booklets included AE questionnaires as well as GPE. We applied multiple imputation techniques to the independent variables, but we chose not to impute the dependent variable GPE. To get unbiased estimates in the regression analysis, it is essential to use the dependent variable to impute values for missing data on the predictor variables but imputing the GPE-scores might lead to bias (Schafer, 1997). However, the decision not to impute GPE led to significantly less data for the analysis, leading to a possibly underpowered study.
Conclusion
We found that the occurrence of non-serious adverse events (NSAEs e.g. aggravation of complaints, stiffness, irradiating pain) did not influence recovery in patients with neck pain treated by physiotherapists with postgraduate qualifications in manual therapy (MT). Currently, there is no need for physiotherapists to consider NSAEs when making prognosis in these patients. But, keeping in mind the criticism on the one-in-ten rule, we cannot exclude the possibility that our study was underpowered.
Appendix A. Supplementary data
Multimedia Component 1 Word document (140KB)
Multimedia Component 2 Word document (20KB)Ethics approval
The Medical Ethical Committee of the Erasmus Medical Centre Rotterdam approved this study. All participants gave written informed consent before data collection began.
Declaration of competing interest
None.
References:
Artus et al., 2017
M. Artus, P. Campbell, C.D. Mallen, et al.
Generic prognostic factors for musculoskeletal pain in primary care: a systematic review
BMJ Open, 7 (2017), Article e012901,
10.1136/bmjopen-2016-012901Austin and Steyerberg, 2017
P.C. Austin, E.W. Steyerberg
Events per variable (EPV) and the relative performance of different
strategies for estimating the out-of-sample validity of logistic regression models
Stat. Methods Med. Res., 26 (2) (2017), pp. 796-808Bier, 2016
J. Bier
Nekpijn. Dutch Guideline Koninklijk Nederlands Genootschap Fysiotherapie (2016)
KNGF-Richtlijn Retrieved from:
https://www.fysionet-evidencebased.nl/images/pdfs/richtlijnen/nekpijn_
2016/nekpijn_praktijkrichtlijn.pdfBischop et al., 2013
M.D. Bischop, P. Mintken, J.E. Bialosky, J.A. Cleland
Patient expectations of benefit from interventions for
NP and resulting influence on outcomes
J. Orthop. Sports Phys. Ther., 43 (7) (2013), pp. 457-465Bot et al., 2005
S.D.M. Bot, J.M. van der Waal, C.B. Terwee, van der Windt, et al.
Incidence and prevalence of complaints of the neck
and upper extremity in general practice
ARD (Ann. Rheum. Dis.), 64 (2005), pp. 118-123Bruls et al., 2013
V.E.J. Bruls, C.H.G. Bastiaenen, R.A. De Bie
Non-traumatic arm, neck and shoulder complaints: prevalence,
course and prognosis in a Dutch university population
BMC Muscoskel. Disord., 14 (2013), p. 8, 10.1186/1471-2474-14-8Côté et al., 2004
P. Côté, J.D. Cassidy, L.J. Carroll, et al.
The annual incidence and course of neck pain in the general population:
a population-based cohort study
Pain, 112 (2004), pp. 267-273Cagnie et al., 2004
Cagnie B, Vinck E, Beernaert A, et al.
How Common Are Side Effects of Spinal Manipulation
And Can These Side Effects Be Predicted?
Manual Therapy 2004 (Aug); 9 (3): 151–156Carnes et al., 2010
D. Carnes, T.S. Mars, B. Mullinger, R. Froud, M. Underwood
Adverse events and manual therapy: a systematic review
Man. Ther., 15 (4) (2010), pp. 355-363Carroll et al., 2008
Carroll LJ, Hogg-Johnson S, Cote P, van der Velde G, Holm LW, et al.
Course and Prognostic Factors for Neck Pain in Workers:
Results of the Bone and Joint Decade 2000–2010
Task Force on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S93–100Carroll et al., 2009
Carroll, LJ, Hogg-Johnson, S, van der Velde, G et al.
Course and Prognostic Factors for Neck Pain in the General Population:
Results of the Bone and Joint Decade 2000–2010 Task Force
on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S75–82Chaibi and Russell, 2019
Chaibi A, Russell MB.
A Risk-benefit Assessment Strategy to Exclude Cervical Artery
Dissection in Spinal Manual-therapy: A Comprehensive Review
Annals of Medicine 2019 (Mar 19): 51 (2): 118–127Chaibi et al., 2021
A. Chaibi, K. Stavem, M.B. Russell
Spinal Manipulative Therapy for Acute Neck Pain: A Systematic
Review and Meta-Analysis of Randomised Controlled Trials
J Clinical Medicine 2021 (Oct 28); 10 (21): 5011Cleland et al., 2008
J.A. Cleland, J.M. Fritz, J.D. Childs
Psychometric properties of the fear-avoidance beliefs questionnaire
and Tampa scale of kinesiophobia in patients with NP
Am. J. Phys. Med. Rehabil., 87 (2008), pp. 109-117De Pauw et al., 2015
R. De Pauw, J. Kregel, C. De Blaiser, et al.
Identifying prognostic factors predicting outcome in patients with
chronic neck pain after multimodal treatment: a retrospective study
Man. Ther., 20 (2015), pp. 592-597, 10.1016/j.math.2015.02.001Ernst, 2007
E. Ernst
Adverse effects after spinal manipulation
J. R. Soc. Med., 100 (2007), pp. 330-338Fejer et al., 2006
R. Fejer, K.O. Kyvik, J. Hartvigsen
The prevalence of neck pain in the world population:
a systematic critical review of the literature
Eur. Spine J., 15 (2006), pp. 834-848Feleus et al., 2007
A. Feleus, et al.
Prognostic indicators for non-recovery of non-traumatic complaints
at arm, neck and shoulder in general practice–6 months follow-up
Rheumatology, 46 (1) (2007), pp. 169-176, 10.1093/rheumatology/kel164Groeneweg et al., 2017
R. Groeneweg, T. haanstra, C.A. Bolman, R.A.B. Oostendorp, M.W. Van Tulder, R.W.J.G. Ostelo
Treatment success in neck pain: the added predictive value
of psychosocial variables in addition to clinical variables
Scand J Pain, 14 (2017 Jan), pp. 44-52, 10.1016/j.sjpain.2016.10.003 Epub 2016 Nov 2Gross et al., 2015
A. Gross, P. Langevin, S.J. Burnie, et al.
Manipulation and mobilisation for neck pain contrasted
against an inactive control or another active treatment
Cochrane Database Syst. Rev. (9) (2015), 10.1002/14651858.CD004249.pub4Haldeman et al., 1999
Haldeman S, Kohlbeck FJ, McGregor M.
Risk Factors and Precipitating Neck Movements Causing Vertebrobasilar
Artery Dissection After Cervical Trauma and Spinal Manipulation
Spine (Phila Pa 1976) 1999 (Apr 15); 24 (8): 785–794Haldeman et al., 2002
Haldeman S, Kohlbeck FJ, McGregor M.
Stroke, Cerebral Artery Dissection, and Cervical Spine Manipulation Therapy
J Neurology 2002 (Jul); 249 (8): 1098–1104Harlapur et al., 2013
M. Harlapur, D. Shimbo
Usual care
M.D. Gellman, J.R. Turner (Eds.),
Encyclopedia of Behavioral Medicine, Springer, New York, NY (2013),
10.1007/978-1-4419-1005-9_1297Harrell, 2015
F.E. Harrell Jr.
Regression Modeling Strategies: with Applications to Linear Models,
Logistic and Ordinal Regression, and Survival Analysis (second ed.),
Springer International Publishing, Cham, Switzerland (2015)Hosmer and Lemeshow, 2010
D.W. Hosmer, S. Lemeshow
Applied Logistic Regression (second ed.),
Wiley-Interscience, Hoboken, USA (2010)Hoving et al., 2004
J.L. Hoving, H.C.W. de Vet, J.W.R. Twisk, W.L.J.M. Deville, et al.
Prognostic factors for NP in general practice
Pain, 110 (2004), pp. 639-645Hoy et al., 2014
Hoy D, March L, Woolf A, et al.
The Global Burden of Neck Pain:
Estimates From the Global Burden of Disease 2010 Study.
Ann Rheum Dis. 2014 (Jul); 73 (7): 1309–1315Hurwitz et al., 2004
E.L. Hurwitz, et al.
Adverse reactions to chiropractic treatment and their effects on satisfaction
and clinical outcomes among patients enrolled in the UCLA NP study
J. Manip. Physiol. Ther., 27 (2004), pp. 16-25Hurwitz et al., 2005
E.L. Hurwitz, et al.
Frequency and Clinical Predictors of adverse reactions
to chiropractic care in the UCLA NP Study
Spine, 30 (2005), pp. 1477-1484Hush et al., 2011
J.M. Hush, C.C. Lin, Z.A. Michaleff, et al.
Prognosis of acute idiopathic neck pain is poor:
a systematic review and meta-analysis
Arch. Phys. Med. Rehabil., 92 (5) (2011), pp. 824-829Kamper et al., 2010
S.J. Kamper, R.W.J.G. Ostelo, D.L. Knol, et al.
Global Perceived Effect scales provided reliable assessments of health transition
in people with musculoskeletal disorders, but ratings
are strongly influenced by current status
J. Clin. Epidemiol., 63 (2010), pp. 760-766Keijsers et al., 2010
E. Keijsers, et al.
Psychosocial factors predicted nonrecovery in both specific
and nonspecific diagnoses at arm, neck, and shoulder
J. Clin. Epidemiol., 63 (12) (2010), pp. 1370-1379, 10.1016/j.jclinepi.2010.01.015Kerry and Taylor, 2014
R. Kerry, A. Taylor
Cervical spine pre-treatment screening for arterial dysfunction:
out with the old, in with the new
InTouch, 147 (2014), pp. 10-14Kranenburg et al., 2017
H.A. Kranenburg, M.A. Schmitt, E.J. Puentedura, et al.
Adverse events associated with the use of cervical spine manipulation
or mobilization and patient characteristics: a systematic review
Musculoskel Sci Pract, 28 (2017), pp. 32-38Landers et al., 2008
M.R. Landers, R.V. Creger, C.V. Baker, et al.
Fear avoidance beliefs questionnaire in NP
Man. Ther., 13 (3) (2008), pp. 239-248Leaver et al., 2013
A.M. Leaver, C.G. Maher, J.H. McAuley, G. Jull, J. Latimer, K.M. Refshauge
People seeking treatment for a new episode of NP typically
have rapid improvement in symptoms: an observational study
J. Physiother., 59 (2013), pp. 31-37Mallen et al., 2007
C.D. Mallen, G. Peat, E. Thomas, K.M. Dunn, P.R. Croft
Prognostic factors for musculoskeletal pain in primary care:
a systematic review
Br. J. Gen. Pract., 57 (541) (2007 Aug 1), pp. 655-661Ogundimu et al., 2016
E.O. Ogundimu, D.G. Altman, G.S. Collins
Adequate sample size for developing prediction models is
not simply related to events per variable
J. Clin. Epidemiol., 76 (2016), pp. 175-182Paanalahti et al., 2014
K. Paanalahti, L.W. Holm, M. Nordin, et al.
Adverse events after manual therapy among patients seeking
care for neck and/or back pain: a randomized controlled trial
BMC Muscoskel. Disord., 15 (2014), p. 77Paanalahti et al., 2014b
K. Paanalahti, L.W. Holm, M. Nordin, M. Asker, J. Lyander, E. Skillgate
Adverse events after manual therapy among patients seeking
care for neck and/or back pain: a randomized controlled trial
BMC Muscoskel. Disord., 15 (1) (2014), p. 77Palml ö f et al., 2016
L. Palmlöf, L.W. Holm, L. Alfredsson, E. Skillgate
Expectations of recovery: a prognostic factor in patients
with NP undergoing manual therapy treatment
Eur. J. Pain, 20 (2016), pp. 1384-1391, 10.1002/ejp.861Peters et al., 2019
R. Peters, J.-H.A.M. Mutsaers, A.P. Verhagen, B.W. Koes, A.L. Pool-Goudzwaard
Prospective cohort study of patients with neck pain in a
manual therapy setting: design and baseline measures
J. Manip. Physiol. Ther., 42 (7) (2019 Sep), pp. 471-479, 10.1016/j.jmpt.2019.07.001Rubinstein et al., 2007
Rubinstein SM, Leboeuf-Yde C, Knol DL, de Koekkoek TE, Pfeifle CE, van Tulder MW.
The Benefits Outweigh the Risks for Patients Undergoing Chiropractic
Care for Neck Pain A Prospective, Multicenter, Cohort Study
J Manipulative Physiol Ther 2007 (Jul); 30 (6): 408–418Rubinstein et al., 2008
S.M. Rubinstein, C. Leboeuf-Yde, D.L. Knol, et al.
Predictors of adverse events following chiropractic care
for patients with neck pain
JMPT (J. Manip. Physiol. Ther.), 31 (2) (2008), pp. 94-103Schafer, 1997
J.L. Schafer
Analysis of Incomplete Multivariate Data
Chapman and Hall, London (1997)Schellingerhout et al., 2012
J.M. Schellingerhout, A.P. Verhagen, M.W. Heymans, B.W. Koes, H.C. De Vet, C.B. Terwee
Measurement properties of disease specific questionnaires
in patients with NP: a systematic review
Qual. Life Res., 21 (4) (2012), pp. 659-670Steyerberg et al., 2000
E.W. Steyerberg, M.J. Eijkemans, F.E. Harrell Jr., J.D. Habbema
Prognostic modelling with logistic regression analysis:
a comparison of selection and estimation methods in small data sets
Stat. Med., 19 (2000), pp. 1059-1079Tabell et al., 2019
V. Tabell, I.M. Tarkka, L.W. Holm, et al.
Do adverse events after manual therapy for back and/or neck pain
have an impact on the chance to recover? A cohort study
Chiropr. Man. Ther., 27 (2019), p. 27, 10.1186/s12998-019-0248-9Van der Ploeg et al., 2014
T. Van der Ploeg, P.C. Austin, E.W. Steyerberg
Modern modelling techniques are data hungry:
a simulation study for predicting dichotomous endpoints
BMC Med. Res. Methodol., 14 (1) (2014), p. 137Vernon, 2008
H. Vernon
The Neck Disability Index: State-of-the-Art, 1991-2008
J Manipulative Physiol Ther 2008 (Sep); 31 (7): 491–502Vineis, 2008
P. Vineis
Smoking and impact on health
Eur. Respir. Rev., 17 (2008), pp. 182-186Vittinghoff and McCulloch, 2007
E. Vittinghoff, C.E. McCulloch
Relaxing the rule of ten events per variable in logistic and Cox regression
Am. J. Epidemiol., 165 (6) (2007), pp. 710-718Von Elm et al., 2007
E. Von Elm, D.G. Altman, M. Egger, S.J. Pocock, P.C. Gøtzsche, et al.
The strengthening the reporting of observational studies in epidemiology
(STROBE) statement: guidelines for reporting observational studies
PLoS Med., 4 (10) (2007), p. e296 10.1371/journal.pmed. 0040296Vos et al., 2008
C.J. Vos, A.P. Verhagen, J. Passchier, B.W. Koes
Clinical course and prognostic factors in acute NP:
an inception cohort study in general practice
Pain Med., 9 (5) (2008 Jul-Aug), pp. 572-580Walton et al., 2013
D.M. Walton, L.J. Carroll, H. Kasch, et al.
An overview of systematic reviews on prognostic factors in neck pain:
results from the international collaboration on neck pain (ICON) project
Open Orthop. J., 7 (Suppl. 4) (2013), pp. 494-505 M9Wynants et al., 2015
L. Wynants, W. Bouwmeester, K.G. Moons, et al.
A simulation study of sample size demonstrated the importance of the number
of events per variable to develop prediction models in clustered data
J. Clin. Epidemiol., 68 (12) (2015), pp. 1406-1414
Return to ADVERSE EVENTS
Return to CHRONIC NECK PAIN
Since 7-19-2023


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |