

A Systems Approach for Assessing Low Back Pain
Care Quality in Veterans Health Administration
Chiropractic Visits: A Cross-Sectional AnalysisThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Manipulative Physiol Ther 2023 (Dec 22) [EPUB] ~ FULL TEXT
OPEN ACCESS Ryan D. Muller, DC, MS • Sarah E. Graham, DC • Xiwen Zhao, MSPH
Anna R. Sites, MSN, RN • Kelsey L. Corcoran, DC • Anthony J. Lisi, DC
VA Connecticut Healthcare System,
West Haven, Connecticut;
Yale School of Medicine,
Yale University,
New Haven, Connecticut.

Objective: The purpose of this study was to explore a systemwide process for assessing components of low back pain (LBP) care quality in Veterans Health Administration (VHA) chiropractic visits using electronic health record (EHR) data.
thods: MeWe performed a cross-sectional quality improvement project. We randomly sampled 1000 on-station VHA chiropractic initial visits occurring from October 1, 2017, to September 30, 2018, for patients with no such visits within the prior 12 months. Characteristics of LBP visits were extracted from VHA national EHR data via structured data queries and manual chart review. We developed quality indicators for history and/or examination and treatment procedures using previously published literature and calculated frequencies of visits meeting these indicators. Visits meeting our history and/or examination and treatment indicators were classified as "high-quality" visits. We performed a regression analysis to assess associations between demographic/clinical characteristics and visits meeting our quality criteria.
Results: There were 592 LBP visits identified. Medical history, physical examination, and neurologic examination were documented in 76%, 77%, and 63% of all LBP visits, respectively. Recommended treatments, such as any manipulation, disease-specific education/advice, and therapeutic exercise, occurred in 75%, 69%, and 40% of chronic visits (n = 383), respectively. In acute/subacute visits (n = 37), any manipulation (92%), manual soft tissue therapy (57%), and disease-specific advice/education (54%) occurred most frequently. Female patients and those with a neck pain comorbid diagnosis were significantly less likely to have a "high-quality" visit, while other regression associations were non-significant.
Conclusion: This study explored a systemwide process for assessing components of care quality in VHA chiropractic visits for LBP. These results produced a potential framework for uniform assessment of care quality in VHA chiropractic visits for LBP and highlight potential areas for improvements in LBP care quality assessments.
Keywords: Chiropractic; Low Back Pain; Quality Assurance, Health Care; Veterans Health.
From the FULL TEXT Article:
Introduction
Low back pain (LBP) causes more years lived with disability (YLDs) worldwide than any other condition and has a global point prevalence of 7.5%. [1] Low back pain is the leading cause of YLDs in the United States (US) population. [2] An estimated $135.5 billion was spent on care for low back and neck pain in the US in 2016, with costs increasing by 6.7% annually from 1996 to 2016. [3, 4] United States veterans are particularly affected by LBP, as it is the second most common musculoskeletal disorder that affects veterans receiving care in the Veterans Health Administration (VHA). [5]
The VHA has been increasing its delivery of evidence-based, non-pharmacologic treatment options for LBP and other pain conditions by expanding Veteran access to a number of treatment approaches, including chiropractic care. [6, 7] Use of chiropractic care in the VHA, most commonly for LBP, has been increasing rapidly, yet little is known about the quality of delivered services. [8, 9]
Appropriate diagnostic workup is an important component of care for patients with LBP. [10] Previous investigators have identified quality indicators, such as key history and examination procedures, that, when present in clinical documentation, serve as markers of a desired LBP workup. [11, 12] However, health care providers’ adherence to some of these elements of quality, such as documenting a thorough neurologic examination and screening for serious diseases, has been shown to be poor. [11]
Providing appropriate management options is also critical in caring for patients with LBP. [13] Evidence from physical therapy and primary care settings, as well as analyses of health care claims data, suggest that guideline-adherent management of patients with LBP may result in better patient outcomes, reduced risk of recurrence, and lower associated medical costs. [14–17] As such, researchers have used clinical practice guidelines (CPGs) as references to assess how often recommended treatment options for LBP are provided in health care settings. [14, 15, 18, 19] Current CPGs recommend non-pharmacologic treatments as first-line therapies in the management LBP. [13, 20, 21] Despite evidence in favor of guideline-adherent care, discrepancies remain between CPG recommendations and the treatments provided to patients with LBP in practice. [18, 19, 22, 23]
These discrepancies between evidence and practice regarding LBP workup and management illustrate a need for a systematic approach to measuring and evaluating characteristics of the examination, management, and treatment procedures of patients with LBP in health care settings. In the VHA system, care delivered by all privileged providers is assessed as part of an ongoing professional practice evaluation process. [6] This includes direct observation of providers’ professional competence and routine chart review performed by peers within the same discipline. The VHA has developed clinical indicators to guide chart review, with some being applicable to all disciplines and others specific to given disciplines. Although this process is suitable for assessing a given provider's performance, it has several limitations that make it unusable for national LBP care quality assessment. For example, the accuracy and reliability by which various providers review peers’ charts have not been evaluated, the chart review elements may not go into specific detail of LBP care, and there is currently no existing process to aggregate the assessment of all providers in the system.
Therefore, developing a uniform, scalable method of assessing LBP care quality in the VHA could have important policy and subsequent practice implications. VHA national electronic health records (EHR) contain rich data that can be analyzed to assess care quality. [24] Thus, the objective of this study was to implement a framework for assessing components of LBP care quality in VHA chiropractic visits using EHR data and present initial results from a systemwide application of that framework.
Methods
This study is part of a larger quality improvement project assessing elements of VHA chiropractic care using administrative data obtained from structured queries of VHA's Corporate Data Warehouse and manual EHR chart review (Figure 1). Using simple random sampling, we identified 1000 on-station (care delivered at VHA facilities by VHA providers) VHA chiropractic initial visits occurring in fiscal year 2018 (October 1, 2017, to September 30, 2018). The sample was limited to patients with no such chiropractic visits in the 12 months prior to the index (initial) visit date. Chiropractic visits were identified using Stop Code 436 in the primary or secondary position. All VHA facilities with on-station chiropractic clinics were eligible for inclusion. Data and related documentation were provided by the Office of Analytics and Performance Integration under the Office of Quality, Safety and Value, Department of Veterans Affairs.
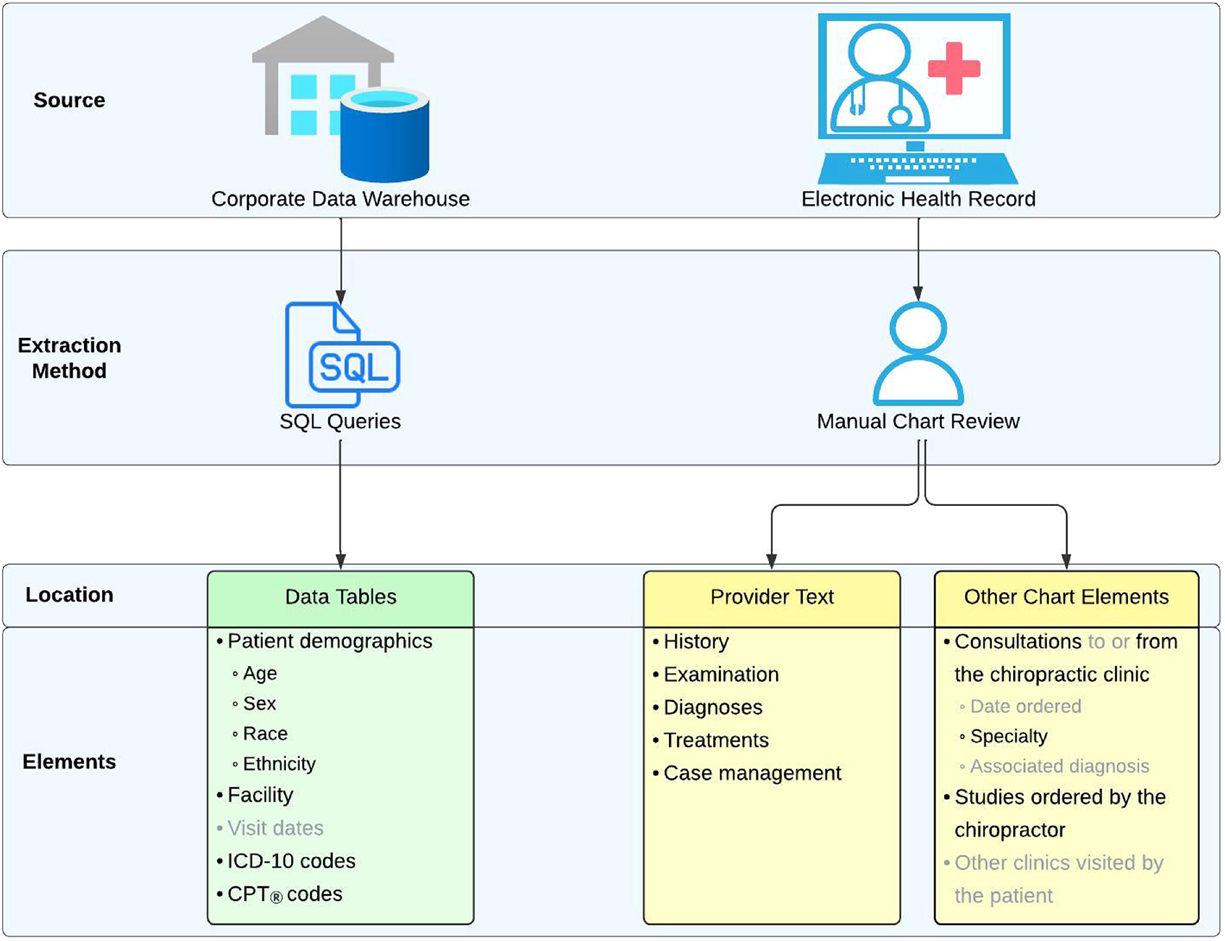
Figure 1
Figure 1. Variables and data sources. This figure includes all variables abstracted as part of the larger project. Variables relevant to this study are listed in black text. CPT, Current Procedural Terminology; ICD-10, International Classification of Diseases 10th Revision; SQL, Structured Query Language.
A team of investigators (S.E.G. and A.J.L.) with >30 years collective experience in clinical chiropractic care and VHA systems identified the clinical variables of interest. Through an iterative process, this team worked with subject matter experts from Quality Insights, Inc, Charleston, West Virginia, an independent External Peer Review Process contractor, to develop the chart abstraction tool. The chart review was conducted by Quality Insights, Inc registered nurses, registered health information administrators, or registered health information technicians. Reviewers abstracted key variables from the free-text documentation and broader EHR elements of each chiropractic visit. The chart abstraction process was piloted on a sample of 60 patients, and the investigator team determined the results captured the intended clinical variables.
Ethics
The Veterans Affairs Connecticut Healthcare System's Research Office determined that this was a quality improvement project and thus did not require institutional review board review.
LBP Care
We defined LBP visits as those including at least 1 LBP diagnosis (with or without radiculopathy) as the primary complaint in the chiropractors’ free-text documentation. We defined LBP care as the evaluation, management, and/or therapeutic services documented in the free text note and/or accompanying Current Procedural Terminology (CPT) codes. Operational definitions for each of the treatments examined are described in the Supplementary Table.
LBP Care Quality
We examined LBP care quality in a stepwise approach. First, all LBP visits were assessed for the presence of 3 history and examination quality indicators identified from previously published literature by Ramanathan et al: documentation of medical history, physical examination, and neurologic examination. [11] Ramanathan et al did not specifically detail what qualifies as successful documentation of medical history nor physical examination. [11] As such, we created operational definitions for these indicators, which are described in the Supplementary Table. We postulated that these 3 quality indicators should be included in all initial LBP visits, irrespective of the chronicity of the underlying complaint or whether the chiropractor provided any treatment and/or management services at that visit.
Next, we identified those visits in which both chronicity of complaint and some treatments were documented in the free-text and/or CPT codes. Chronicity was defined as acute (<4 weeks), subacute (4–12 weeks), and chronic (>12 weeks). [13] We categorized treatments as “recommended” or “no recommendation” based on the American College of Physicians (ACP) CPG for noninvasive treatments for acute, subacute, and chronic LBP. [13] The ACP guideline does not specify what qualifies as spinal manipulation, nor does it have any mention of manual mobilization. As such, we classified manual mobilization as “no recommendation.” While the article by Ramanathan et al does include quality indicators related to the treatment provided to LBP patients, we chose to classify treatment options based on the ACP CPG because the treatment recommendations therein were more comprehensive than the Ramanathan et al article. [11, 13]
Finally, we tabulated visits including the presence of all 3 history and/or examination quality indicators, those with at least 2 recommended treatments, and those with both. We defined visits, including both to be “high-quality.” Provision of treatments classified as “no recommendation” did not exclude such visits from being “high-quality” nor count against these visits in any way.
Risk of Bias
We used simple random sampling of charts to avoid selection bias. To ensure completeness of data, we excluded cases where complete data were not available. To minimize selective reporting bias, all outcomes measured in the study were included in the manuscript, regardless of their direction or significance.
Statistical Analysis
The demographic and disease characteristics pertaining to all LBP visits were summarized as counts and percentages for categorical variables and as means with SDs for continuous variables. These analyses were done using Microsoft Excel. [25] Subsequently, an exploration of the association between demographic and clinical characteristics and LBP visits that adhered to all 3 predefined history and examination indicators was conducted, utilizing generalized linear mixed models (GLMM), with the facility serving as the random effect. Lastly, in chronic visits where treatment was administered, the interplay between variables of interest and visits that offered 2 or more recommended treatments and met the criteria for being classified as high-quality visits was analyzed by adding an interaction term to the GLMM. All GLMM analyses were executed using the R Statistical Software (version 4.2.2; R Foundation for Statistical Computing). [26]
Results
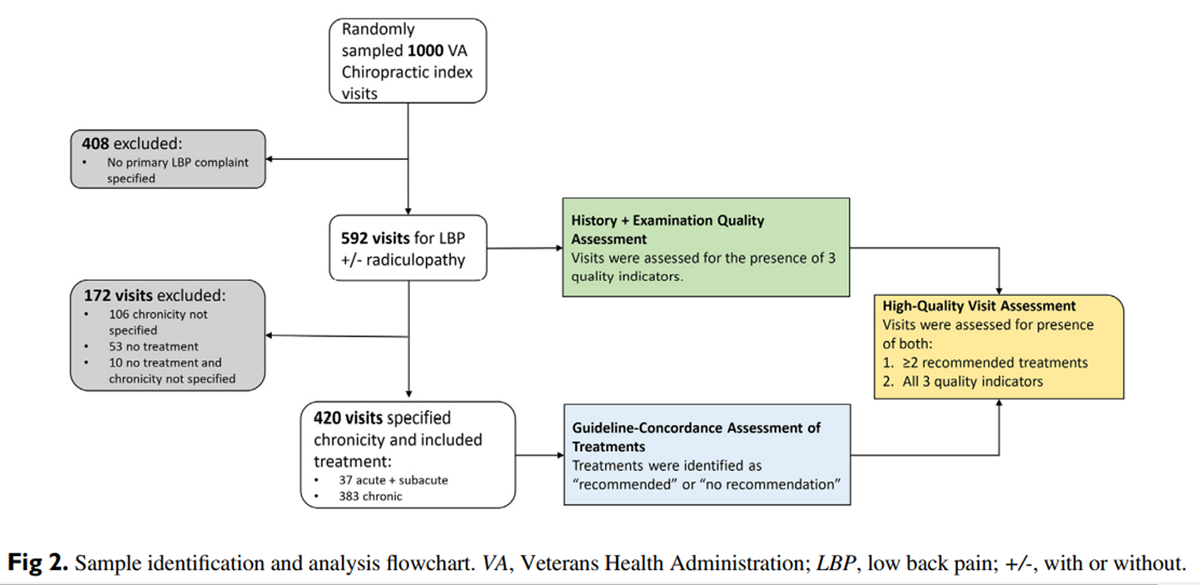
Figure 2

Table 1
Page 5One thousand initial chiropractic visit records were identified originating from 69 of the 105 VHA facilities providing on-station chiropractic care during the study timeframe. The median count of records per facility was 12 (range, 1–53). Of the 1000 initial chiropractic visit records, 592 included a primary complaint of LBP with or without radiculopathy. Among those 592 visits, 420 contained documentation that specified complaint chronicity and delivery of any treatment (Figure 2).
Demographics and frequencies of extracted variables are reported in Table 1. Male patients accounted for 505 (85%) of all LBP initial visits within our study. The racial composition of patients in these visits was 71% White, 19% Black or African American, and 9% other. The mean age of participants was 53 (SD = 16) years.
History and Examination Indicators
In all LBP index visits (N = 592), physical examination was documented in 454 (77%), medical history in 448 (76%), and neurologic examination in 371 (63%). At least 1, at least 2, and all 3 indicators were present in 87%, 73%, and 54% of visits, respectively.
Treatments

Table 2
Page 6Acute and/or subacute and chronic LBP treatment frequencies are shown in Table 2. Any type of manipulation (high-velocity low-amplitude, drop-assisted, flexion-distraction, sacro-occipital technique, and impulse instrument) was delivered in 92% of acute and/or subacute and 75% of chronic visits. Disease-specific advice and/or education was given in over half of acute and/or subacute (54%) and chronic (69%) visits. Therapeutic exercise was delivered more commonly in chronic visits (40%) than acute and/or subacute visits (35%), whereas manual soft tissue therapy was delivered more commonly in acute and/or subacute visits (56%) than chronic (32%).
High-Quality Visits
Of the 37 acute and/or subacute visits, 21 (57%) contained all 3 history and examination indicators, 31 (81%) contained 2 or more recommended treatments, and 21 (57%) contained both, meeting our definition of high-quality. Of the 383 chronic visits, 211 (55%) contained all 3 history and examination indicators, 267 (70%) contained 2 or more recommended treatments, and 151 (39%) contained both, thus meeting our definition of high-quality.
Associations Between Outcomes and Variables of Interest

Table 3
Page 7Generalized linear mixed models found no significant associations between demographic and clinical variables of interest and visits including 2 or more recommended treatments. Similarly, no significant associations were found between variables of interest and visits meeting all 3 history and examination indicators. Female patients were significantly less likely than male patients to have a high-quality visit (odds ratio, 0.52; 95% CI, 0.27–0.95; P = .032). Additionally, patients with a comorbid neck pain diagnosis were less likely than those without a neck pain diagnosis to have a high-quality visit (odds ratio, 0.56; 95% CI, 0.33–0.93; P = .024). All other associations between variables of interest and visits meeting high-quality criteria were statistically nonsignificant (P > .05) (Table 3).
Discussion
This study presents a systematic framework, developed using published literature, for assessing LBP care quality in VHA chiropractic index visits using EHR data and preliminary results from our testing of that framework. Developing a uniform, scalable method of assessing care quality can have important policy and practice implications. In a large system like VHA, scalable solutions are facilitated by automation, which, in turn, is facilitated by maximizing the quality and quantity of structured data (via improvements in clinical documentation capture) and refining the application of computational processes, such as natural language processing and machine learning. Such innovations are being explored, and the results of our project can help inform ongoing efforts in automation. [27]
The results of our study also provide an initial benchmark of LBP care quality in VHA chiropractic visits. All 3 of our history and examination indicators were present in 54% of initial LBP visits. A 2017 scoping review found that in chiropractic care across all conditions, a complete patient history was taken in 31% of patient visits, and neurologic examinations were performed in 64.6% of visits. [28] A retrospective medical record review of Australian general practitioner, chiropractic, physiotherapy, and specialist physician LBP patient visits found physical examination to be documented in 87%, medical history in 94%, and neurologic examination in 63% of visits. [11]
We created our quality indicators and treatment classifications based on work from Ramanathan et al and the ACP CPG because these publications more comprehensively aligned with the aims of our study compared to other guidelines. For the purposes of our study, high-quality visits had to include documented delivery of 2 or more recommended treatments. We chose this criterion because VHA chiropractic care typically includes multiple therapies, and CPGs recommend multiple non-pharmacologic interventions within the scope of chiropractic care (eg, advice and/or education, spinal manipulation) for patients with LBP. [20, 29–31] Therefore, we thought it likely that a high-quality initial chiropractic visit would include delivery of 2 or more recommended treatments. It should be noted, however, that it may not always be necessary or appropriate to provide 2 or more recommended treatments during an initial chiropractic visit.
Any spinal manipulation was the most frequently provided intervention in both acute and/or subacute (92%) and chronic (75%) LBP initial visits in our study. Although CPGs consistently recommend practitioners provide advice and/or education for patients with LBP, disease-specific advice and/or education was provided in 54% of acute and/or subacute and 69% of chronic visits. [13, 29, 30] One previous study evaluated the guideline concordance of chiropractic treatments in patients with LBP across a care plan in a teaching clinic. [19] In this study, 98.8% of acute and 100% of patients with chronic LBP received spinal manipulation and/or mobilization, 50.6% of acute and 44.7% of chronic patients received education and/or advice, 48.1% of acute and 48.0% of chronic received exercise, and 87.5% of acute received soft tissue therapy, all of which met their definition of recommended treatments. We are aware of no other study that has assigned a quality rating to individual chiropractic LBP visits based on history and/or examination and treatment procedures.
None of the acute and/or subacute visits identified in our sample included female patients. Our analysis of chronic LBP visits found female patients to be significantly less likely than male patients to have a high-quality visit. It is unclear from the findings of this study why female sex was less likely to be associated with a high-quality visit. Prior work from one VHA medical center demonstrated improved outcomes for female veterans managed by chiropractors for both neck and back pain. [32, 33] Nonetheless, this finding warrants further investigation as female veterans are among the fastest growing populations of VHA users, and VHA chiropractic clinics have a higher proportion of female patients than the general VHA enrollee population. [8, 34, 35]
We also found patients with neck pain (with or without radiculopathy) comorbid diagnoses to be significantly less likely to have a high-quality visit. The results from our study do not provide definitive conclusions as to whether patients with neck pain comorbid diagnoses receive lower quality care or if visits including patients with this diagnosis were low-quality visits and, therefore, a neck pain comorbid diagnosis was included appropriately or inappropriately.
Results from our novel framework illustrate several strengths of our approach. We were able to identify and extract structured data relevant to assessing care quality and implement a manual chart review process that identified and abstracted applicable free-text and other chart data. To measure quality, we developed a rating scale based on published evidence and successfully applied that scale to rate chiropractic visits using chart abstraction data.
We identified several areas for continued improvement in our framework. While we were able to assess the association between variables of interest and outcomes in chronic LBP visits using generalized linear mixed-effect models, we were unable to perform this analysis on acute and/or subacute visits due to a small sample size (n = 37). Future work could benefit from purposeful inclusion of a larger number of patient visits for acute and/or subacute LBP to better elucidate aspects of care in this population. Inclusion of additional elements of LBP care quality, such as screening for red flags and assessing appropriateness of ordered imaging, could also strengthen future quality assessments. Due to technical issues in the data collection process, we were unable to evaluate providers’ assessment of red flag indicators described by Ramanathan et al. [11] Additionally, we note that we did not use our framework to rate the performance of any individual chiropractor. Our results are exploratory of a process and not part of the existing quality assurance measures for VA chiropractors. Lastly, our framework could be improved by evaluating the quality of LBP care throughout an entire care plan.
Limitations
Retrospective chart analyses rely upon the accuracy of clinicians’ EHR documentation. As such, some data may not accurately capture the care that occurred during visits. The provider text note was used when determining chronicity of complaint and assessing history and examination procedures. However, provider text, CPT codes, or both were used when determining LBP care procedures that occurred during visits. Future work should be consistent with using either approach.
Due to our data being limited to index LBP chiropractic visits, we could not account for treatments that may have been delivered at subsequent visits. We did not attempt to assess care plan quality based on frequency and duration of visits; however, recommendations for these aspects of care are not made in many LBP CPGs. [13, 20, 30] The treatment classifications used in this project are based on a single CPG, while multiple CPGs for the treatment of LBP exist. Existing research suggests some homogeneity exists across international guidelines for non-pharmacologic care of LBP, [29] yet any approach to assess care quality must be agile to adapt as new recommendations emerge. We created operational definitions to characterize documentation of the history and examination quality indicators and treatment classifications that have been described in the literature; however, our definitions may differ from some sources.
We used simple random sampling to identify on-station chiropractic index visits without consideration of chiropractic clinic size or number of cases per facility. Sampling could be improved by weighting by chiropractic clinic characteristics. Finally, the external validity of our exploratory approach to assessing LBP care quality in VHA chiropractic visits is unknown. While we used a CPG and previous publications to develop the present framework, this approach may not be generalizable to other health care systems.
Future Studies
Additional work is needed to refine an approach to LBP quality assessment using national EHR data. In addition to items mentioned previously, future work should assess aspects of LBP care quality across an entire episode of care rather than at index visits alone. Also, future assessments of care quality should be expanded to evaluate management of other conditions commonly seen by VHA chiropractors.
Conclusion
This study explored a systemwide process for assessing components of LBP care quality using EHR data from VHA index chiropractic visits. Our work provides a potential framework for uniform assessment of care quality in VHA chiropractic visits for LBP and highlights potential areas for improvements in LBP care quality assessments.
Practical Applications
Our study found that it was possible to create a framework for assessing care quality in Veterans Health Administration chiropractic visits for low back pain utilizing electronic health record data.
We developed an evidence-based approach to measuring quality and were able to apply quality ratings to individual chiropractic patient visits for low back pain.
This study highlights potential areas for improvement in care and the need for additional work to understand and optimize care delivery and quality analyses.
Appendix
Funding Sources and Conflicts of Interest
This material is based on work supported by the US Department of Veterans Affairs and the Interinstitutional Network for Chiropractic Research through a grant from the Palmer College Foundation. R.D.M. is a postdoctoral fellow supported by the Department of Veterans Affairs Office of Academic Affiliations and a grant from Parker University. S.E.G. is a postdoctoral associate supported by a grant from the NCMIC Foundation. No conflicts of interest were reported for this study.
Contributorship Information
Concept development (provided idea for the research): A.J.L, R.D.M., S.E.G.
Design (planned the methods to generate the results): R.D.M., A.J.L., A.R.S., S.E.G.
Supervision (oversight, organization and implementation): A.J.L., L.A.B., K.L.C.
Data collection/processing (experiments, organization, or reporting data): R.D.M., S.E.G., A.J.L., A.R.S.
Analysis/interpretation (analysis, evaluation, presentation of results): X.Z., R.D.M., A.J.L.
Literature search (performed the literature search): R.D.M., A.J.L.
Writing (responsible for writing a substantive part of the manuscript): R.D.M., A.J.L.
Critical review (revised manuscript for intellectual content): A.J.L., L.A.B., S.E.G., K.L.C.
References:
US Burden of Disease Collaborators.
The state of US health, 1990–2016: burden of diseases,
injuries, and risk factors among US states.
JAMA. 2018;319(14):1444–1472.Wu A, March L, Zheng X, et al.
Global Low Back Pain Prevalence and Years Lived with Disability from
1990 to 2017: Estimates from the Global Burden of Disease Study 2017
Annals of Translational Medicine 2020 (Mar); 8 (6): 299Dieleman JL, Cao J, Chapin A, et al.
US Health Care Spending by Payer and Health Condition, 1996-2016
JAMA 2020 (Mar 3); 323 (9): 863–884James SL, Abate D, Abate KH, et al.
Global, regional, and national incidence, prevalence, and years lived with
disability for 354 diseases and injuries for 195 countries and territories,
1990?2017: a systematic analysis for the Global Burden of Disease Study 2017.
Lancet. 2018;392(10159):1789–1858.Goulet JL, Kerns RD, Bair M, et al.
The musculoskeletal diagnosis cohort: examining pain and pain care among veterans.
Pain. 2016;157(8):1696–1703.Department of Veterans Affairs.
VHA Directive 1190 Peer Review for Quality ManagementKligler B, Bair MJ, Banerjea R, et al.
Clinical policy recommendations from the VHA state–of–the–art conference
on non–pharmacological approaches to chronic musculoskeletal pain.
J Gen Intern Med. 2018;33(suppl 1):16–23.Lisi AJ, Brandt CA.
Trends in the Use and Characteristics of Chiropractic Services
in the Department of Veterans Affairs
J Manipulative Physiol Ther. 2016 (Jun); 39 (5): 381–386Burdick R, Corcoran KL, Zhao X, Lisi A.
The rate of use of Veterans Affairs chiropractic care: a 5–year analysis.
Chiropr Man Ther. 2022;30(1):4.Wiles LK, Hibbert PD, Stephens JH, et al.
What constitutes “appropriate care” for low back pain?: Point–of–care
clinical indicators from guideline evidence and experts
(the STANDING Collaboration Project).
Spine. 2022;47(12):879.Ramanathan SA, Hibbert PD, Maher CG, et al.
CareTrack: toward appropriate care for low back pain.
Spine. 2017;42 (13):E802-E809.Luther SL, Finch DK, Bouayad L, et al.
Measuring pain care quality in the Veterans Health
Administration primary care setting.
Pain. 2022;163(6):e715-e724.Qaseem A, Wilt TJ, McLean RM, Forciea MA;
Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain:
A Clinical Practice Guideline From the American College of Physicians
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 514–530Childs JD, Fritz JM, Wu SS, et al.
Implications of early and guideline adherent physical therapy
for low back pain on utilization and costs.
BMC Health Serv Res. 2015;15(1):150.Rutten GM, Degen S, Hendriks EJ, Braspenning JC, Harting J.
Adherence to clinical practice guidelines for low back pain in physical therapy: do patients benefit?
Phys Ther. 2010;90(8):1111-1122.Stevans JM, Delitto A, Khoja SS, et al.
Risk Factors Associated With Transition From Acute to Chronic
Low Back Pain in US Patients Seeking Primary Care
JAMA Network Open 2021 (Feb 1); 4 (2): e2037371Gaspar FW, Thiese MS, Wizner K, Hegmann K.
Guideline adherence and lost workdays for acute low back pain
in the California workers’ compensation system.
PLoS One. 2021;16(6): e0253268.Zadro J, O'Keeffe M, Maher C.
Do Physical Therapists Follow Evidence-based Guidelines When
Managing Musculoskeletal Conditions? Systematic Review
BMJ Open. 2019 (Oct 7); 9 (10): e032329Csiernik B, Smith A, Plener J, Tibbles A, Young JJ.
Intervention usage for the management of low back pain
in a chiropractic teaching clinic.
Chiropr Man Ther. 2022;30(1):3.George SZ, Fritz JM, Silfies SP, et al.
Interventions for the management of acute and chronic low back pain: revision 2021.
J Orthop Sports Phys Ther. 2021; 51: CPG1-CPG60Pangarkar SS, Kang DG, Sandbrink F, et al.
VA/DoD clinical practice guideline: diagnosis and treatment of low back pain.
J Gen Intern Med. 2019;34(11):2620-2629.Foster NE, Anema JR, Cherkin D, et al.
Prevention and Treatment of Low Back Pain:
Evidence, Challenges, and Promising Directions
Lancet. 2018 (Jun 9); 391 (10137): 2368–2383Buchbinder R, van Tulder M, Öberg B, Costa LM, Woolf A, at al.
Low Back Pain: A Call For Action
Lancet. 2018 (Jun 9); 391 (10137): 2384–2388
This is the fourth of 4 articles in the remarkable Lancet Series on Low Back PainJustice AC, Erdos J, Brandt C, Conigliaro J, Tierney W, Bryant K.
The Veterans Affairs Healthcare system: a unique laboratory for observational and interventional research.
Med Care. 2006;44(8 suppl 2):S7-12.Microsoft.
Microsoft Excel Spreadsheet Software
Microsoft 365. Available at:
https://www.microsoft.com/en-us/microsoft-365/excel
Accessed February 28, 2023.R Foundation.
The R Project for Statistical Computing.
Available at: https://www.r-project.org/
Accessed February 28, 2023.Coleman BC, Fodeh S, Lisi AJ, et al.
Exploring supervised machine learning approaches to predicting
Veterans Health Administration chiropractic service utilization.
Chiropr Man Ther. 2020;28(1):47.Beliveau PJH, Wong JJ, Sutton DA, et al.
The Chiropractic Profession: A Scoping Review of Utilization Rates,
Reasons for Seeking Care, Patient Profiles, and Care Provided
Chiropractic & Manual Therapies 2017 (Nov 22); 25: 35O’Connell NE, Cook CE, Wand BM, Ward SP.
Clinical guidelines for low back pain: a critical review of
consensus and inconsistencies across three major guidelines.
Best Pract Res Clin Rheumatol. 2016;30(6):968-980.National Institute for Health and Care Excellence (NICE):
Low Back Pain and Sciatica in Over 16s:
Assessment and Management (PDF)
NICE Guideline, No. 59 2016 (Nov): 1–1067Halloran SM, Coleman BC, Kawecki T, Long CR, Goertz C, Lisi AJ.
Characteristics and practice patterns of U.S. Veterans Health Administration
doctors of chiropractic: a cross-sectional survey.
J Manipulative Physiol Ther. 2021;44(7):535-545.Corcoran KL, Dunn AS, Green BN, Formolo LR, Beehler GP.
Changes in Female Veterans' Neck Pain Following
Chiropractic Care at a Hospital for Veterans
Complement Ther Clin Pract. 2018 (Feb); 30: 91–95Corcoran KL, Dunn AS, Formolo LR, Beehler GP.
Chiropractic Management for US Female Veterans With Low
Back Pain: A Retrospective Study of Clinical Outcomes
J Manipulative Physiol Ther. 2017 (Oct); 40 (8): 573–579Yano EM, Hayes P, Wright S, et al.
Integration of women veterans into VA Quality improvement research efforts: what researchers need to know.
J Gen Intern Med. 2010;25(suppl 1):56-61.Graham S, Coleman B, Zhao X, Lisi A.
Evaluating rates of chiropractic use and utilization by patient sex
within the United States Veterans Health Administration:
a serial crosssectional analysis.
Chiropr Man Ther. 2023;31(1):29.
Return to LOW BACK PAIN
Return to CHIROPRACTIC CARE FOR VETERANS
Since 12-27-2023


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |