

Chiropractic This section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Primary Care 2002 (Jun); 29 (2): 419–437 ~ FULL TEXT
OPEN ACCESS Simon Dagenais, DC, PhD, Scott Haldeman, DC, MD, PhD, FRCP(C)
Irvine Chiropractic,
17101 Armstrong #101,
Irvine, CA 92614, USA.Chiropractic is now more than a century old, and it is licensed throughout the United States and Canada and recognized in more than 60 countries worldwide. Doctors of Chiropractic receive training that is focused on the treatment of NMS conditions through manual and physical procedures, such as manipulation, massage, exercise, and nutrition. Most patients present to chiropractors with low back pain, neck pain, whiplash, and headaches. Numerous studies and expert panel reviews have supported the use of chiropractic and manipulation for these complaints. Satisfaction with chiropractic care for low back pain typically is good. Chiropractic, in general, offers safe and cost-effective procedures for selected musculoskeletal problems.
From the Full-Text Article:
Background
A century after it was founded, chiropractic is now the largest alternative health profession, with more than 52,000 practitioners in the United States. [1, 2] Most chiropractors view themselves as neuromusculoskeletal (NMS) specialists and choose to focus their practice on the treatment of muscle and joint pain. Evidence is growing to support the use of chiropractic and spinal manipulation, the treatment most associated with chiropractic, for a variety of conditions such as low back pain, neck pain, whiplash, and headaches. [3–9] The exact mechanism of action of manipulation is unknown, but numerous theories have been proposed and are currently the subject of ongoing research. Relationships between primary care physicians and chiropractors have been improving steadily since the days when it was considered unethical by the American Medical Association for physicians to refer patients to chiropractors. The goal of this article is to provide a brief overview of chiropractic for the primary care physician to increase his or her understanding of the current status of chiropractic. The article includes a discussion of the history of chiropractic, its educational requirements, its pertinent legislation, and its use; a brief explanation of its treatment principles; and a review of the literature concerning the effectiveness, cost-effectiveness, and safety of chiropractic and manipulation for commonly treated conditions.
Historical perspective
The word chiropractic was derived from the Greek words cheir and praktos to designate a treatment done by hand. The profession of chiropractic generally is considered to have been founded in 1895 by a magnetic healer named D.D. Palmer after his positive experiences with manipulation of the spine. Through further practice and studies, he became convinced that this method of treatment was of benefit and devoted his life to developing the art and science of chiropractic. Palmer founded the first college of chiropractic (now Palmer University in Davenport, Iowa), wrote numerous textbooks on chiropractic, was a promoter of the discipline, and trained his son, B.J. Palmer, to eventually broaden the appeal of the profession.
Chiropractic burgeoned in the early 1900s at a time when traditional health care left much to be desired, and many professions such as homeopathy, naturopathy, and magnetic healing were attempting to become established. Although many if its theories were controversial, chiropractic was able to thrive in this environment by providing an effective, safe, and lowcost method to relieve common NMS complaints, often with immediate results. As the number of practitioners grew, legislative efforts were made to suppress chiropractic, resulting in the arrest of practitioners in the 1920s and 1930s based on charges of practicing medicine without a license.
The landscape for interaction between medical physicians and chiropractors changed in 1975 after a workshop on “The Research Status of Spinal Manipulative Therapy” by the National Institute of Neurological and Communicative Diseases and Stroke was convened in Bethesda, Maryland. [10] This event was one of the first professional conferences attended by physicians and chiropractors, and it became obvious that cooperative research was necessary to define the role of spinal manipulation as a treatment approach. This cooperation became a reality after the 1987 ruling of the US Court of Appeals in Illinois in the Wilk v American Medical Association (AMA) lawsuit. A group of chiropractors launched this suit under the Sherman Antitrust Act, alleging that the AMA and other medical associations had conspired illegally against chiropractic by forbidding its members to associate with them and disseminating mistruths about the dangers of chiropractic. The court ruled against the AMA and ordered it to pay restitution to chiropractic associations, amend its policies regarding chiropractic, and publicly renounce its former views. [11]
Shortly after this verdict, public and medical perception of chiropractic began to change. One symbol of the newfound spirit of cooperation between chiropractic and other health professions was the foundation of the American Back Society, whose members included primary care physicians, orthopedists, neurologists, physical therapists, and chiropractors. Other professional groups, such as the North American Spine Society, the International Society for the Study of the Lumbar Spine, and the American Public Health Association, followed suit by admitting chiropractors as members. This participation of chiropractors in major medical societies has led to the further integration of chiropractic into the scientific community. During this period, the first peer-reviewed scientific journal devoted to chiropractic and manual medicine, the Journal of Manipulative and Physiological Therapeutics, was included in Index Medicus, ensuring a presence for chiropractic research in the scientific literature.
Education
The Council on Chiropractic Education (CCE) is licensed by the US Secretary of Education to maintain accreditation standards for chiropractic education institutions. Currently, there are 15 accredited institutions in the United States, all of which are private, independent colleges or universities. The Florida legislature recently voted to establish a chiropractic program within the Florida State University system, which, if instituted, would be the first government-sponsored program in the United States.
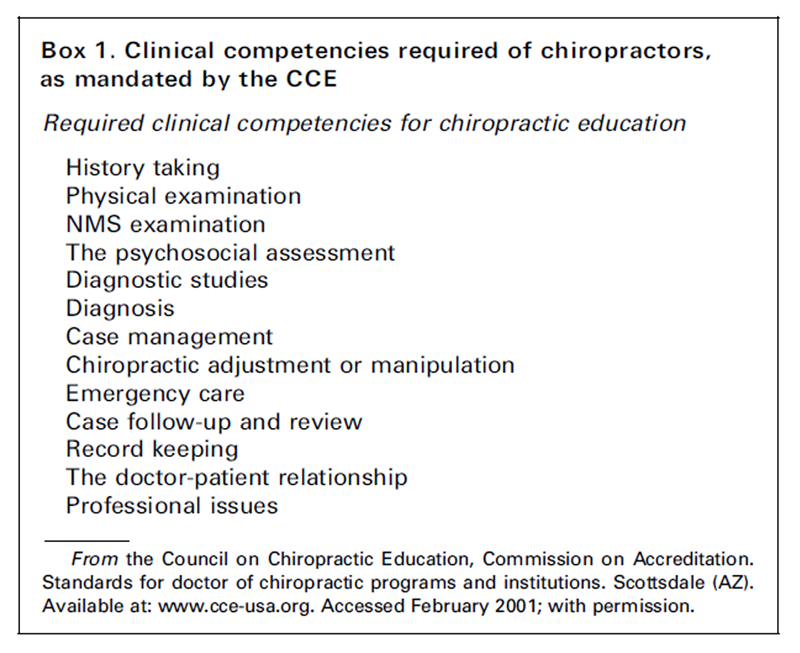
Box 1 Educational requirements for chiropractors are similar to those of other health professions. Current prerequisites for admission to chiropractic education include a minimum of 90 credits of undergraduate education, with a minimum of six credits in chemistry, organic chemistry, biology, and physics, and additional requirements in social sciences or humanities, communication or language skills, and psychology. Standards may soon be raised to include a bachelor’s degree before entry into the program; surveys of the profession indicate that approximately 40%to 50% of chiropractors had a college degree before beginning their chiropractic education. [12, 13] The structure of chiropractic education is similar to medical education with classroom education in basic and clinical sciences and supervised practical clinical training in academic health centers. The curriculum must include at least 4,200 hours of instruction and must teach the clinical competencies outlined in Box 1.
One study of medical and chiropractic education programs concluded that both were comparable in their approaches to basic sciences and somewhat comparable in clinical sciences. [4] The main differences were noted in the quantity of practical clinical training, which was much more comprehensive in the education of medical physicians. Chiropractic training places a greater emphasis on examination and treatment of spinal disorders, with only superficial training in pharmacology and no training in surgery. Internship occurs before graduation, and there are no postgraduate residency requirements. Many new graduates undergo informal apprenticeships with more experienced practitioners before opening a private practice. Specialized training through part-time studies or 3–year residencies is also available in orthopedics, radiology, sports medicine, rehabilitation, and other disciplines.
Licensure
Chiropractic is licensed in all 50 states in the United States and all provinces in Canada. To gain licensure, chiropractors must graduate from a CCE-accredited institution and successfully complete a series of national examinations administered by the Federation of Chiropractic Examination Boards. The first three written examinations cover the basic and clinical sciences, whereas for the fourth examination, a candidate must complete a patient encounter successfully (i.e., obtaining a clinical history, performing a physical examination, establishing a diagnosis, interpreting radiologic and laboratory findings, and delivering an appropriate treatment plan). Individual states may require additional examinations, usually on topics such as jurisprudence; most states require continuing-education credits to maintain a license.

Table 1 Chiropractic rapidly is gaining acceptance internationally and currently is practiced in more than 60 countries. The international division of the CCE has given accreditation to two institutions in Canada, two in Australia, and three in Europe (one in England, one in France, and one in Denmark); several other international chiropractic institutions have applied for CCE accreditation. Chiropractic is recognized in many countries throughout the world, whether through official legislation or de facto recognition, as indicated in Table 1.
Use
A 1998 study by Eisenberg et al. [14] reported that 42.1% of the population had used at least one alternative therapy in the past 12 months, and that 11.1% had seen a chiropractor, making it the most commonly used alternative medicine practice. Several studies show that chiropractic is the most frequently used form of alternative medicine. [15–18] Estimates on the use of chiropractic in the general population range from a low of 3.3% [17] to a high of 18%. [16] These discrepancies are likely attributable to methodologic differences and sample selection. It seems reasonable to estimate that approximately 10% of the general population visits a chiropractor each year. The most common conditions cited in these studies for which chiropractic care is sought include back pain, arthritis, headaches, neck problems, sprains or strains, chronic pain, and digestive problems. [14, 15] A study found that chiropractic was the third most common source of care for patients with low back pain (sought by 30.8% of such patients), after general practitioners (58.6%) and orthopedists (36.9%). [19] Use of chiropractors was highest in the western United States, where 44.6% of those with low back pain sought their services, as compared with 29.5% in the South.
Commonly treated conditions
In 1991, Shekelle and Brook [8] reported that 42.1% of visits to chiropractors were for low back pain and that 10.3% were for neck or face pain. Hurwitz et al. [20] reported that 68% of chiropractic patients sought care for low back pain, whereas Manga et al. [21] reported that approximately 95% of chiropractic practice in Ontario, Canada, is for NMS conditions. A recent study examined the nature of presenting complaints for 7,527 patients reporting to 161 chiropractors who observed a greater-than-average number of non-NMS conditions in the United States and Canada. [13] The largest group of patients was those seeking care for back pain (46.0%), followed by neck pain (12.7%), shoulder pain (5.5%), and nonmigraine headaches (4.8%). Few patients presented with non-NMS conditions such as gastrointestinal symptoms (1.1%), upper respiratory tract infections (0.9%), allergies (0.7%), migraines (0.6%), and sinus pain (0.6%). A small group of patients (5.1%) was seeking preventive, or maintenance care, which is encouraged by certain chiropractors on the assumption that periodic chiropractic treatment may have a prophylactic effect against spinal disorders. At this time there is no convincing evidence to support the use of spinal manipulation as a preventive therapy. Chiropractors commonly also offer other preventive care services, including smoking cessation, weight loss programs, fitness counseling, and stress management. [13]
Chiropractic clinical practice
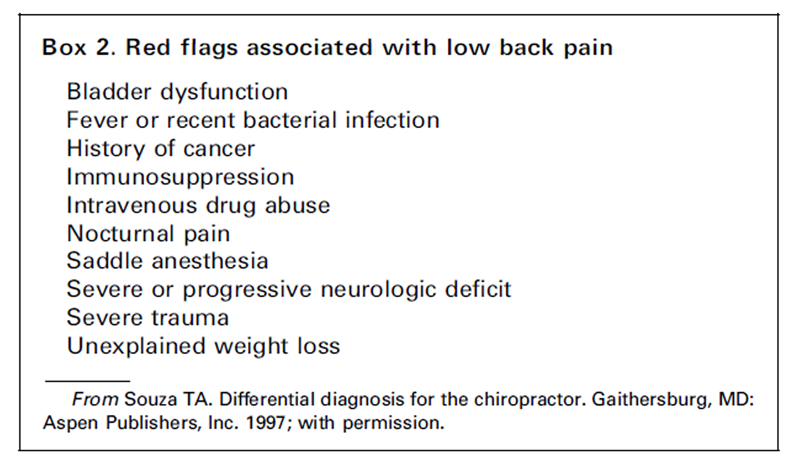
Box 2 The procedure followed by chiropractors for evaluating a new patient is much the same as that followed by any other physician. When patients present to a chiropractor for their initial visit, the chiropractor is likely to obtain a history of the presenting complaint, including its mechanism of injury or onset, provocative or palliative factors, quality and severity of pain, and a review of systems and significant medical conditions. The chiropractic physical examination, however, tends to focus more on the spinal examination than the general physical examination performed by a primary care medical physician. It may include some form of postural assessment, range-of-motion studies, inspection and palpation of affected areas, muscle strength testing, orthopedic provocation testing, and neurologic screening of dermatomes, myotomes, and deep tendon reflexes. In the presence of risk factors or so-called red flags (Box 2), radiologic or other diagnostic examinations may be performed or ordered by a chiropractor. Chiropractors also may order radiographs for all patients to assess the structural integrity of the skeleton and for biomechanical analysis of vertebral relationships before administering treatment.
Unique to the chiropractic experience is the practice of spending as much as 60 to 90 minutes examining a patient and then explaining the results of the examination, the working diagnosis, the proposed treatment plan, and providing general education about chiropractic. This encounter is considered one of the most important aspects of chiropractic practice and is emphasized throughout chiropractic education. In fact, one review of chiropractic commented that “chiropractic’s most important contribution may have to do with the patient-physician relationship”. [22] Communicating in simple language is believed to help the patient understand his or her condition and how chiropractic can help treat it. The practitioner also outlines the benefits of continuing with treatment beyond the acute phase and beginning some form of rehabilitative treatment to prevent further occurrences. Once discharged, patients are nevertheless encouraged to seek care if their symptoms recur.
Satisfaction with care
The amount of time spent with patients and the perceived interest in their problems may account for the high rates of satisfaction typically associated with chiropractic care. [23–26] A 1989 study examined the satisfaction of 457 patients in a health maintenance organization who received care for their low back pain from either a medical physician or a chiropractor. [23] Although patient populations were similar for both groups, significant differences were noted in the percentage of patients who reported being very satisfied with their care (66% for chiropractors versus 22% for medical physicians). Chiropractors scored significantly higher in providing sufficient information about the cause of pain (53% versus 17%), giving a clear idea about recovery time (44% versus 16%), and using a model or chart to explain the cause of pain (80% versus 27%).
Theories of manipulation
Box 3
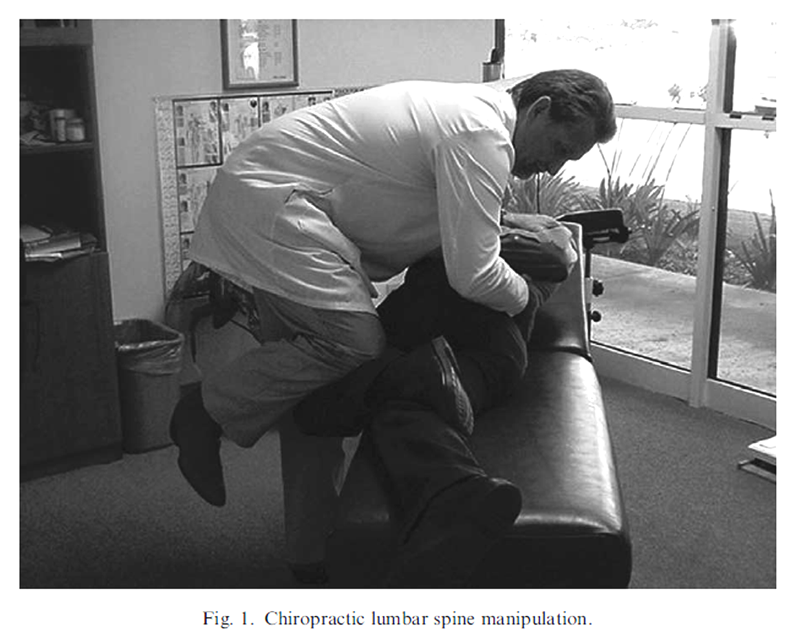
Figure 1
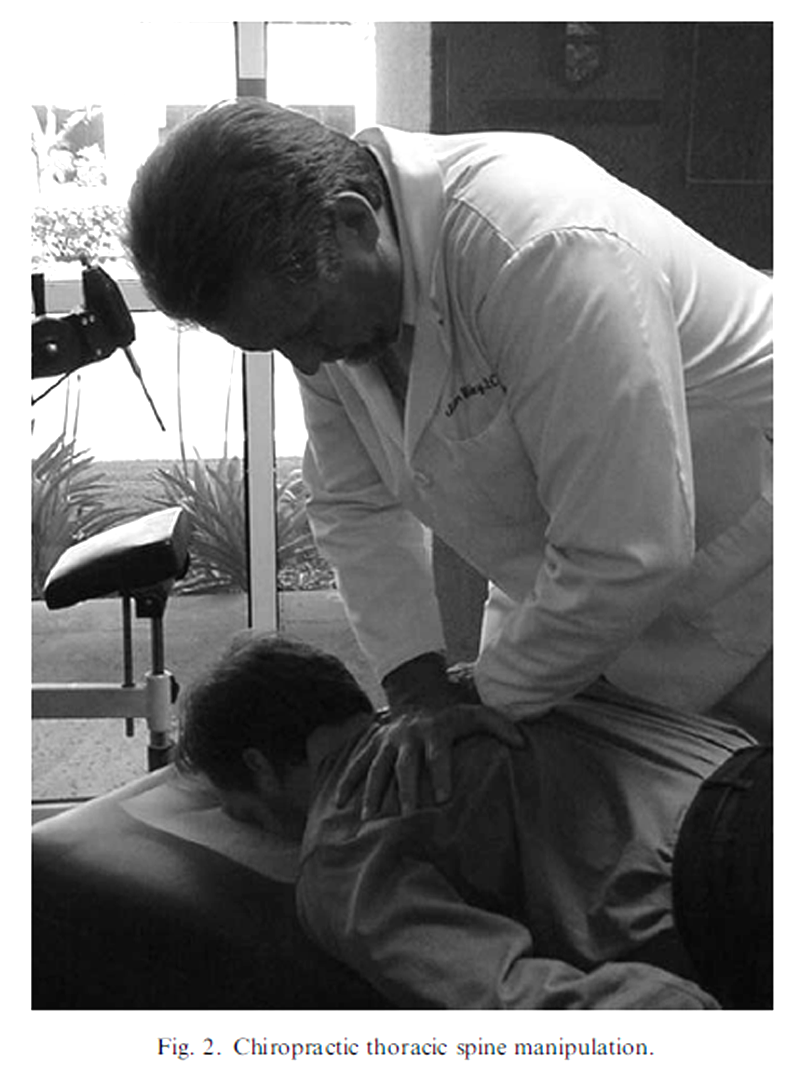
Figure 2
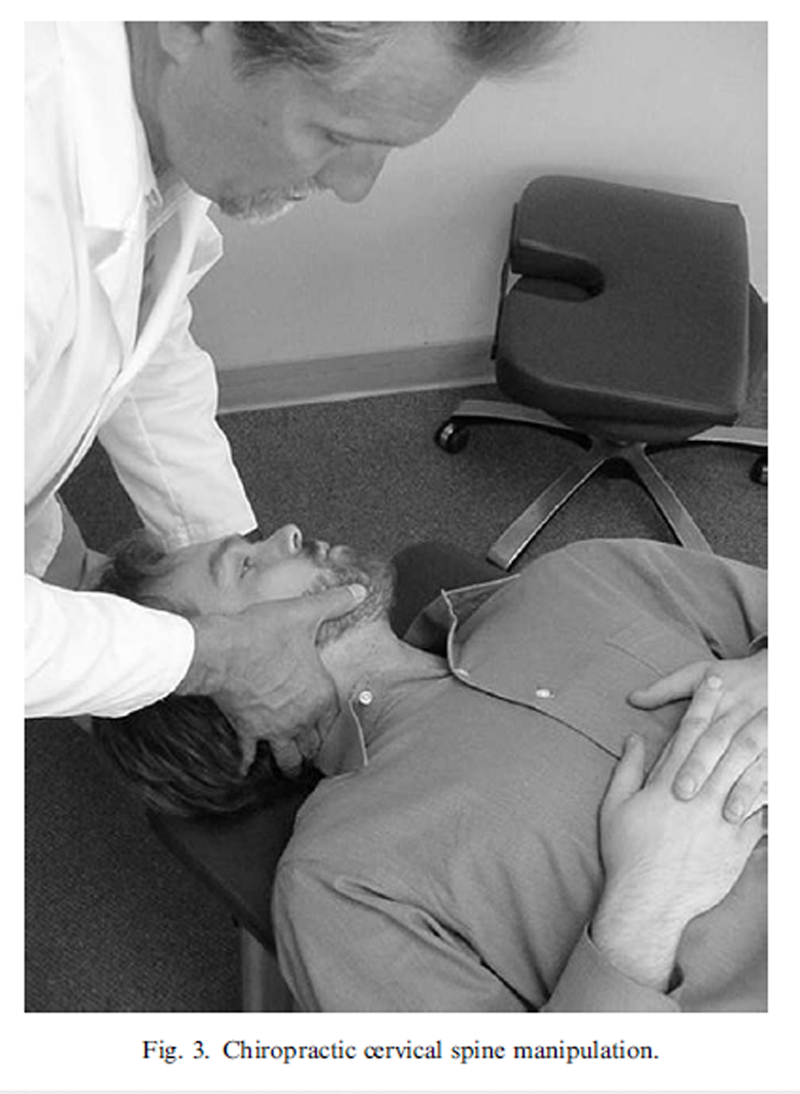
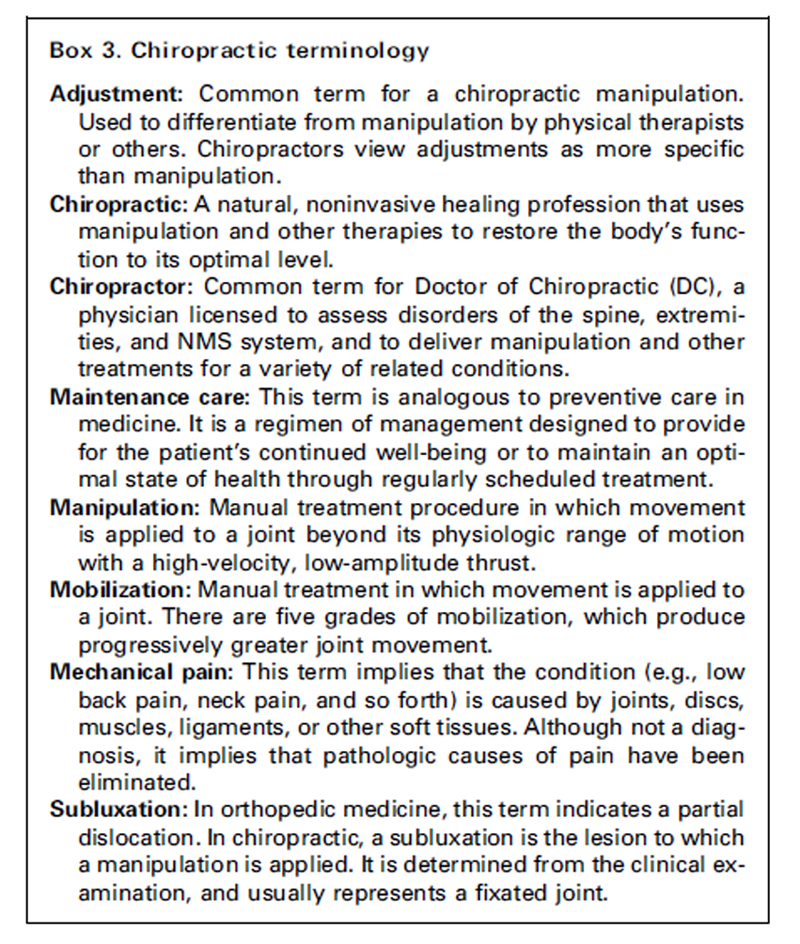
Figure 3 Spinal manipulation has been practiced for thousands of years. Hippocrates is quoted as saying “ in all disease look first to the spine,” and evidence is mounting that manipulation can be safe and effective for a variety of conditions. Its mechanism of action, however, is largely unknown. Early theories explained the effect of the adjustment (see Box 3 for terminology) as re-establishing a normal flow of vital energy within the body that had been impaired by a misalignment of a vertebra impinging the nerve root or spinal cord. [27]
More modern theories include both biomechanical and neurophysiologic models. Biomechanics experts who have studied manipulation postulate that fibrous adhesions within joints may be broken by the forceful thrusting, thus increasing the range of motion of a joint. [28, 29] This notion is supported by evidence that the pop or crack that commonly follows a spinal manipulation is associated with the accumulation of gas within a peripheral joint and usually results in increased range of motion of that joint. [30, 31] Another biomechanical theory suggests that manipulation releases small tags from the joint capsule that might be entrapped within the joint. [32] Neurophysiologists, on the other hand, attempt to explain the effect of manipulation by measuring direct stimulation of joint mechanoreceptors and the resulting reflex muscle contraction followed by relaxation of paraspinal muscles. [33]
There is also some evidence that manipulation can modulate central nervous system excitability, at least during the immediate postmanipulation period, as measured by changes in evoked H-reflexes. [34] The recording of visceral reflex and organ function changes on stimulation of spinal somatic receptors is being studied as a possible explanation for claimed effects of spinal manipulative and manual treatments on certain functional visceral disorders, such as infantile colic and premenstrual syndrome. [35] Ongoing research should begin to unravel the physiologic effects of manipulation in the near future.
There are many different types of manipulation techniques that can be adapted according to practitioner or patient preference and the specific condition being treated. Some of the most common methods of applying spinal manipulation are shown in Figs. 1–3.
Review of the clinical literature
The clinical literature evaluating spinal manipulation and chiropractic for the treatment of low back pain, neck pain, headaches, and a few non-NMS conditions has grown steadily during the past two decades. It is no longer possible to review each of these trials in a general discussion of chiropractic. These studies, however, have been reviewed by a number of panels in government and private agencies. Most of these panels have been multidisciplinary, with the participation of chiropractors, primary care physicians, orthopedic and neurologic surgeons, methodologists, and epidemiologists. The purpose of these panels often was to evaluate the literature supporting all treatments available for the specific condition being investigated, and to then integrate this knowledge into evidence-based guidelines for clinicians, policy makers, and consumers. Systematic reviews of the literature and meta-analyses are also useful when evaluating a wide body of knowledge to identify trends. The conclusions of a number of expert panels and literature reviews examining the evidence in favor of spinal manipulation are summarized in the following sections.
Low back pain
A panel on the treatment of acute low back pain in adults that was sponsored by the Agency for Health Care Policy and Research, a branch of the US federal government, published its findings in 1994. [3] This panel of experts rated the evidence for various therapies in the treatment of low back pain. One of its recommendations was a 1–month course of spinal manipulation for patients with acute low back pain without radiculopathy. Manipulation was also a reasonable option for the treatment of sciatica, although less evidence was available for this condition. Several other guidelines have been published internationally, with similar findings. In Denmark, guidelines recommended manipulation for acute low back pain of greater than 2 to 3 days’ duration and for acute exacerbation of recurrent or chronic low back pain. [36] Manipulation also was described as generally very safe if contraindications are respected (i.e., malignancies, fractures, bone infections, bleeding disorders, and so forth). In New Zealand, guidelines concluded that acute low back pain is managed best with simple analgesics or manipulation, which was found to be safe and effective in the first 4 to 6 weeks of symptoms, after which patients should be re-evaluated. [37]

Table 2 In the United Kingdom, practice guidelines state, “within the first 6 weeks of acute or recurrent low back pain, manipulation provides better short-term improvement in pain and activity levels and higher patient satisfaction than the treatments to which it has been compared”. [38] Other UK guidelines identified 36 randomized, controlled trials on manipulation for low back pain, 24 of which had some form of positive results. [39] The recommendations were to consider manipulation for patients requiring additional pain relief or a return to normal activities. A Swedish report of evidence-based care for chronic low back pain found strong evidence for the effectiveness of manipulation, especially to achieve short-term pain relief. [40] In Australia, investigators for guidelines on acute low back pain found that manual therapy seems more effective than placebo and was similar in effectiveness to other forms of conservative therapy. [41] Table 2 summarizes conclusions from different evidence-based clinical guidelines on manipulation for low back pain.
A meta-analysis in 1992 identified 23 randomized clinical trials of spinal manipulation for various types of low back pain (i.e., acute, subacute, chronic, sciatica, and so forth). [42] Methodologic quality was mixed, with quality scores ranging from 9% to 73%, with a mean of 39.3%. Outcomes in the manipulation group were better than the control group in 86% of the comparisons, although the size of the effect varied greatly. A review of manipulation for acute and subacute low back pain by Shekelle et al. in 1992 [7] identified nine controlled trials of varying quality that were of sufficient similarity to allow for meta-analysis. Combining the results from these trials, the authors reported that manipulation increased the probability of recovery from acute or subacute low back pain by 34% after 2 to 3 weeks of treatment.
Although most of the literature on manipulation has focused on acute low back pain, there is a growing body of data on its effectiveness for chronic low back pain. Early analyses of the literature, such as that by Shekelle et al. [7], rightfully concluded that there was insufficient evidence to form an opinion on the usefulness of spinal manipulation for chronic low back pain. A more recent systematic review of randomized, controlled trials of manipulation for subacute and chronic low back pain uncovered eight relevant trials. [43] Most (52.5%) reported positive results, whereas 25% reported negative results, and 12.5% reported inconclusive results. Methodologic quality was criticized again, especially in length of follow-up for outcomes.
Neck pain
The Quebec Task Force on Whiplash-Associated Disorders, after a review of the literature on all treatment approaches for this condition, produced a short list of reasonable treatment approaches and considered manipulation appropriate for the treatment of patients with whiplash-associated neck pain. [9] A systematic review of all research into nonsurgical, conservative treatments for neck pain found early evidence to support the use of manual treatments, in combination with other treatments, for short-term pain relief. [44] Another study reviewed evidence from 67 published articles that included randomized, controlled trials, cohort studies, case series, and case reports regarding manipulation and mobilization for various neck conditions (i.e., acute, subacute, and chronic neck pain with and without radiation). [5]
Methodologic quality was mixed, with quality scores ranging from 33% to 77%. These authors concluded that manipulation was of benefit for subacute or chronic neck pain, but that there was, at that time, insufficient evidence to evaluate its effectiveness for acute neck pain. A third review of manual therapies for neck pain found manipulation to be effective when used with other treatments for short-term pain relief; the authors also concluded that manipulation carried a low risk of complications. [45]
Headaches
An expert panel from Duke University recently published a review of physical treatments for tension-type and cervicogenic headaches and found evidence supporting the use of manipulation for those conditions. [6] In 1995, a literature review identified nine clinical trials (four randomized, controlled trials and five case series) of chiropractic for tension-type headaches and three trials (one randomized, controlled trial and two case series) for migraine headaches. [46] The outcomes of manipulation for tension-type headaches were generally good, and compared favorably with mobilization, ice, and amitriptyline; results for migraine headaches were fair, and more research in this area was recommended. Another review, by Hurwitz et al. [5], found evidence to support manipulation or mobilization in the relief of symptoms for muscle tension headache. A recent review [47] of cervicogenic headaches found that manipulation had the strongest evidence of all the treatments reviewed for treatment of this type of headache, with two randomized, controlled trials showing positive results.
Non-neuromusculoskeletal conditions
Research on the effectiveness of manipulation on non-NMS conditions such as asthma, premenstrual pain, and infantile colic has just started, and it is not possible to draw any conclusions about the evidence at this time. The literature on these topics is scant and consists mainly of case reports, cohort studies, and randomized, controlled trials with many methodologic flaws. For example, a study comparing spinal manipulation with sham manipulation for children with asthma found no significant differences between the groups. [48]
The study, however, was only single-blinded, the treatment was delivered by 11 different chiropractors, and the sham treatment included soft-tissue massage, gentle palpation, distraction, and small impulses to the spine. Studies reporting positive results for manipulation also have had strong flaws. A study of chiropractic for premenstrual syndrome found that symptoms generally could be reduced with manipulation and soft-tissue therapy. [49] The treatment, however, was delivered at seven separate clinics and varied according to practitioner preference, and the placebo consisted of an instrument many chiropractors use to deliver a low-force type of manipulation. A trial comparing manipulation with dimethicone for infantile colic found significant differences in hours of crying in favor of the manipulation group. [50] The treatment period was only 2 weeks with no long-term follow-up, however.
Safety of manipulation
A review of the available literature on the risk of adverse effects after manipulation shows that it remains a controversial subject. There is, however, a growing body of clinical surveys and epidemiologic studies that is providing information on this topic. It is quite common for patients to describe local discomfort in the area of treatment, or even headaches or fatigue. A recent survey concerning patients who report these complications noted that these symptoms are usually gone the next day, and none were present after 48 hours. [51] There are a few case reports of cauda equina syndrome after lumbar manipulation, but a review suggested that this occurred in only 1 in 100 million manipulations. [7, 52]
There is a reported association between cervical manipulation and vertebral artery dissection. Although this topic has been the source of a series of case reports and surveys, the exact frequency of this association remains unclear. A 10–year survey of chiropractors in Denmark uncovered only five cases in which a cerebrovascular event followed chiropractic treatment, for a rate of 1 per 1.3 million treatments. [53] The likelihood of a stroke after chiropractic manipulation in Canada has been reported to be 1 per 5.83 million treatments. Research by neurologists suggests that the frequency of this association may be somewhat higher, perhaps approximately 1 per 500,000 to 1 million cervical manipulations. [54, 55] A recent epidemiologic study in Ontario, Canada showed a five-fold increase in the association between chiropractic treatments and vertebral artery dissection for patients younger than 45 years of age; there was no increased risk in the general population or in patients older than 45. [56] It is probably reasonable to consider the risk of increased symptoms after manual therapy to the cervical spine to be 1% to 2%, whereas the risk of serious complication or death per cervical manipulation may be considered to be approximately 0.0001%. [45]
Patients with neck pain who receive any treatment are subject to risk, and the issue of relative safety is more important given similar outcomes in treatment. A review of the literature comparing the safety of manipulation with nonsteroidal anti-inflammatory drugs (NSAIDs) for neck pain concluded that “the best evidence indicates that cervical manipulation for neck pain is much safer than the use of NSAIDs, by as much as a factor of several hundred times”. [57] It is estimated that serious side effects resulting from the use of NSAIDs, such as gastrointestinal bleeding, may be as high as 0.4% per year, and death rates have been reported to be as high as 0.04% per year (3,200 deaths annually in the United States). [58–60] Cervical discectomy and fusion carries a reported death rate of 0.13% and a serious complication rate of 6.7%. [61]
Cost-effectiveness
A study of 1,397 chiropractic patients throughout the United States reported that 40% paid for treatment through private, fee-for-service insurance, 20% paid through Workers’ Compensation or personal injury cases, 20% were self-paying, and 20% paid through Medicare, prepaid insurance, or other methods. [20] Many insurance plans and managed care groups recently have initiated reimbursement of chiropractic services, primarily in response to member demands. [62] Plans for workers’ injuries in all states reimburse the services of chiropractors, and Medicare has reimbursed chiropractic care since 1972. Congress recently voted to integrate chiropractic into the medical services system of the Armed Forces after a successful demonstration project. [63]
Given the growth of third-party reimbursement, there is an increasing interest in studying the cost-effectiveness of chiropractic treatment. Early evidence from the literature is favorable to chiropractic. Jarvis et al. [64] reviewed 3,062 claims for back injuries in the Workers’ Compensation Fund of Utah in 1986 and compared the cost of medical versus chiropractic care. For six common back pain diagnoses, cost of care was significantly lower for chiropractic ($527 versus $684), and worker compensation costs were almost 10 times lower ($68 versus $668). A study of treatment costs for back or neck pain (International Classification of Diseases-9 codes 720–724) in a managed care setting showed significantly lower costs for chiropractic care ($539) than medical care ($774), with similar levels of patient satisfaction. [65]
Stano and Smith [66] reviewed 2 years of medical insurance claims data from 6,183 patients choosing chiropractic or medical care for nine common lumbar diagnoses and reported a lower median cost of care for chiropractic ($175 versus $221), mainly owing to inpatient costs incurred by medical patients.
The Manga et al. report [21] in Canada recommended that a government-sponsored health insurance plan enhance its coverage of chiropractors as first-contact physicians for musculoskeletal disorders to reduce health care costs. A detailed analysis of this literature by Baldwin et al. [67], however, has revealed many methodologic flaws in this literature and concludes that these studies fail to clarify whether medical or chiropractic care is more cost-effective. They recommend more rigorous studies on the topic.
Summary
Chiropractic is now more than a century old, and it is licensed throughout the United States and Canada and recognized in more than 60 countries worldwide. Doctors of Chiropractic receive training that is focused on the treatment of NMS conditions through manual and physical procedures, such as manipulation, massage, exercise, and nutrition. Most patients present to chiropractors with low back pain, neck pain, whiplash, and headaches. Numerous studies and expert panel reviews have supported the use of chiropractic and manipulation for these complaints. Satisfaction with chiropractic care for low back pain typically is good. Chiropractic, in general, offers safe and cost-effective procedures for selected musculoskeletal problems.
References:
Cooper RA, Laud P, Dietrich CL.
Current and projected workforce of nonphysician clinicians.
JAMA 1998;280:788–94.Gaumer GL, Walker A, Su S.
Chiropractic and a new taxonomy of primary care activities.
J Manipulative Physiol Ther 2001;24:239–59.Bigos SJ, editor.
Acute Lower Back Problems in Adults: Clinical Practice Guideline 14
AHCPR Publication No. 95–0642: US Department of Health and Human Services; 1994.Coulter I, Adams A, Coggan P, et al.
A Comparative Study of Chiropractic and Medical Education
Altern Ther Health Med. 1998 (Sep); 4 (5): 64–75Hurwitz EL, Aker PO, Adams AH, Meeker WC, Shekelle PG.
Manipulation and Mobilization of the Cervical Spine:
A Systematic Review of the Literature
Spine (Phila Pa 1976) 1996 (Aug 1); 21 (15): 1746–1760McCrory DC , Penzien DB et al. (2001)
Evidence Report: Behavioral and Physical Treatments for Tension-Type
and Cervicogenic Headache
Des Moines, Iowa, Foundation for Chiropractic Education and Research.Shekelle PG, Adams AH, Chassin MR, et al.
Spinal manipulation for low-back pain.
Ann Intern Med 1992;117:590–8.Shekelle PG, Brook RH.
A community-based study of the use of chiropractic services.
Am J Public Health 1991;81:439–42.Spitzer WO, Skovron ML, Salmi LR, Cassidy JD, Duranceau J, Suissa S, Zeiss E.
Scientific Monograph of the Quebec Task Force on Whiplash-Associated Disorders
Redefining Whiplash and its Management
Spine (Phila Pa 1976). 1995 (Apr 15); 20 (8 Suppl): S1-S73Goldstein M, editor.
The research status of spinal manipulative therapy,
DHEW publication no. (NIH) 76–998.
Bethesda, MD: US Department of Health, Education, and Welfare; 1975.Getzendanner S.
Permanent injunction order against AMA.
JAMA 1988;259:81–2.Baffi CR, Redican KJ, Morris L, et al.
Demographics and practice characteristics of chiropractors.
J Manipulative Physiol Ther 1988;11:85–8.Hawk C, Long CR, Boulanger KT.
Prevalence of Nonmusculoskeletal Complaints in Chiropractic Practice:
Report From a Practice-based Research Program
J Manipulative Physiol Ther 2001 (Mar); 24 (3): 157–169Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van Rompay M, Kessler RC.
Trends in Alternative Medicine Use in the United States, 1990 to 1997:
Results of a Follow-up National Survey
JAMA 1998 (Nov 11); 280 (18): 1569–1575Astin JA.
Why patients use alternative medicine.
JAMA 1998;279:1548–53.Drivdahl CE, Miser WF.
The use of alternative health care by a family practice population.
J Am Board Fam Pract 1998;11:244–6.Druss BG, Rosenheck RA.
Association between use of unconventional therapies
and conventional medical services.
JAMA 1999;282:651–6.Palinkas LA, Kabongo ML.
The use of complementary and alternative medicine
by primary care patients.
J Fam Pract 2000;49:1121–30.Deyo RA, Tsui-Wu YJ.
Descriptive epidemiology of low-back pain and its
related medical care in the United States.
Spine 1987;12:264–8.Hurwitz EL, Coulter ID, Adams AH, et al.
Use of chiropractic services from 1985 through 1991
in the United States and Canada.
Am J Public Health 1998;88:771–6.Manga P, Angus D, Papadopoulos C, Swan W.
The Effectiveness and Cost-Effectiveness of Chiropractic
Management of Low-Back Pain
Ottawa: Kenilworth Publishing; 1993.Ted J. Kaptchuk, OMD; David M. Eisenberg, MD
Chiropractic. Origins, Controversies and Contributions
Archives of Internal Medicine 1998 (Nov 9); 158 (20): 2215-2224Cherkin, D.C. and MacCornack, F.A.
Patient Evaluations of Low Back Pain Care From
Family Physicians and Chiropractors
Western Journal of Medicine 1989 (Mar); 150 (3): 351–355Meade TW, Dyer S, Browne W, et al:
Randomised Comparison of Chiropractic and Hospital Outpatient
Management for Low Back Pain: Results from Extended Follow up
British Medical Journal 1995 (Aug 5); 311 (7001): 349–351Solomon DH, Bates DW, Panush RS, et al.
Costs, outcomes, and patient satisfaction by provider type for patients
with rheumatic and musculoskeletal conditions: a critical review
of the literature and proposed methodologic standards.
Ann Intern Med 1997;127: 52–60.Verhoef MJ, Page SA, Waddell SC.
The Chiropractic Outcome Study: Pain, Functional Ability
and Satisfaction With Care
J Manipulative Physiol Ther 1997 (May); 20 (4): 235–240Palmer DD.
The chiropractor’s adjuster, the science, art and philosophy of chiropractic.
Portland, Oregon: Portland Printing House; 1910.Evans DP, Burke MS, Lloyd KN, et al.
Lumbar spinal manipulation on trial, part I:
Clinical assessment.
Rheumatol Rehabil 1978;17:46–53.Nwuga VCB.
Relative therapeutic efficacy of vertebral manipulation and
conventional treatment in back pain management.
Am J Phys Med Rehabil 1982;61:273–8.Roston JB, Wheeler Haines RW.
Cracking in the metacarpophalangeal joint.
J Anat 1965;81:165.Unsworth A, Dowson D, Wright V.
Cracking joints, a bioengineering study of cavitation
in the metacarpophalangeal joint.
Ann Rheum Dis 1971;30:348–358.Giles LGF.
Lumbosacral and cervical zygapophyseal joint inclusions.
Manual Medicine 1986;2:89–92.Herzog W, Scheele D, Conway PJ.
Electromyographic responses of back and limb muscles
associated with spinal manipulative therapy.
Spine 1999;24:146–52.Dishman JD, Bulbulian R.
Spinal reflex attenuation associated with spinal manipulation
Spine 2000 (Ict 1); 25: 2519–2525Sato A.
Spinal reflex physiology.
In: Haldeman S, editor. Principles and practice of chiropractic.
2nd edition. Norwalk, CT): Appleton & Lange; 1992.Manniche C, Ankjær-Jensen A, Olsen A, et al.
Low-Back Pain: Frequency, Management and Prevention
from an HTA perspective
Copenhagen: Danish Institute for Health Technology Assessment, 1999.ACC, the National Health Committee.
New Zealand Acute Low Back Pain Guide
Wellington, NZ: Ministry of Health, 1997.Waddell G.
Chiropractic for low back pain: evidence for manipulation is stronger
than that for most orthodox medical treatments.
BMJ 1999;318:262.Royal College of General Practitioners.
Clinical Guidelines for the Management of Acute Low Back Pain
London: Royal College of General Practitioners; (1999). [UK]van Tulder MW, Goossens M, Waddell G, Nachemson A.
Conservative treatment of chronic low back pain.
In: Nachemson A, Jonsson E, editors. Swedish SBU report:
evidence based treatment for back pain.
Stockholm/Philadelphia: Swedish Council on Technology Assessment in Health Care (SBU)/
Lippincott Williams & Wilkins; 2000.Bogduk N, for the Australasian Faculty of Musculoskeletal Medicine
for the National Musculoskeletal Medicine Initiative.
Evidence-based clinical guidelines for the management of acute low back pain.
Canberra, Australia: National Medical Research Council; 1999.Anderson R, Meeker WC, Wirick BE, Mootz RD, Kirk DH, Adams A.
A meta-analysis of clinical trials of spinal manipulation.
J Manipulative Physiol Ther 1992;15:181–94.Koes BW, Assendelft WJ, van der Heijden GJ, et al.
Spinal manipulation for low back pain:
an updated systematic review of randomized clinical trials.
Spine 1996;21:2860–71.Aker PD, Gross AR, Goldsmith CH, Peloso P.
Conservative management of mechanical neck pain:
systematic overview and meta-analysis.
BMJ 1996;313:1291–6.Gross AR, Aker PD, Quartly C.
Manual therapy in the treatment of neck pain.
Rheum Dis Clin North Am 1996;22:579–98.Vernon HT.
The effectiveness of chiropractic manipulation in the treatment
of headache: an exploration in the literature.
J Manipulative Physiol Ther 1995;18:611–17.Haldeman S, Dagenais S.
Cervicogenic Headaches: A Critical Review
Spine J 2001 (Jan); 1 (1): 31–46Balon J, et al.
A Comparison of Active and Simulated Chiropractic Manipulation
as Adjunctive Treatment for Childhood Asthma
New England Journal of Medicine 1998; 339(15): 1013-1020Walsh MJ, Polus BI.
A randomized, placebo-controlled clinical trial on the efficacy
of chiropractic therapy on premenstrual syndrome.
J Manipulative Physiol Ther 1999;22: 582–5.Wiberg, JM, Nordsteen, J, and Nilsson, N.
The Short-term Effect of Spinal Manipulation in the Treatment of Infantile Colic:
A Randomized Controlled Clinical Trial with a Blinded Observer
J Manipulative Physiol Ther 1999 (Oct); 22 (8): 517–522Leboeuf-Yde C, Hennius B, Rudberg E, et al.
Side effects of chiropractic treatment: a prospective study.
J Manipulative Physiol Ther 1997;20:511–5.Haldeman S, Rubinstein S.
Cauda equina syndrome in patients undergoing manipulation of the lumbar spine.
Spine 1992;17:1469–73.Klougart N, Leboeuf-Yde C, Rasmussen LR.
Safety in Chiropractic Practice, Part I; The Occurrence of Cerebrovascular Accidents
After Manipulation to the Neck in Denmark from 1978-1988
J Manipulative Physiol Ther 1996 (Jul); 19 (6): 371–377Carlini W.
American Heart Association News 1995;Feb.19.Norris JW, Beletsky V, Nadareishvili ZG.
Sudden Neck Movement and Cervical Artery Dissection
CMAJ. 2000 (Jul 11); 163 (1): 38–40Rothwell DM, Bondy SJ, Williams JI.
Chiropractic Manipulation and Stroke:
A Population-based Case-control Study
Stroke 2001 (May); 32 (5): 1054-1060Dabbs V Lauretti WJ
A Risk Assessment of Cervical Manipulation vs. NSAIDs
for the Treatment of Neck Pain
J Manipulative Physiol Ther 1995 (Oct); 18 (8): 530–536Carson JL, Strom BL, Soper KA, West SL, Morse ML.
The association of non-steroidal anti-inflammatory drugs
with upper gastrointestinal tract bleeding.
Arch Int Med 1987; 147:85–8.Fries JF.
Assessing and understanding patient risk.
Scand J Rheumatol 1992;92:21–4.Gabriel SE, Jaahkimainen L, Bombadier C.
Risk for serious gastrointestinal complications related to use of
non-steroidal anti-inflammatory drugs: a meta-analysis.
Ann Intern Med 1991;115:787–96.Romano PS, Campa DR, Rainwater JA.
Elective cervical discectomy in California:
postoperative in-hospital complications and their risk factors.
Spine 1997;22:2677–92.Pelletier KR, Marie A, Krasner M. et al.
Current Trends in the Integration and Reimbursement of Complementary and
Alternative Medicine by Managed Care, Insurance Carriers, and Hospital Providers
Am J Health Promot 1997 (Nov); 12 (2): 112–122Dynamic Chiropractic staff writer.
Congress passes historic chiropractic legislation.
Dynamic Chiropractic, November 15, 2000.Jarvis K.B., Phillips R.B., Morris E.K.
Cost Per Case Comparison of Back Injury Claims of Chiropractic Versus
Medical Management For Conditions With Identical Diagnostic Codes
J Occup Med 1991 (Aug); 33 (8): 847–852Mosley CD, Cohen IG, Arnold RM.
Cost-effectiveness of chiropractic care in a managed care setting.
American Journal of Managed Care 1996;2:280–2.Stano M, Smith M.
Chiropractic and medical costs of low back care.
Med Care 1996; 34:191–204.Baldwin ML, Cote P, Frank JW, et al.
Cost-effectiveness Studies of Medical and Chiropractic Care for
Occupational Low Back Pain. A Critical Review of the Literature
Spine J. 2001 (Mar); 1 (2): 138–147
Return to ALL ABOUT CHIROPRACTIC
Since 12-18-2022


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |