

Low-value Care in Musculoskeletal Health Care:
Is There a Way Forward?This section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Pain Practice 2022 (Sep); 22 (Suppl 2): 65–70 ~ FULL TEXT
OPEN ACCESS Jan Hartvigsen PhD, Steven J. Kamper PhD, Simon D. French PhD
Department of Sports Science and Clinical Biomechanics,
Center for Muscle and Joint Health,
University of Southern Denmark,
Odense M, Denmark.
Arch Physiother 2021Background: Low-value care that wastes resources and harms patients is prevalent in health systems everywhere.
Methods: As part of an invited keynote presentation at the Pain in Motion IV conference held in Maastricht, Holland, in May 2022, we reviewed evidence for low-value care in musculoskeletal conditions and discussed possible solutions.
Results: Drivers of low-value care are diverse and affect patients, clinicians, and health systems everywhere. We show that low-value care for back pian, neck pain, and osteoarthritis is prevalent in all professional groups involved in caring for people who seek care for these conditions. Implementation efforts that aim to reverse low-value care seem to work better if designed using established conceptual and theoretical frameworks.
There is more like this @ our:
LOW BACK PAIN Page and our
SPINAL PAIN MANAGEMENT PageConclusion: Low-value care is prevalent in the care of people with musculoskeletal conditions. Reducing low-value care requires behaviour change among patients and clinicians as well as in health systems. There is evidence that behaviour change can be facilitated through good conceptual and theoretical frameworks but not convincing evidence that it changes patient outcomes.
Keywords: back pain; clinical guidelines; evidence-based practice; low-value care; osteoarthritis.
From the Full-Text Article:
Low-Value Care Is Prevalent In Health Systems
Low-value care is defined as health services that confer little or no benefit to patients or where risk of harm exceeds probable benefit, according to best available evidence. [1] Low-value care is common across health systems globally and includes ineffective screening programs, unnecessary diagnostic testing and imaging, ineffective and harmful treatments, and inefficient organization of health systems. [2, 3] It is estimated that only around 60% of services are in line with best available evidence, 30% is waste, duplication, or low value, and 10% is harmful. [4] Low-value care is not a trivial issue; it adds cost and consumes resources, causes iatrogenic harm, and impedes delivery of high-value care that reliably provides health benefits for individuals and populations. [5]
Drivers of low-value care are numerous. In some circumstances clinicians act according to their own financial benefit rather than the patient's best interests. [6] For example, provision of ineffective services can be motivated by commercial ties to ancillary service facilities or to pharmaceutical and medical device industries. [7, 8] Clinician knowledge, assumptions, and bias also play a role in provision of low-value care. Clinicians may be unfamiliar with best practice clinical guidelines or choose to disregard recommendations when evidence contradicts their training, professional identity, or perceived clinical experience. [9, 10] The quality of the patient–clinician relationship is important. For example, when a patient distrusts the clinician and demands further testing or treatment, or when a clinician orders testing or imaging to protect against litigation as part of defensive medicine. [11] Further, the way health systems are organized can promote low-value care. Hospital income may be tied to unnecessary procedures, profits of private insurance companies sometimes increase with consumption of health care, and pharmaceutical companies may subsidize patient payments in order to increase patient demand. [12] Final, perverse incentives exist in healthcare systems when interventions discouraged in evidence-based guidelines (eg, opioids, imaging, and surgeries) are widely available and publicly funded, whereas recommended treatments (eg, physical and psychological therapies) are not. [13]
In this paper, we describe what high-value care should look like according to guideline recommendations for people with musculoskeletal conditions (MSK) and provide examples of low-value care. We argue the need for behavior change among patients, clinicians, and in healthcare systems, and we present models for implementation that might facilitate delivery of high-value care. This paper is not a systematic review of the evidence; however, in preparation, we performed repeated literature searches of PubMed and Scopus to identify guideline recommendations for treatment of common MSK conditions (back pain, neck pain, and osteoarthritis), as well as systematic reviews or primary studies of evidence regarding adherence to these recommendations.
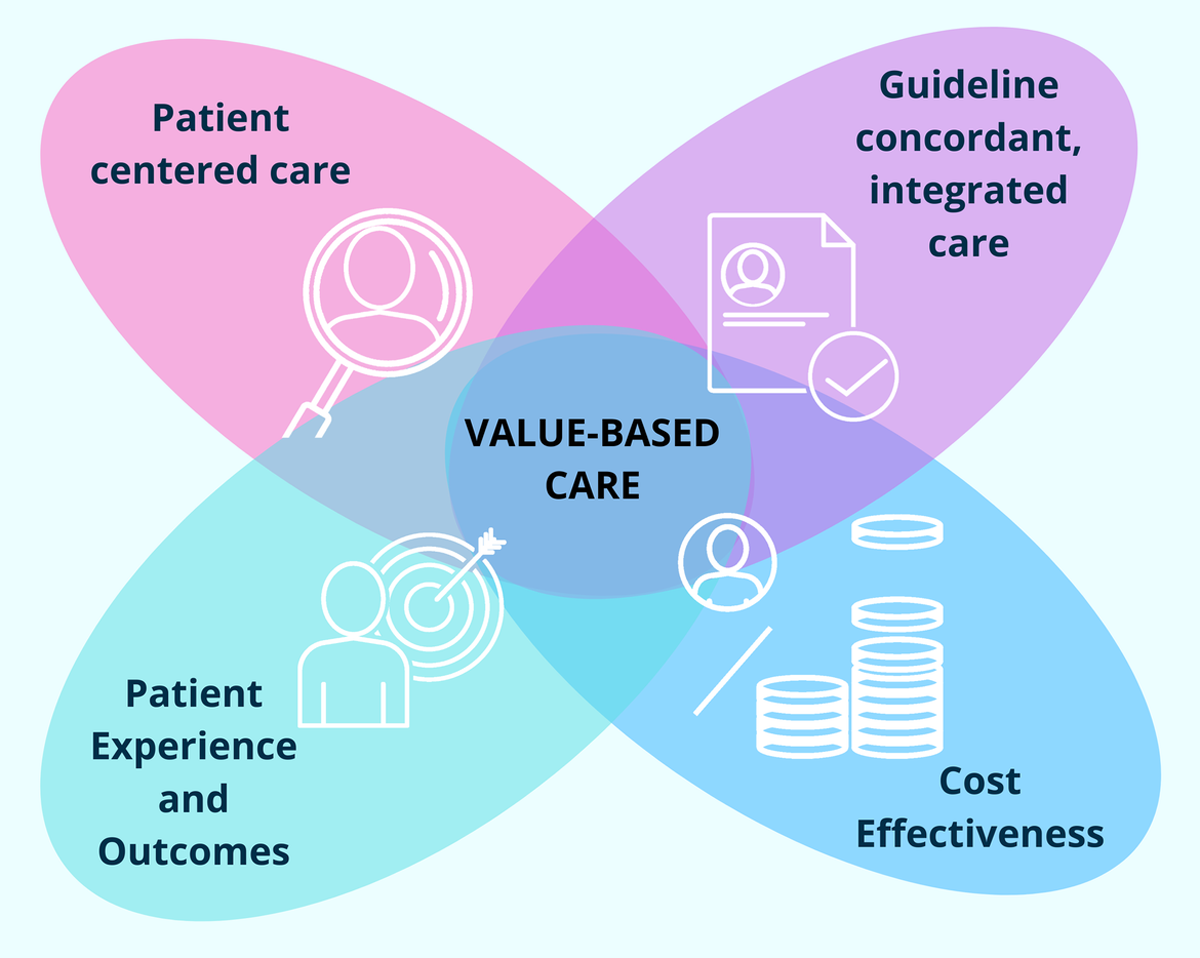
Guideline Recommended Care
Clinical practice guidelines across MSK conditions provide several consistent recommendations, including the following. [14, 15]
patient-centered care containing information and education about the condition;
consideration of psychosocial factors as appropriate for improving pain and function;
encouraging people to remain at work;
physical activity and exercise interventions;
manual therapy only as an adjunct to other treatments;
pharmacological options for short-term pain relief with careful consideration of potential harm harms;
advice to not perform routine imaging; and
high-quality non-surgical care prior to surgery
Specifically, for low back pain, there is broad consensus that patients should initially receive non-pharmacological care. [16–18] Recommendations in guidelines for neck pain are similar to those in low back pain guidelines, although oral and topical analgesics are recommended as first-line treatments. [16] For people with hip or knee osteoarthritis, provision of exercise programs and support for weight management is emphasized. [19, 20]
Non-Guideline Recommended Care Is Prevalent
There is overwhelming evidence that many patients receive care that does not reflect guideline recommendations, a pattern that is not confined to particular health professions. Kamper et al systematically reviewed studies describing usual care for people with back pain and found that if patients sought care from general practitioners, fewer than 20% of patients received evidence-based information and advice, around 25% received referral for imaging, and between 20% and 30% received a prescription for opioids. When care is delivered in emergency departments, 30% received imaging and up to 60% were prescribed opioids.
Furthermore, there is inconsistent provision of education and advice regarding maintenance of physical activity. [21] In a systematic review including 94 primary studies evaluating whether physical therapists provided care consistent with guidelines for people with back pain, Zadro et al found that approximately 40% did not. [22] Amorin-Woods demonstrated that chiropractors provided inappropriate care to back pain patients 30% of the time. [23] In Australia, an audit of online information on clinic webpages and on Facebook revealed that 72% of chiropractors and 61% of physiotherapists had breaches of advertising guidelines when marketing their practice and services to patients and the public. [24] Further, a scoping review of the chiropractic literature demonstrated that adherence to imaging guidelines is sub-optimal. [25]
Hagen et al reviewed studies that dealt with primary care for knee or hip osteoarthritis and found that less than half received an assessment of their pain and/or function, and fewer than 40% received recommendations for exercise or were offered education and self-management support. [26] Thorlund et al scrutinized prescription registries in Sweden and found that among more than 8,000 people with newly diagnosed osteoarthritis of the knee or hip, more than half of incident opioid prescriptions were prescribed inappropriately according to national treatment guidelines. [27] Nationwide reviews of health systems indicators show that just 45% of Australians, [28] and less than 30% of UK [29] patients with OA receive evidence-based care.
Surgery is arguably the most radical treatment for any MSK disorder. Apart from injuries, the most common reason for orthopedic surgery is chronic pain related to osteoarthritis, back pain, or neck pain. [30] Justification for these surgeries often relies on structural or mechanistic rationales, which ignores the influence of psychological and social factors on chronic pain and the poor link between degenerative changes and pain. For example, structural pathology was not related to patient-reported pain and function in Danish patients undergoing meniscal surgery in the knee, [31] and Brinjiki et al systematically reviewed 33 original papers reporting imaging findings on MRI for more than 3,100 asymptomatic individuals and found that the prevalence approached those of people with symptoms in the back. For arthroscopic surgery for pain and degenerative changes in the knee, there is suspicion that they cause greater harms than benefit [32, 33] and it is not possible to reliably identify subgroups of patients that benefit from the surgery. [34]
In the United States, spinal fusion surgery increased 600% between 1993 and 2011 mainly for the treatment of “degenerative disc disease” [35] despite no evidence that fusion surgery is superior to well-structured rehabilitation programs [36] and despite no evidence showing an increase in prevalence of the condition. [37] In addition, complex surgical procedures in the spine have greater risk of complications with no additional benefit over simpler surgical procedures, [38] or indeed not performing the procedure at all. [35]
Reversing Low-Value Care Requires Change At All Levels
The shift in MSK guideline recommendations in recent decades to non-pharmacological options as first-line care and the identification of widespread low-value care has brought challenges for healthcare systems everywhere. To bring care into line with best available guideline recommended evidence, behavior change at multiple levels is required including for patients, clinicians, organization of the clinical setting, and in the broader healthcare system. Before we can address the problems, implementation science researchers suggest that we need to understand the function of the current systems, including what is currently being done in clinical practice, how and why this is different from guideline recommendations, and what the potential solutions for bridging the gaps might be. Through systematic identification of barriers and facilitators to change, we can select intervention components that address each one specifically. [39]
Involvement of patients in planning and evaluation of health service delivery is recommended by the World Health Organization. [40] This is motivated by a desire to design health systems that meet the needs of the end users. Olsson et al reviewed 34 studies from eight countries found evidence that patient involvement in designing service delivery is time consuming but can result in increased collaboration between healthcare providers and patients, increased motivation for organizational change, and changed clinical practice. [41]
At the clinician level, dissemination of information about best practice and clinical practice guidelines, and one-off implementation efforts targeting individual clinicians does not generate sustained behavior change and high-value care. [42] In a Cochrane review including 30 original studies, Tzortziou Brown et al investigated the effectiveness of professional interventions for general practitioners that aim to improve the management of MSK conditions in primary care. [43] They concluded that feedback on performance combined with guideline dissemination may lead to small improvements in guideline-consistent GP behavior with regard to low back pain, while GP education on osteoarthritis pain and the use of influential physicians may lead to slight improvement in patient outcomes and guideline-consistent behavior. [43]
At the health system level, authors of a recent systematic review identified 28 original studies evaluating the impact of implementing pathways designed to improve care as well as relieve overburdened secondary-care centers. They found that service effiency could be improved through decreased wait times and appropriate use of consultant appointments, but that it was uncertain whether patient outcomes were improved. [44] In addition, it is important to be aware that broader health systems issues such as reimbursement schemes and professional hierarchies influence what care is delivered and how. [45, 46]
Medical societies and health professional associations are addressing low-value care, for example, via the establishment and support of the Choosing Wisely campaign. The aim of Choosing Wisely is to decrease healthcare waste and iatrogenesis, and one target of the campaign is imaging for low back pain. [47] In Choosing Wisely professional bodies make public a core set of principles with recommendations to clinicians, patients, and other stakeholders regarding which interventions and services they should offer, and which not. Since its launch in 2012, Choosing Wisely has been established in more than 20 countries and has more than 100 participating professional associations [47]; however, large-scale impact of this initiative has not yet been documented. [48]
Effective Implementation Requires Good Conceptual And Theoretical Frameworks
The use of theory to inform design of interventions can help to overcome what has been termed the “ISLAGIATT principle” (It Seemed Like A Good Idea At The Time), where inherent biases and personal beliefs, rather than theory, evidence, and a systematic approach, guide decisions. [49, 50] Although research into how to best achieve behavior change has intensified in recent years, there is currently no strong basis for favoring one particular solution over another to overcome a particular low-value care problem. [51]
Systematic assessment and selection of intervention components that address identified, modifiable barriers and enablers underpinned by an overarching framework is the most promising way forward. [52] To date, however, implementation interventions to address low-value care have been largely based on simple and mostly unstated models of human behavior, or in the case of the few theory-based interventions, a systematic process has not been followed. [52–54] Davis et al reviewed 235 evaluations of guideline dissemination and implementation studies and concluded that justification for the choice of implementation interventions was typically poor. Only 22.5% of interventions were based on a theory, and in just 6% the theory was explicit. [54] Nonetheless, various conceptual and theoretical frameworks are applicable when aiming to replace low-value care with better solutions. [52]
Importantly, there is a growing body of evidence demonstrating that interventions based on theory are more effective in changing behavior, even though few specific theories have been robustly tested in healthcare settings. [55] Therefore the explicit use of theories and frameworks is encouraged based on available evidence, and guidance is available. [56]
Examples of commonly used theoretical implementation frameworks includeThe Theoretical Domains Framework [57, 58];
the Consolidated Framework for Implementation Research (CFIR) [59];
the Exploration, Preparation, Implementation, Sustainment (EPIS) framework [60]; and
the Re-AIM framework. [31]
Examples Of Interventions Designed To Facilitate High-Value Care
There are attempts to implement programs that seek to address barriers to the uptake of guideline recommendations such as clinician knowledge and confidence and organizational barriers in the clinic. Examples include the PARTNER study where a model of service delivery that targets general practitioners and their patients seeking care for knee osteoarthritis are implemented. [62] Patients are referred to a behavior change intervention aimed at promoting self-management, and the GP is trained in delivering a tailored intervention focusing on exercise and weight loss. [62] In the SOLAS project, physiotherapists are trained to deliver a group-based intervention involving information and exercises supported by an e-health leaning program for people with persistent back pain. [63] The Danish GLA:D project is a structured program of patient education integrated with a group-based supervised exercise for people with osteoarthritis of the knee or hip [64, 65] or persistent and/or recurrent back pain. Outcomes from people receiving GLA:D are systematically followed in clinical registries and data are made public. [66, 67]
In the ALIGN cluster randomized trial, French et al compared the effectiveness of a tailored, multi-faceted intervention based on guideline recommendations aiming at reducing inappropriate imaging referral and improve outcomes to passive dissemination of the guideline in people seeking care for acute back pain from physiotherapists and chiropractors in Victoria, Australia. [68] They found that clinicians in the intervention group were more likely to provide advice about staying active, but there were no important differences in X-ray referral and no difference in patient outcomes.
Finally, Taylor et al compared the effectiveness of a participative group intervention that introduced cognitive behavioral approaches designed to promote self-management to usual care and relaxation music. They found that it was not effective for reducing back-related disability; however, some differences favoring the intervention group were found for depression and social integration, but not for pain intensity, self-efficacy, or global perceived effect. [69]
Conclusion
Low-value care that wastes resources and harms patients is prevalent in health systems worldwide. Low-value care affects the millions of people who suffer from MSK pain and disability who receive care that is contrary to recommendations in evidence-based clinical practice guidelines. Low-value care is provided by all health professions. If the trend of pervasive low-value care is to be reversed, a concerted effort that involves all stakeholders including patients, clinicians, professional organizations, funders, decision makers, and health system administrators is needed. Such efforts should build on transparent investigation of barriers and enablers to best practice care delivery and designed using established conceptual and theoretical frameworks.
Conflict Of Interest
Jan Hartvigsen declares that he is co-developer of the GLA:D Back project, which is mentioned in this paper. He has no financial outcome from the project.
References:
Elshaug AG, Rosenthal MB, Lavis JN, Brownlee S, Schmidt H, Nagpal S, et al.
Levers for addressing medical underuse and overuse:
achieving high-value health care.
Lancet. 2017; 390: 191– 202.Schwartz AL, Landon BE, Elshaug AG, Chernew ME, McWilliams JM.
Measuring low-value care in Medicare.
JAMA Int Med. 2014; 174: 1067– 76.Shrank WH, Rogstad TL, Parekh N.
Waste in the US health care system: estimated costs and potential for savings.
JAMA. 2019; 322: 1501– 9.Braithwaite J, Glasziou P, Westbrook J.
The three numbers you need to know about healthcare: the 60-30-10 challenge.
BMC Med. 2020; 18: 102.Razmaria AA.
High-value care.
Jama. 2015; 314: 2462.Saini V, Garcia-Armesto S, Klemperer D, Paris V, Elshaug AG, Brownlee S, et al.
Drivers of poor medical care.
Lancet. 2017; 390: 178– 90.Mitchell JM, Sass TR.
Physician ownership of ancillary services:
indirect demand inducement or quality assurance?
J Health Econ. 1995; 14: 263– 89.Tefferi A, Kantarjian H, Rajkumar SV, Baker LH, Abkowitz JL, Adamson JW, et al.
In support of a patient-driven initiative and petition to
lower the high price of cancer drugs.
Mayo Clin Proc. 2015; 90: 996– 1000.Sirovich BE, Lipner RS, Johnston M, Holmboe ES.
The association between residency training and internists' ability to practice conservatively.
JAMA Int Med. 2014; 174: 1640– 8.Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, et al.
Why don't physicians follow clinical practice guidelines?
A framework for improvement.
Jama. 1999; 282: 1458– 65.Djulbegovic B, Hozo I, Ioannidis JP.
Modern health care as a game theory problem.
Eur J Clin Invest. 2015; 45: 1– 12.Prasad V, Cifu A.
Medical reversal: why we must raise the bar before adopting new technologies.
Yale J Biol Med. 2011; 84: 471– 8.Buchbinder R, van Tulder M, Öberg B, Costa LM, Woolf A, at al.
Low Back Pain: A Call For Action
Lancet. 2018 (Jun 9); 391 (10137): 2384–2388
This is the fourth of 4 articles in the remarkable Lancet Series on Low Back PainBabatunde OO, Jordan JL, Van der Windt DA, Hill JC, Foster NE, Protheroe J.
Effective treatment options for musculoskeletal pain in primary care:
a systematic overview of current evidence.
PLoS One. 2017; 12:e0178621.Lin I, Wiles L, Waller R, Goucke R, Nagree Y, Gibberd M, et al.
What Does Best Practice Care for Musculoskeletal Pain Look Like?
Eleven Consistent Recommendations From High-quality
Clinical Practice Guidelines: Systematic Review
British J Sports Medicine 2020 (Jan); 54 (2): 79–86Corp N, Mansell G, Stynes S, et al..
Evidence-based treatment recommendations for neck and low back pain
across Europe: A systematic review of guidelines
European J Pain 2021 (Feb); 25 (2): 275–295Qaseem A, Wilt TJ, McLean RM, Forciea MA;
Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain:
A Clinical Practice Guideline From the American College of Physicians
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 514–530Oliveira CB, Maher CG, Pinto RZ, Traeger AC, Lin CC, Chenot JF, et al.
Clinical practice guidelines for the management of non-specific
low back pain in primary care: an updated overview.
Eur Spine J. 2018; 27: 2791– 803.McAlindon TE, Bannuru RR, Sullivan MC, Arden NK, Berenbaum F, Bierma-Zeinstra SM, et al.
OARSI guidelines for the non-surgical management of knee osteoarthritis.
Osteoarthr Cartil. 2014; 22: 363– 88.Hunter DJ, Bierma-Zeinstra S.
Osteoarthritis.
Lancet. 2019; 393: 1745– 59.Kamper SJ, Logan G, Copsey B, et –al.
What is Usual Care for Low Back Pain? A Systematic Review of
Health Care Provided to Patients with Low Back Pain in
Family Practice and Emergency Departments
Pain. 2020 (Apr); 161 (4): 694–702Zadro J, O'Keeffe M, Maher C.
Do Physical Therapists Follow Evidence-based Guidelines When
Managing Musculoskeletal Conditions? Systematic Review
BMJ Open. 2019 (Oct 7); 9 (10): e032329Amorin-Woods LG, Beck RW, Parkin-Smith GF, Lougheed J, Bremner AP.
Adherence to Clinical Practice Guidelines Among Three Primary
Contact Professions: A Best Evidence Synthesis of the Literature
for the Management of Acute and Subacute Low Back Pain
J Can Chiropr Assoc 2014 (Sept); 58(3): 220–237Simpson JK.
At-risk advertising by Australian chiropractors and physiotherapists.
Chiropr Man Therap. 2019; 27: 30.Bussieres AE, Al Zoubi F, Stuber K, French SD, Boruff J, Corrigan J, et al.
Evidence-based Practice, Research Utilization, and Knowledge Translation
in Chiropractic: A Scoping Review
BMC Complement Altern Med. 2016 (Jul 13); 16 (1): 216Hagen KB, Smedslund G, Osteras N, Jamtvedt G.
Quality of community-based osteoarthritis care:
a systematic review and meta-analysis.
Arthritis Care Res. 2016; 68: 1443– 52.Thorlund JB, Turkiewicz A, Prieto-Alhambra D, Englund M.
Inappropriate opioid dispensing in patients with knee and hip osteoarthritis:
a population-based cohort study.
Osteoarthr Cartil. 2020; 28: 146– 53.Runciman WB, Coiera EW, Day RO, Hannaford NA, Hibbert PD, Hunt TD, et al.
Towards the delivery of appropriate health care in Australia.
Med J Aust. 2012; 197: 78– 81.Steel N, Bachmann M, Maisey S, Shekelle P, Breeze E, Marmot M, et al.
Self reported receipt of care consistent with 32 quality indicators:
national population survey of adults aged 50 or more in England.
BMJ. 2008; 337:a957.Rose J, Weiser TG, Hider P, Wilson L, Gruen RL, Bickler SW.
Estimated need for surgery worldwide based on prevalence of diseases:
a modelling strategy for the WHO Global Health estimate.
Lancet Glob Health. 2015; 3(Suppl 2): S13– 20.Tornbjerg SM, Nissen N, Englund M, Jorgensen U, Schjerning J, Lohmander LS, et al.
Structural pathology is not related to patient-reported pain
and function in patients undergoing meniscal surgery.
Br J Sports Med. 2017; 51: 525– 30.Thorlund JB, Juhl CB, Roos EM, Lohmander LS.
Arthroscopic surgery for degenerative knee: systematic review
and meta-analysis of benefits and harms.
BMJ. 2015; 350:h2747.Lohmander LS, Thorlund JB, Roos EM.
Routine knee arthroscopic surgery for the painful knee
in middle-aged and old patients—time to abandon ship.
Acta Orthop. 2016; 87: 2– 4.Pihl K, Ensor J, Peat G, Englund M, Lohmander S, Jorgensen U, et al.
Wild goose chase – no predictable patient subgroups benefit from
meniscal surgery: patient-reported outcomes of 641 patients
1 year after surgery.
Br J Sports Med. 2020; 54: 13– 22.Harris IA, Sidhu V, Mittal R, Adie S.
Surgery for chronic musculoskeletal pain: the question of evidence.
Pain. 2020; 161: S95– S103.Mirza SK, Deyo RA.
Systematic review of randomized trials comparing lumbar fusion surgery
to nonoperative care for treatment of chronic back pain.
Spine. 2007; 32: 816– 23.Deyo RA.
Fusion surgery for lumbar degenerative disc disease:
still more questions than answers.
Spine J. 2015; 15: 272– 4.Machado GC, Maher CG, Ferreira PH, Harris IA, Deyo RA, McKay D, et al.
Trends, complications, and costs for hospital admission
and surgery for lumbar spinal stenosis.
Spine. 2017; 42: 1737– 43.French SD, Green SE, O'Connor DA, McKenzie JE, Francis JJ, Michie S, et al.
Developing theory-informed behaviour change interventions to implement
evidence into practice: a systematic approach using the theoretical domains framework.
Implement Sci. 2012; 7: 38.World Health Organization.
Global action plan for the prevention and control of
non-communicable diseases 2013–2022.
Geneva: World Health Organization; 2013.Sandvin Olsson AB, Strom A, Haaland-Overby M, Fredriksen K, Stenberg U.
How can we describe impact of adult patient participation in
health-service development? A scoping review.
Patient Educ Couns. 2020; 103: 1453– 66.Mesner SA, Foster NE, French SD.
Implementation Interventions to Improve the Management of
Non-specific Low Back Pain: A Systematic Review
BMC Musculoskelet Disord. 2016 (Jun 10); 17: 258Tzortziou Brown V, Underwood M, Mohamed N, Westwood O, Morrissey D.
Professional interventions for general practitioners on
the management of musculoskeletal conditions.
Cochrane Database Syst Rev. 2016;(5):CD007495.Murphy C, French H, McCarthy G, Cunningham C.
Clinical pathways for the management of low back pain from
primary to specialised care: a systematic review.
Eur Spine J. 2022; 31: 1846– 65.Ingvarsson S, Augustsson H, Hasson H, Nilsen P, von Thiele Schwarz U.
Why do they do it? A grounded theory study of the use of
low-value care among primary health care physicians.
Implement Sci. 2020; 15: 93.Hall AM, Scurrey SR, Pike AE, Albury C, Richmond HL, Matthews J, et al.
Physician-reported barriers to using evidence-based recommendations for
low back pain in clinical practice: a systematic review and synthesis of
qualitative studies using the theoretical domains framework.
Implement Sci. 2019; 14: 49.Born KB, Levinson W.
Choosing wisely campaigns globally: a shared approach
to tackling the problem of overuse in healthcare.
J Gen Fam Med. 2019; 20: 9– 12.Hong AS, Ross-Degnan D, Zhang F, Wharam JF.
Small decline in low-value back imaging associated with
the ‘choosing Wisely’ Campaign, 2012–14.
Health Aff. 2017; 36: 671– 9.Hughes CM, Cadogan CA, Ryan CA.
Development of a pharmacy practice intervention: lessons from the literature.
Int J Clin Pharmacol. 2016; 38: 601– 6.Michie S, van Stralen MM, West R.
The behaviour change wheel: a new method for characterising
and designing behaviour change interventions.
Implement Sci. 2011; 6: 42.Grimshaw JM, Eccles MP, Lavis JN, Hill SJ, Squires JE.
Knowledge translation of research findings.
Implement Sci. 2012; 7: 50.Nilsen P.
Making sense of implementation theories, models and frameworks.
Implement Sci. 2015; 10: 53.Michie S.
Designing and implementing behaviour change interventions to improve population health.
J Health Serv Res Policy. 2008; 13(Suppl 3): 64– 9.Davies P, Walker AE, Grimshaw JM.
A systematic review of the use of theory in the design of guideline dissemination
and implementation strategies and interpretation of the results of rigorous evaluations.
Implement Sci. 2010; 5: 14.Baker R, Camosso-Stefinovic J, Gillies C, Shaw EJ, Cheater F, Flottorp S, et al.
Tailored interventions to address determinants of practice.
Cochrane Database Syst Rev. 2015;(4): CD005470.Moullin JC, Dickson KS, Stadnick NA, Albers B, Nilsen P, Broder-Fingert S, et al.
Ten recommendations for using implementation frameworks in research and practice.
Implement Sci Commun. 2020; 1: 42.Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A, et al.
Making psychological theory useful for implementing
evidence based practice: a consensus approach.
Qual Saf Health Care. 2005; 14: 26– 33.Atkins L, Francis J, Islam R, O'Connor D, Patey A, Ivers N, et al.
A guide to using the theoretical domains framework of
behaviour change to investigate implementation problems.
Implement Sci. 2017; 12: 77.Keith RE, Crosson JC, O'Malley AS, Cromp D, Taylor EF.
Using the consolidated framework for implementation research (CFIR)
to produce actionable findings: a rapid-cycle evaluation approach to improving implementation.
Implement Sci. 2017; 12: 15.Moullin JC, Dickson KS, Stadnick NA, Rabin B, Aarons GA.
Systematic review of the exploration, preparation, implementation, sustainment (EPIS) framework.
Implement Sci. 2019; 14: 1.Glasgow RE, Estabrooks PE.
Pragmatic applications of RE-AIM for health care initiatives
in community and clinical settings.
Prev Chronic Dis. 2018; 15: E02.Hunter DJ, Hinman RS, Bowden JL, Egerton T, Briggs AM, Bunker SJ, et al.
Effectiveness of a new model of primary care management on knee pain
and function in patients with knee osteoarthritis: protocol for THE PARTNER STUDY.
BMC Musculoskelet Disord. 2018; 19: 132.Hurley DA, Keogh A, Mc Ardle D, Hall AM, Richmond H, Guerin S, et al.
Evaluation of an E-learning training program to support implementation
of a group-based, theory-driven, self-management intervention for
osteoarthritis and low-Back pain: pre-post study.
J Med Internet Res. 2019; 21:e11123.Roos EM, Barton CJ, Davis AM, McGlasson R, Kemp JL, Crossley KM, et al.
GLA:D to have a high-value option for patients with knee and hip arthritis
across four continents: good life with osteoArthritis from Denmark.
Br J Sports Med. 2018; 52: 1544– 5.Skou ST, Roos EM.
Good life with osteoArthritis in Denmark (GLA:D): evidence-based education
and supervised neuromuscular exercise delivered by certified physiotherapists nationwide.
BMC Musculoskelet Disord. 2017; 18(1): 72.Kjaer P, Kongsted A, Ris I, Abbott A, Rasmussen CDN, Roos EM, et al.
GLA:D® Back group-based patient education integrated with exercises to
support self-management of back pain-development, theories and scientific evidence.
BMC Musculoskelet Disord. 2018; 19(1): 418.Kongsted A, Hartvigsen J, Boyle E, Ris I, Kjaer P, Thomassen L, et al.
GLA:D® back: group-based patient education integrated with exercises to
support self-management of persistent back pain—feasibility of implementing
standardised care by a course for clinicians.
Pilot Feasibility Stud. 2019; 5: 65.French SD, O'Connor DA, Green SE, Page MJ, Mortimer DS, Turner SL, et al.
Improving adherence to acute low back pain guideline recommendations
with chiropractors and physiotherapists: the ALIGN cluster randomised controlled trial.
Trials. 2022; 23(1): 142.Taylor SJ, Carnes D, Homer K, Kahan BC, Hounsome N, Eldridge S, et al.
Novel three-Day, community-based, nonpharmacological group intervention
for chronic musculoskeletal pain (COPERS): a randomised clinical trial.
PLoS Med. 2016; 13:e1002040.
Return to LOW BACK PAIN
Return to SPINAL PAIN MANAGEMENT
Since 9-17-2022


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |