

Chiropractic Integration Within a Community
Health Centre: A Cost Description and Partial
Analysis of Cost-utility from the
Perspective of the InstitutionThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Can Chiropr Assoc. 2019 (Aug); 63 (2): 64–79 ~ FULL TEXT
OPEN ACCESS Peter C Emary, DC, MSc, Amy L Brown, DC, Douglas F Cameron, DC, and Alexander F Pessoa, DC
Private Practice, Cambridge, ON, Canada.
FROM: Weeks ~ JMPT 2016 (Feb) Hurwitz ~ JMPT 2016 (May)OBJECTIVE: To evaluate costs and consequences of a new back pain service provided by chiropractors integrated into a Community Health Centre in Cambridge, Ontario. The study sample included 95 consecutive patients presenting between January 2014 to January 2016 with a mixture of sub-acute and chronic back pain.
METHODS: A secondary cost-utility analysis was performed and conducted from the perspective of the healthcare institution. Cost-utility was calculated as cost per quality-adjusted life year (QALY) gained over a time horizon of 90 days.
RESULTS: According to the EuroQol 5 Domain questionnaire, nearly 70% of patients improved. The mean number of treatment sessions was 8.4, and an average of 0.21 QALYs were gained at an average cost per QALY of $1,042. Seventy-seven percent of patients did not visit their primary care provider over the 90-day period, representing potential cost savings to the institution of between $2,022.23 and $6,135.82.
There are more articles like this @ our: Cost-Effectiveness of Chiropractic Page Conclusions: Adding chiropractic care to usual medical care was associated with improved outcomes at a reasonable cost in a sample of complex patients with sub-acute and chronic back pain. Future comparative cost-effectiveness studies are needed.
KEYWORDS: chiropractic; community health centres; cost analysis; health services research
From the FULL TEXT Article:
Introduction
The efficacy for chiropractic care including manipulative therapy in treating patients with spine-related pain has been established. [1–3] Moreover, clinical trials have shown greater efficacy when chiropractic treatment is added to usual medical care in managing patients with these conditions. [4, 5] Chiropractic care also has the potential to be cost-effective, as chiropractors typically use a conservative (i.e. non-pharmacological, non-surgical) approach. In fact, studies have shown that when managed by a chiropractor, even when controlling for confounding factors, patients tend to have fewer advanced medical procedures including opioids and referrals for diagnostic imaging, injections, or spinal surgery. [6–8]
Although chiropractic care has been suggested as a cost-effective alternative to the medical management of spine-related pain disorders9, the evidence for economic evaluations of chiropractic treatment compared with, or added to, medical care is inconclusive. [10] Regardless, back and neck pain remain prevalent and costly in society. The socioeconomic burden of these disorders, in terms of health resource utilization and economic costs (e.g. lost productivity), is particularly high among vulnerable populations. [9, 11] In Canada, such populations commonly receive health care services at the primary care level within Community Health Centres (CHCs). [12]
CHCs are non-profit, publicly funded and community-governed organizations that promote health, illness prevention, and community development. [12] These centres employ multidisciplinary teams of health professionals that traditionally include medical doctors, nurse practitioners, registered nurses, dieticians, social workers, and community health workers. CHCs are distinct from other primary care centres in that they serve the needs of complex patient populations, typically including younger individuals, the socioeconomically disadvantaged, people with severe mental health or addiction issues (e.g. opioid over-use), and those with various other co-morbidities. [12, 13] Musculoskeletal disorders including chronic back pain are also prevalent among these groups. [9, 14, 15] To improve the management of these patients, particularly in the clinical area of low back pain, a growing number of Ontario CHCs have been adding chiropractic care to their existing medical services. Some of these programs have been voluntary [16] and some have been funded as pilot projects by the Ontario Ministry of Health and Long-Term Care [14, 17]
In line with such integration, the examination of costs and cost-effectiveness of chiropractic care has become one of the top research priorities for the chiropractic profession in Canada. [18] In 2017, a pilot project was conducted to evaluate a new integrated chiropractic back pain program at the Langs CHC in Cambridge, Ontario. [16, 19] The main findings included patient-reported improvements in back pain intensity, disability and health-related quality of life, high levels of satisfaction, and reduced primary care provider visits and analgesic use with this service. [16] Although such findings suggest potential for health cost savings, a formal economic evaluation of this project was not undertaken. Others have found similar outcomes [14, 15, 17] yet few studies have examined the costs associated with chiropractic integration into primary healthcare settings, including within CHCs. Moreover, no studies have explored whether the implementation of these programs is cost-effective from the institutional point of view. As such, the purpose of the current study was to conduct a secondary analysis of the aforementioned program16 using an economic evaluation design completed from the perspective of the Langs CHC. [19] Resource utilization and costs at the CHC from the health system perspective will be measured in a future study.
Research Question
In adult patients with back pain presenting within a CHC setting, is the addition of chiropractic care to usual medical care cost-effective from the perspective of the healthcare institution?
Methods
Study Design
This was a secondary cost-utility analysis [20] of a prospective, single-cohort observational study of a new back pain service provided by chiropractors integrated into a primary care CHC setting. The service was evaluated using patient-reported outcome measures, and data were collected prospectively on consecutive patients throughout the first two years of the program between January 2014 and January 2016. [16] For the current study, cost-utility was calculated as cost per quality-adjusted life year (QALY) gained. All costs are presented in 2019 Canadian dollars, and the perspective of the analysis was the Langs CHC (i.e. healthcare institution). The time horizon was 90 days (i.e. the length of time used for a care episode of low back pain in the previous study [16]). With a time horizon of less than one year, discounting of costs and effects was not performed.
Chiropractic Care
The chiropractic service provided at the CHC has been described previously. [16] Briefly, treatment sessions were evidence-based [21] and included high-velocity, low-amplitude spinal manipulation, soft-tissue therapy, education, reassurance, and home advice (e.g. icing, spinal stretching, and core strengthening exercises). Initial visits were typically 60 minutes in length and follow-up visits were 15 minutes. The service was provided on a rotating basis by four chiropractors (PCE, ALB, DFC, AFP), and was accessible on Tuesdays and Thursdays at the CHC from 12pm to 2pm, for a total of four hours per week.
Usual Medical Care
At the time of referral for chiropractic treatment all patients had already been under the management of their primary care provider for a back pain-related complaint. This was termed as ‘usual medical care’ and defined as any and all medical care received by patients with back pain at the Langs CHC, including but not limited to: primary care provider consultation visits (approximately 30 minutes in length), prescription medications (i.e. muscle relaxants, anti-inflammatories, analgesics), referrals for specialty care (e.g. spine surgical consultation), and referrals for diagnostic testing (e.g. lab work, imaging).
Patients
To be eligible, participants were: rostered patients at the Langs CHC, 18 years of age or older, seen and referred by their primary care provider (i.e. medical doctor or nurse practitioner) for a back pain-related complaint, unable to privately pay for chiropractic care, and suitable for manual therapy (i.e. absence of “red flags” [21]). Patients were screened by their primary care provider for eligibility and referred for chiropractic treatment. Referred patients included both naïve chiropractic patients and those with prior experience with chiropractic care. Patients completed an initial questionnaire before their first appointment, and then again at or before 90-day follow-up.
Baseline and Follow-up Instruments
Outcome measures included the Bournemouth (BQ)22 and Bothersomeness23 questionnaires, the Patient Global Impression of Change (PGIC), [24] and the EuroQol 5 Domain (EQ-5D). [25] The EQ-5D (3L version) is a widely used generic measure of health status commonly used in economic evaluations such as cost-utility analyses. [26] It assesses patient health in five dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression). Each of these dimensions has three levels of response: no problems, some problems, and extreme problems. The EQ-5D also includes a visual analogue scale (VAS), on which the patient rates their perceived health from 0 (worst health imaginable) to 100 (best health imaginable). Responses from the five EQ-5D domains were used in the current study to generate a descriptive profile and a single index value of health status (i.e. utility) for each patient. [26] The pre-treatment and follow-up questionnaires also inquired about patient satisfaction, work status, details of medication usage, and other health care utilization. All instruments were administered at baseline and at (or before) 90-day follow-up.
Data Analysis
Descriptive statistics were used to summarize the demographic and clinical characteristic data from the pre-treatment questionnaires. For follow-up data, comparisons were made between responders and non-responders using the chi-squared test (or Fisher’s exact test when appropriate) and independent t-test for categorical and continuous variables, respectively. The distributions for cost and effect data were analyzed for normality by examining data histograms, probability plots, and quantile-quantile plots, and then confirmed with the Kolmogorov-Smirnov test. For normal distributions, average values were calculated as the mean with 95% confidence intervals (CIs). For non-normal distributions, non-parametric bootstrapping (using 10,000 samples taken with replacement) was used to estimate 95% CIs. Because cost data are typically skewed20, average values were also presented as the mean (standard deviation) and median (inter-quartile range) for comparison. Statistical significance was set at p < 0.05, and SAS® (SAS Institute Inc., Cary, North Carolina), Version 9.4, was used for analysis.
Analyses of the BQ, Bothersomeness, and PGIC outcome scores for the study have been described elsewhere.16 For the EQ-5D, each patient’s index (or utility) score was calculated using the EuroQol societal preference weights for Canada. [27] In general these scores range from less than 0 (where 0 is a health state equivalent to death, and negative values are valued as worse than death) to 1 (perfect health), with higher scores indicating higher health utility. [26] These were then used to calculate QALYs, as the change in EQ-5D index scores from baseline to follow-up multiplied by the estimated length of effect. [28, 29] These values were then adjusted to a 90-day time horizon (by dividing each by four) for the current study. In addition, individual EQ-5D domain change scores were calculated and presented as recommended by EuroQol. [25, 26]
A Paretian method [26, 30] was also used to compare patients’ EQ-5D health states pre- and post-chiropractic treatment. With this method, patients were categorized into one of four categories: worse (i.e. worse in at least one dimension and no better in any other), same (i.e. no change in pre-post health state profiles), mixed (i.e. better on one dimension, but worse on another), and improved (i.e. better on at least one dimension and no worse in any other).

Table 1 For the cost analysis, cost estimates were obtained directly from the Langs institution. CHCs including Langs are unique in that they, unlike most Canadian primary care centres, which use fee-for-service reimbursement from provincial health plans for physician services, employ health professionals on a salaried basis. [13] For the purposes of this study, despite chiropractic services only being partially subsidized at the Langs CHC [16] we examined cost-utility of the program in a fully funded scenario. In addition, resource use for the program was determined by combining hourly wages and overhead expenses with the total number of hours of clinic operation over a 90-day period. For example, if the chiropractic low back pain program operated four hours per week this would result in a total of 52 hours over a 90-day period. Cost per patient was then calculated as the number of treatment visits (converted into total hours of use) multiplied by the unit costs of the program. For example, if a patient came to the clinic for a total of nine chiropractic treatment visits (one 60-minute initial visit and eight 15-minute follow-up visits) this would equal a total of three hours of chiropractic service use. If the total hourly cost of the chiropractic low back pain program (including hourly chiropractor salary, shared reception, and overhead expenses) was $95.04 then the total program cost for that patient would be $285.12. Resource use items and unit costs from the perspective of the healthcare institution are provided in Table 1.
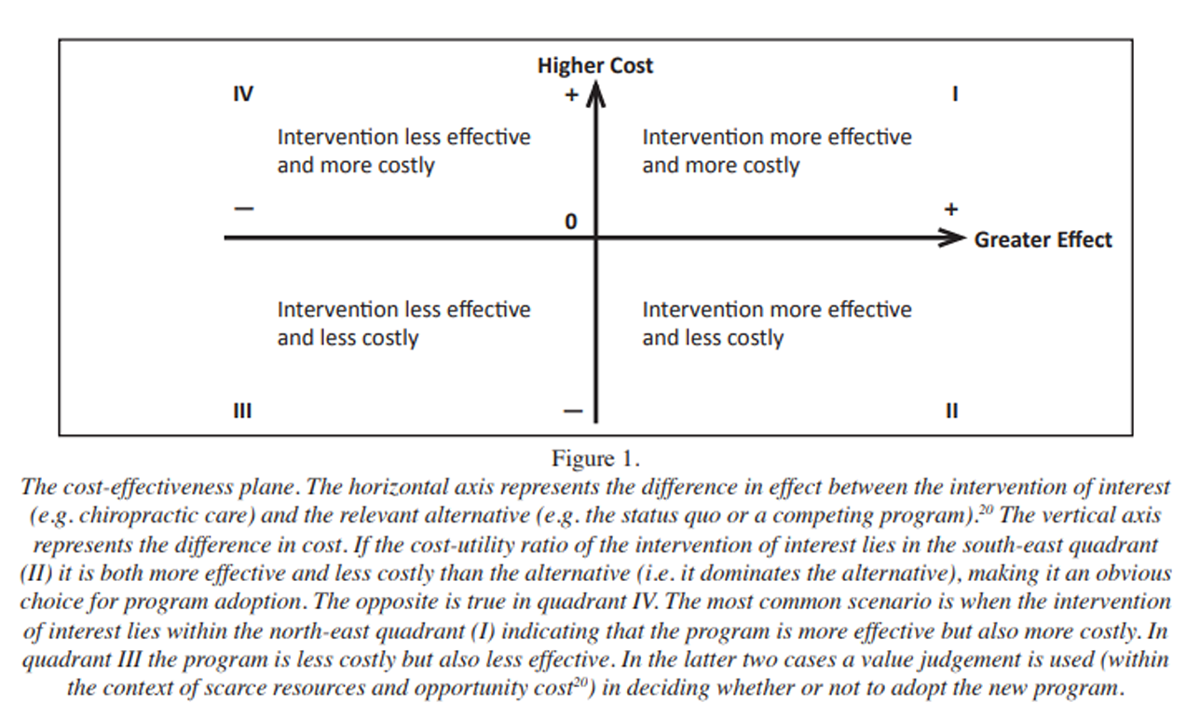
Figure 1 Cost-utility of the chiropractic program was calculated as the average cost per QALY gained per patient during the 90-day period and plotted graphically on a cost-effectiveness plane (Figure 1). We performed a one-way sensitivity analysis [20] comparing mean and median cost per QALY gained values to investigate the impact of any differences between these values on study results. We also tested for potential cost savings of the program in a scenario [20] sensitivity analysis (see below).
Ethical Considerations
This study was approved by the AECC University College Policy and Procedures on Research Ethics. [16] All patients were also informed in writing at their first visit that the information given in the questionnaires would be used anonymously. Informed consent to chiropractic treatment was performed by the attending clinician.
Results
Patient Characteristics

Table 2 In total, 95 consecutive patients reporting a back pain-related complaint were included in the service evaluation. The mean age of the cohort was 49 (±16) years and two-thirds (66%) were unemployed. Of those in paid employment, most (88%) were on sick leave because of their back pain. Eighty percent of patients had sub-acute (24%) or chronic (56%) back pain, with most describing it as constant (68%) and disabling (90%). Only a minority (19%) of patients had had a pain-free month in the past six months, and nearly four out of every 10 (37%) rated themselves in poor general health. Despite being a mostly chronic back pain population, the large majority (84%) expected to improve with treatment. In general, patients were also high users of health care services with two-thirds (65%) taking daily prescription analgesics and a similar proportion (67%) utilizing other health care providers in addition to their primary care physician for pain management. Baseline demographic and clinical characteristics of the study sample are summarized in Table 2.
Follow-Up
There were a substantial number of patients who after completing the baseline assessment dropped out or were lost to follow-up. Out of 95 patients, 45 completed both the initial and follow-up assessments (47.4% response rate). Baseline data between responders and non-responders were analyzed for bias but no differences in age, sex, and severity of their condition (as measured by baseline total BQ scores) were found between the two groups. [16] Baseline EQ-5D scores were nearly all identical as well, with the exception that fewer responders reported extreme problems with anxiety and depression compared to non-responders (Appendix 1). No information was available regarding loss to follow-up of patients under usual medical care.
Patient-Reported Outcome Measures
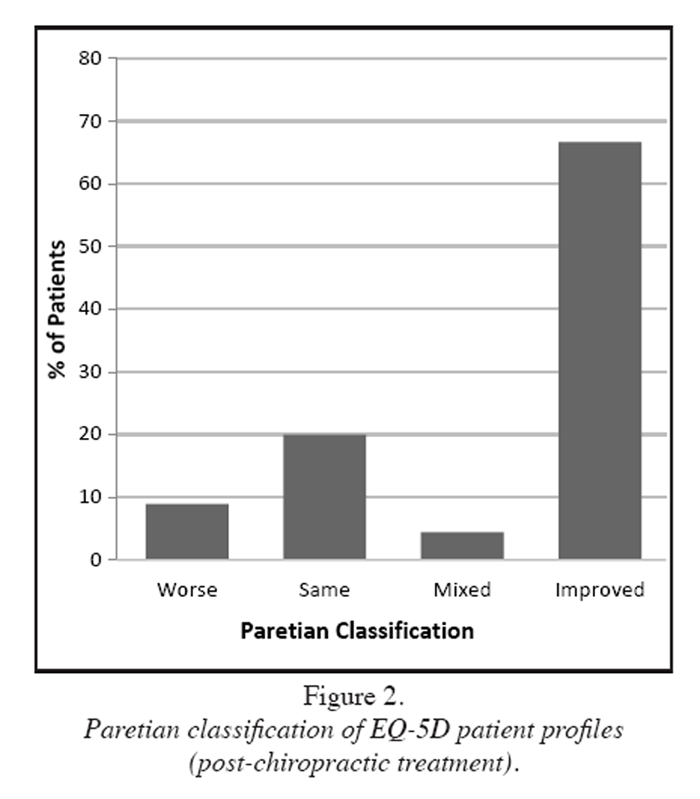
Figure 2

Table 3 Health outcomes for the BQ, Bothersomeness, PGIC, and patient satisfaction measures have been reported elsewhere. [16] EQ-5D scores as categorized using the Paretian method indicated that two-thirds (67%) of patients at follow-up improved and fewer than one in 10 (8.9%) had worsened (Figure 2). The remainder stayed about the same (20%) or had mixed improvement (4.4%). These results were similar to those obtained in the study sample using the BQ, Bothersomeness, and PGIC measures reported previously. [16] An analysis of the five EQ-5D domains revealed that the highest reported changes for improvement (in decreasing order) were in self-care, anxiety/ depression, usual activities, and mobility, whereas the lowest changes in improvement reported by patients were in pain/discomfort (Table 3).
Cost Analysis
The mean time between completing the pre-treatment and follow-up questionnaires over the 90-day period was 10 ± 8.3 weeks (range, 1–47 weeks). The mean number of chiropractic treatment sessions that patients received during this time was 8.4 ± 3.8 (range, 2–16 visits). Among this group, nearly half (46%) of those who were on sick leave for their back-pain complaint returned to work post-chiropractic treatment. With regards to other health care utilization, more than three-quarters (77%) had not sought help from any other practitioner for their back pain during the follow-up period, and more than eight out of 10 (82%) were either not taking any medication or had managed to significantly reduce their medication usage for their pain.

Table 4

Table 5
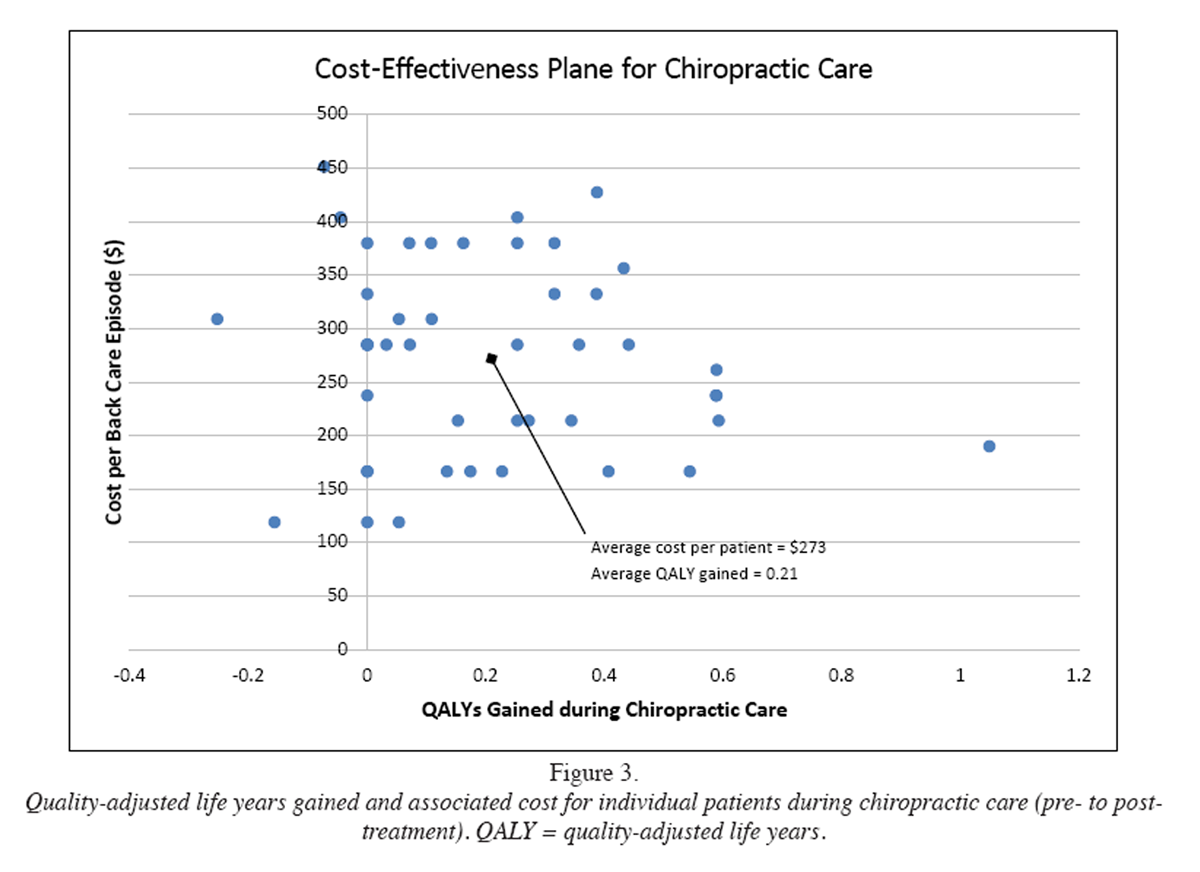
Figure 3 An analysis of the cost of care during the 90-day follow-up period is shown in Table 4. The mean total cost of direct care was approximately $263 (95% CI, $237 to $289) per patient, while the overhead cost for use of an examination room was only around $10 (95% CI, $9 to $11) per patient, leading to a total mean cost of care of about $273 (95% CI, $246 to $300). Chiropractic consultation visits, fully subsidized by the Langs institution at a rate of $81 per hour, would have contributed to 85% of total costs. Other costs including shared reception services and overhead expenses would constitute around 11% and 4%, respectively.
The costs to the healthcare institution per QALY gained with chiropractic care are summarized in Table 5. Over the 90-day period an average of 0.21 (95% CI, 0.14 to 0.29) QALYs were gained at an average cost per QALY (including overhead expenses) of $1,042 (95% CI, $768 to $1,340). This represents a trade-off between higher costs and improved outcomes for patients treated with chiropractic care (compared with no chiropractic care). [20] This trade-off is illustrated in Figure 3 as the distribution of cost versus QALYs gained during chiropractic care. The average cost per QALY gained would fall within the north-east quadrant of the cost-effectiveness plane. When median cost per QALY gained was used, the value reduced (i.e. $905 vs. $1,042) and remained in a trade-off position yet would fall at a more south-easterly position (not shown in Figure 3).
Cost Savings
Studies from the literature have reported the mean number of annual visits to a primary care physician for the management of chronic back pain to be between 5.4 and 16.4 per patient. [31, 32] Assuming similar rates of utilization, if 77% of patients in the current study did not visit their primary care provider during the 90-day period while under chiropractic care this would result in cost savings for the institution. For instance, if primary care visits at the Langs CHC were 30 minutes in length and if an average wage of $86.42 for medical services was used (see Table 1), the reduced total number of hours of primary care visits in this cohort of patients over a 90-day period would have ranged between 23.4 and 71 hours, representing a potential cost savings from this program of between $2,022.23 and $6,135.82. (This was assuming a linear relationship between cost reduction and time in extrapolating these figures from 10 weeks [i.e. the average number of weeks patients were under this service] to three months.) Taking these cost savings into account, in a worst-case scenario the average cost per QALY gained during chiropractic care would have remained in a trade-off position between higher costs and improved outcomes, but at a lower cost per QALY gained (i.e. $517 [95% CI, $466 to $568] vs. $1,042 [95% CI, $768 to $1,340]). However, in a best-case scenario there would have been an average cost savings of $212 (95% CI, $193 to $231) per QALY gained per patient, moving the cost-utility ratio into the southeast quadrant of the cost-effectiveness plane (Appendix 2). Median cost per QALY gained values were slightly lower in each scenario (i.e. $431 and ?$177, respectively) but did not change the qualitative conclusions of the results.
Discussion
This study aimed to evaluate the potential cost-utility of chiropractic services integrated within a Canadian primary care CHC setting from the perspective of the healthcare institution. Nearly 70% of patients who were referred into this service pathway and followed through to discharge reported improvement with chiropractic care. This finding is consistent with those of other studies involving the integration of chiropractic services in the management of patients with low back pain and other musculoskeletal disorders. [14–17, 33] On average, patients also reported a gain of 0.21 QALYs over a 90-day period. In other words, each patient gained an average of 0.21 years (i.e. greater than two and a half months) in full health during this time as a result of receiving chiropractic treatment. This is an important finding as the majority of patients in this study reported persistent back pain symptoms at baseline despite being under usual medical care.
Without taking potential cost savings of the current program into consideration, the average cost per QALY gained per patient over the 90-day treatment period was $1,042. When compared to a threshold of $20,000 per QALY recommended in Canada as a cut-off for accepting health care programs as being cost-effective [34], this program appears to represent very good value-for-money. In essence, needed resources that would be displaced from other treatments or programs at the healthcare institution in order to fund the chiropractic program (i.e. the opportunity cost [20]) would be comparatively low. Although this threshold is arbitrary and has been challenged in the literature [36] many healthcare programs including pharmaceutical and surgical interventions with equivocal long-term outcomes to chiropractic treatment [36-38] have been universally adopted in healthcare systems at much higher cost-utility ratios than the current program. [39]
The findings of the current study suggest there may also be potential for cost savings to the healthcare institution when chiropractic care is added to usual medical care in the management of complex patient populations such as those who present within CHCs. For instance, over three-quarters of patients in this study did not visit their primary care provider while under chiropractic care. Similar reductions in physician visits in association with chiropractic integration have also been reported elsewhere. [15, 40] When taken in to account this translates into an estimated average cost reduction (in terms of hourly services in primary care provider visits) of between greater than $2,000 and $6,000 over the course of three months. (Exact values calculated were $2,022.23 and $6,135.82, respectively.) In a fully funded scenario, if the chiropractic program were to cost the healthcare institution $4,942.08 over three months, the opportunity cost (i.e. resources that would need to be displaced from other programs to fund the chiropractic program) over this time period would range from a high of around $3,000 to a low of nearly ?$1,200. In other words, in the first case, and in the context of scarce resources, a choice would need to be made by the healthcare institution in order to decide if the value of what is being added is greater than the value of what is being given up. [20] For instance, would it be worth taking resources from other institution programs (e.g. youth and teen, diabetes education, midwifery [19]) to fund low back pain services?
Alternatively, the institution could generate the required resources through, for example, additional fundraising and/or government grants. In the second case, however, the potential cost savings alone would more than subsidize the chiropractic service. Although we did not consider the costs to the institution for patients who were lost to follow-up, we also did not consider the cost savings these patients may have created for the institution by not visiting their primary care provider while under chiropractic care. For instance, these patients had an average of 3.6 ± 2.8 (range, 1–11) visits at the institution at the point they were lost to follow-up. Although this group would have generated less in terms of potential cost savings to the institution, they also would have created less costs as they attended for fewer visits than the group of patients not lost to follow-up (i.e. average of 3.6 vs. 8.4 visits). Notwithstanding, the estimated reductions in primary care provider visits for this study were based on rates of physician utilization by chronic back pain patients observed in other research [31, 32], as actual rates were not tracked in the current study. Until such measures are conducted, caution is warranted in applying these estimates to the current context.
In addition to reduced primary care provider visits, the majority of patients in this service pathway at follow-up reported reductions in the use of analgesic medications. Reductions in pain medication usage with access to chiropractic services have also been reported in other studies. [5, 6, 8, 17, 33, 40] In light of the current opioid crisis, further investigation regarding the impact of chiropractic integration on opioid use among chronic back pain patients in the healthcare system is warranted.
In this study almost half of respondents who were employed but on sick leave at baseline returned to work after the 90-day treatment period. As unemployment rates and disability are characteristically high among CHC patient populations [13-16], this is also a potentially important finding. The return-to-work of even a small number of such cases has indirect cost savings implications from the societal perspective. From the health system perspective there may have been other reductions in health service utilization, such as emergency department visits, orders for advanced diagnostic imaging, referrals for injections, and/or referrals for spinal surgery, that were not measured in the current study. Spine-related pain is often disabling and recurrent41, particularly in complex patients and those of low socioeconomic status. [9, 11, 13–16, 41] Such patients also tend to be high users of healthcare services. [11] By adding chiropractic care to usual medical care within the CHC setting, the findings of the current study and others [14–16, 33, 40 ] suggest there may be potential for cost savings outside of those obtainable through the healthcare institution. As such, the effect of chiropractic integration on these and other direct and indirect health system and societal costs and consequences should be measured in future investigations. Future studies should include a comparator group so as to properly evaluate these programs within the economic context. [20]
Limitations
This study had several important limitations. First, this was a single-cohort study conducted on a relatively small patient sample. A complete economic evaluation would have included a comparison between at least two health care programs or alternatives. [20] Although the current study design allowed for the evaluation of the addition of a new program to the existing back care services provided at the CHC (i.e. chiropractic care plus usual medical care) data were not collected on a control group of patients not receiving chiropractic treatment. As such, incremental cost-utility (i.e. the added cost per additional QALY gained with the new program compared to the existing one) could not be calculated. At best, cost-utility could only be examined from a ‘with’ versus ‘without’ chiropractic care scenario as part of a partial economic evaluation. [20]
Second, there was a high loss to follow-up. In all pragmatic studies, which, by their nature, are not conducted in a highly controlled research environment, there is likely to be a relatively high number of dropouts, as was the case here. However, we are not aware of any systematic differences between those patients who did and did not complete follow-up questionnaires as baseline characteristics were similar between the two groups. Nevertheless, caution is warranted in extrapolating the findings to other CHC populations.
Third, QALYs were measured for this study using a time trade-off approach. [26] In brief, with this method 243 potential individual health states from the EQ-5D (3L) were transformed into single indexes. The difference between the pre- and post-treatment indexes were then multiplied by the estimated length of effect (and then adjusted to a 90-day time horizon) to obtain the QALYs gained for each patient from chiropractic treatment. [28] Although a complete set of these indexes has been obtained from a representative sample of the Canadian general population, [27] and this value set was used in calculating QALYs for the current study, these measures were based on societal preferences and not that of the individual patient. For this and other reasons (such as the restrictive assumptions that underlie utility theory [20]) QALYs have been criticized in the literature [42] and measures such as healthy-years equivalents (HYEs) and willingness-to-pay methods have been suggested as superior alternatives. [42, 43] Although this value set was obtained from a Canadian population27 there may have also been systematic differences in terms of socio-demographics between this group and the current study sample. For instance, when contrasted with the current study cohort participants in the aforementioned sample [27] were, on average, older, more well-educated, and of a higher socioeconomic class (i.e. higher income levels). As such, these preference weights may not have been completely generalizable to the current study group.
Fourth, we used methods similar to those proposed by Newell et al. [44] to estimate the length of effect for the benefits of chiropractic care in the current study. However, the cited rate of reoccurrence [44] was based on a study involving patients with acute back pain symptoms. [29] Moreover, there are limitations to assuming that the benefit from chiropractic care will be the same for every patient. The majority of CHC patients in the current study presented with chronic back pain symptoms, which may have resulted in an over-estimation of the length of effect of chiropractic care for these patients. Furthermore, it was assumed that individual patients’ baseline QALYs would not have changed without chiropractic treatment. The follow-up period was also less than ideal as a follow-up of one to two years is more commonly recommended for spine pain patients. [45] Although the majority of patients in the current study at baseline presented with chronic and persistent back pain, those with acute pain may have been more likely to recover regardless of treatment, [29, 44] thereby also contributing to an inflated benefit of the chiropractic service.
Finally, for this study we estimated primary care provider visit utilization from the literature as these rates were not measured in the original study. [16] Although these utilization rates were not directly measured for the current study they may still have been an accurate proxy as they were obtained from chronic back pain patient populations who were similar in many respects to the current study sample. Nevertheless, other health care utilization measured previously [16] was also conducted using patient-reported questionnaires. The non-utilization of primary care services reported by 77% of patients from that study was not validated (e.g. with data from electronic medical charts) and therefore could have been subject to measurement bias.
Conclusion
This study evaluated the cost-utility of chiropractic integration for low back pain services within a primary care CHC setting from the perspective of the healthcare institution. Among the subjects followed in this study, the addition of chiropractic care to usual medical care was associated with improved outcomes at a reasonable cost. These outcomes, along with the potential cost savings of such integration, may have important implications for healthcare institutions and their patients, as well as for policy decision-makers and other health stakeholders. Future comparative cost and effectiveness studies with control of confounding are nevertheless needed to evaluate the impact of chiropractic care with or without usual medical care in these settings.
Appendix Files
Appendix 1 Comparison of reported levels within baseline EQ-5D dimensions of responders (n = 45) and non-responders (n = 50)
Appendix 2 Quality-adjusted life years gained and associated potential cost savings to the healthcare institution per individual patient with chiropractic care.
(A) Worst case scenario.
(B) Best case scenario.
QALY = quality-adjusted life yearDisclaimer:
PCE is supported by research grants from McMaster University and the NCMIC Foundation for graduate studies. The other authors have no disclaimers, competing interests, or sources of support or funding to report in the preparation of this manuscript.
References:
Bronfort G Haas M Evans RL et al.
Efficacy of Spinal Manipulation and Mobilization for Low Back Pain and Neck Pain:
A Systematic Review and Best Evidence Synthesis
Spine J (N American Spine Soc) 2004 (May); 4 (3): 335–356Bronfort G, Haas M, Evans R, Leiniger B, Triano J.
Effectiveness of Manual Therapies: The UK Evidence Report
Chiropractic & Osteopathy 2010 (Feb 25); 18 (1): 3Coulter ID, Crawford C, Hurwitz EL, Vernon H, Khorsan R, Suttorp Booth M, Herman PM.
Manipulation and Mobilization for Treating Chronic Low Back Pain:
A Systematic Review and Meta-analysis
Spine J. 2018 (May); 18 (5): 866–879Goertz CM, Long CR, Hondras MA, Petri R, Delgado R, Lawrence DJ, et al.
Adding Chiropractic Manipulative Therapy to Standard Medical Care
for Patients with Acute Low Back Pain: Results of a Pragmatic
Randomized Comparative Effectiveness Study
Spine (Phila Pa 1976). 2013 (Apr 15); 38 (8): 627–634Goertz CM, Long CR, Vining RD, Pohlman KA, Walter J, Coulter I.
Effect of Usual Medical Care Plus Chiropractic Care vs Usual Medical Care
Alone on Pain and Disability Among US Service Members With
Low Back Pain. A Comparative Effectiveness Clinical Trial
JAMA Network Open. 2018 (May 18); 1 (1): e180105 NCT01692275Houweling, TA, Braga, AV, Hausheer, T, Vogelsang, M, Peterson, C, and Humphreys, BK.
First-Contact Care With a Medical vs Chiropractic Provider After Consultation With
a Swiss Telemedicine Provider: Comparison of Outcomes, Patient Satisfaction, and
Health Care Costs in Spinal, Hip, and Shoulder Pain Patients
J Manipulative Physiol Ther. 2015 (Sep); 38 (7): 477–483Fritz JM, Kim J, Dorius J.
Importance of the Type of Provider Seen to Begin Health Care for a New Episode
Low Back Pain: Associations with Future Utilization and Costs
J Eval Clin Pract. 2016 (Apr); 22 (2): 247–252Horn ME, George SZ, Fritz JM.
Influence of Initial Provider on Health Care Utilization in Patients Seeking Care for Neck Pain
Mayo Clin Proc Innov Qual Outcomes. 2017 (Oct 19); 1 (3): 226–233Manga, P.
Economic Case for the Integration of Chiropractic Services into the Health Care System
J Manipulative Physiol Ther 2000 (Feb); 23 (2): 118–122Blanchette M, Stochkendahl M., Da Silva RB, et al.
Effectiveness and Economic Evaluation of Chiropractic Care for the Treatment of Low Back Pain:
A Systematic Review of Pragmatic Studies
PLoS One. 2016 (Aug 3); 11 (8): e0160037Bath B, Trask C, McCrosky J, Lawson J.
A biopsychosocial profile of adult Canadians with and without chronic back disorders:
a population-based analysis of the 2009–2010 Canadian Community Health Surveys.
Biomed Res Int. 2014;2014 919621Community Health Centres.
Toronto, Ontario, Canada: Ontario Ministry of Health and Long-Term Care; 2019.
[Accessed March 19, 2019]. Available at:
https://www.ontario.ca/page/communityhealth-centresGlazier RH, Zagorski BM, Rayner J. ICES
Investigative Report. Toronto: Institute for Clinical Evaluative Sciences; 2012.
Comparison of primary care models in Ontario by demographics,
case mix and emergency department use, 2008/09 to 2009/10Garner MJ, Aker P, Balon J, Birmingham M, Moher D, Keenan D, et al.
Chiropractic Care of Musculoskeletal Disorders in a Unique Population
Within Canadian Community Health Centers
J Manipulative Physiol Ther 2007 (Mar); 30 (3): 165–170Passmore SR, Toth A, Kanavosky J, Olin G.
Initial Integration of Chiropractic Services into a Provincially Funded
Inner City Community Health Centre: A Program Description
J Can Chiropr Assoc 2015 (Dec); 59 (4): 363–372Emary PC, Brown AL, Cameron DF, Pessoa AF, Bolton JE.
Management of Back Pain-related Disorders in a Community With Limited Access
to Health Care Services: A Description of Integration
of Chiropractors as Service Providers
J Manipulative Physiol Ther. 2017 (Nov); 40 (9): 635–642Final Report.
Toronto, Ontario, Canada: Centre for Effective Practice; Mar 31, 2017.
Primary Care Low Back Pain Pilot EvaluationFrench SD, Beliveau PJH, Bruno P, Passmore SR, Hayden JA, Srbely J, et al.
Research Priorities of the Canadian Chiropractic Profession:
A Consensus Study Using a Modified Delphi Technique
Chiropractic & Manual Therapies 2017 (Dec 12); 25: 38Langs. Cambridge:
Langs Community Health Centre; 2019. [Accessed February 25, 2019]. Available at:
https://www.langs.org/programsservices/health/community-health-centreDrummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW.
Methods for the Economic Evaluation of Health Care Programmes. 4th ed.
Oxford; Oxford University Press; 2015Globe, G, Farabaugh, RJ, Hawk, C et al.
Clinical Practice Guideline: Chiropractic Care for Low Back Pain
J Manipulative Physiol Ther. 2016 (Jan); 39 (1): 1–22Bolton JE, Breen A.
The Bournemouth Questionnaire: A Short-form Comprehensive Outcome Measure.
I. Psychometric Properties in Back Pain Patients
J Manipulative Physiol Ther 1999 (Oct); 22 (8): 503-510Dunn KM. Croft PR.
Classification of Low Back Pain in Primary Care: Using "Bothersomeness"
to Identify the Most Severe Cases
Spine (Phila Pa 1976). 2005 (Aug 15); 30 (16): 1887–1892Field J, Newell D.
Relationship Between STarT Back Screening Tool and Prognosis
for Low Back Pain Patients Receiving Spinal Manipulative Therapy
Chiropractic & Manual Therapies 2012 (Jun 12); 20 (1): 17EuroQol Group.
EuroQol—A new facility for the measurement of health-related quality of life.
Health Policy. 1990;16(3):199–208EuroQol Research Foundation.
EQ-5D-3L User Guide. 2018. Available from:
https://euroqol.org/publications/user-guidesBansback N, Tsuchiya A, Brazier J, Anis A.
Canadian valuation of EQ-5D health states:
preliminary value set and considerations for future valuation studies.
PLoS One. 2012;7(2):e31115Devlin NJ, Appleby J.
Getting the Most out of PROMS: Putting Health Outcomes at the Heart of NHS Decision-making
London: The King’s Fund; 2010Stanton TR, Henschke N, Maher CG, Refshauge KM, Latimer J, McAuley JH.
After an episode of acute low back pain, recurrence is unpredictable and not as common as previously thought.
Spine. 2008;33(26):2923–2928Devlin NJ, Parkin D, Browne J.
Patient-reported outcome measures in the NHS: new methods for analysing and reporting EQ-5D data.
Health Econ. 2010;19(8):886–905Carey TS, Freburger JK, Holmes GM, Castel L, Darter J, Agans R, Kalsbeek W, Jackman A.
A long way to go: practice patterns and evidence in chronic low back pain care.
Spine. 2009;34(7):718–724Hong J, Reed C, Novick D, Happich M.
Costs associated with treatment of chronic low back pain: an analysis of the UK General Practice Research Database.
Spine. 2013;38(1):75–82Gurden M, Morelli M, Sharp G, Baker K, Betts N, Bolton J.
Evaluation of a general practitioner referral service for manual treatment of back and neck pain.
Prim Health Care Res Dev. 2012;13(3):204–210Laupacis A, Feeny D, Detsky AS, Tugwell PX.
How attractive does a new technology have to be to warrant adoption and utilization?
Tentative guidelines for using clinical and economic evaluations.
CMAJ. 1992;146(4):473–481Gafni A, Birch S.
Guidelines for the adoption of new technologies: a prescription for uncontrolled growth
in expenditures and how to avoid the problem.
CMAJ. 1993;148(6):913–917van der Velde G, Hogg-Johnson S, Bayoumi AM, Cassidy JD, Côté P.
Identifying the best treatment among common nonsurgical neck pain treatments: a decision analysis.
Spine. 2008;33(4 Suppl):S184–S191Luijsterburg PAJ, Verhagen AP, Ostelo RWJG, van Os TAG, Peul WC, Koes BW.
Effectiveness of conservative treatments for the lumbosacroal radicular syndrome: a systematic review.
Eur Spine J. 2007;16(7):881–899Jacobs WCH, van Tulder M, Arts M, Rubinstein SM, van Middelkoop M, Ostelo R.
Surgery versus conservative management of sciatica due to a lumbar herniated disc: a systematic review.
Eur Spine J. 2011;20(4):513–522Dagenais S, Roffey DM, Wai EK, Haldeman S, Caro J.
Can cost utility evaluations inform decision making about interventions for low back pain?
Spine J. 2009;9(11):944–957Mior S, Gamble B, Barnsley J, Côté P, Côté E.
Changes in Primary Care Physician's Management of Low Back Pain
in a Model of Interprofessional Collaborative Care:
An Uncontrolled Before-After Study
Chiropractic & Manual Therapies 2013 (Feb 1); 21 (1): 6Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, Hoy D, Karppinen J et al.
What Low Back Pain Is and Why We Need to Pay Attention
Lancet. 2018 (Jun 9); 391 (10137): 2356–2367
This is the second of 4 articles in the remarkable Lancet Series on Low Back PainMehrez A, Gafni A.
Quality-adjusted life years, utility theory, and healthy-years equivalents.
Med Decis Making. 1989;9(2):142–149Gafni A.
Willingness-to-pay as a measure of benefits. Relevant questions in the context of public decision making
about health care programs.
Med Care. 1991;29(12):1246–1252Newell D, Diment E, Bolton JE.
An electronic patient-reported outcome measures system in UK chiropractic practices:
a feasibility study of routine collection of outcomes and costs.
J Manipulative Physiol Ther. 2016;39(1):31–41Kongsted A, Kent P, Axen I, Downie AS, Dunn KM.
What Have We Learned From Ten Years of Trajectory Research in Low Back Pain?
BMC Musculoskelet Disord. 2016 (May 21); 17 (1): 220
Return to COST-EFFECTIVENESS
Return to INTEGRATED HEALTH CARE
Return to INITIAL PROVIDER/FIRST CONTACT
Since 10-06-2019


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |